Systems of care worldwide are attempting to meet the challenge of providing comprehensive, early-intervention services for individuals experiencing a first psychotic episode in the face of mounting evidence of the effectiveness of such interventions (
1). Many countries with national health care systems establish first-episode psychosis (FEP) teams to provide a comprehensive, intense array of services to persons recently diagnosed as having schizophrenia or other psychotic disorders (
2). Although models of FEP treatment vary, effectiveness studies in Australia, the United Kingdom, Hong Kong, and Italy have found that early-intervention programs had costs similar to or less than costs for usual care but yielded greater improvements in functioning and lower rates of inpatient hospitalization (
1–
4).
Most FEP models implemented outside the United States are in countries with state-funded national health programs. The fragmentation of the U.S. health care system poses particular challenges for FEP and early-intervention programs. Many implementation and financing strategies are possible (
5), such as using fully or partially dedicated FEP teams, training a team of clinicians with other responsibilities to provide FEP treatment as needed to their clients, and using a hub-and-spoke model in which practitioners trained in FEP treatment travel to clients in a designated area (
6). However, it is unlikely that a single payer will support the comprehensive activities called for in FEP programs, and coordination across systems of care can be difficult.
To stimulate and study the impact of early intervention for psychosis in the United States, the National Institute of Mental Health established the Recovery After Initial Schizophrenia Episode (RAISE) initiative (
7). The New York State Office of Mental Health (OMH) is a partner in the RAISE Connection program, which established fully dedicated multidisciplinary FEP teams that provide individuals experiencing a first psychotic episode with roughly two years of treatment services tailored to meet each person’s needs, including help with illness management, medication, supported employment and education, family psychoeducation, and substance abuse treatment. As an outgrowth of its participation in the RAISE initiative, OMH is exploring how to scale up early-intervention services for individuals across the state who are experiencing early psychosis. This column describes the New York State FEP projection tool: how it was developed, how it works, how it is being used in New York State, and how it can be applied in other settings.
Tool for estimating FEP resource needs
Development
A core planning issue was to estimate the number of FEP teams that would be needed, both statewide and in various urban and rural areas. To our knowledge, only one decision support tool had been developed for early intervention in psychosis (
8); however, this tool was developed on the basis of cost simulations in the United Kingdom and is not easily applicable to other treatment settings. Thus we used a state-academic partnership to facilitate the planning of this initiative through the development of an interactive planning tool.
The estimate of number of teams needed is driven by many unknowns, for example, the number of clients served by a team, the average duration of time an individual is served, the percentage of individuals with FEP who are identified and agree to receive services, and estimates of the incidence of FEP, which vary widely. Therefore, our goal was to create a user-friendly modeling tool that would allow the user to input various estimates for these variables and see the impact on the estimate of number of teams needed statewide, how large an area’s population needed to be to have enough incident cases each year to support an FEP team, and what the costs of operating such teams would be under various staffing models.
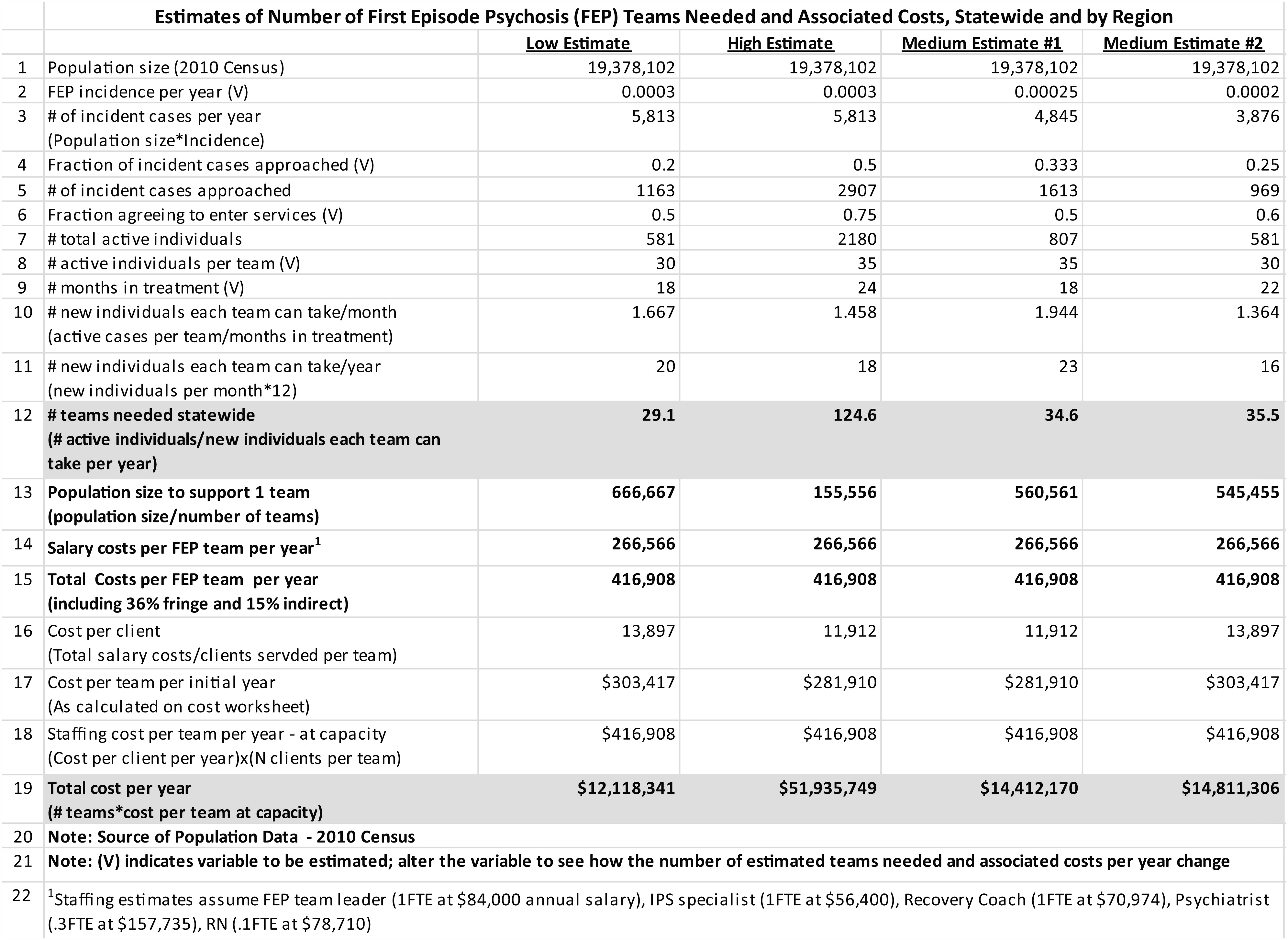
Figure 1 presents an example of the tool in use. [The full, interactive Excel-based tool is available as an online
data supplement.]
The tool
The first page of the tool shows step-by-step calculations for determining the number of fully dedicated FEP teams needed to support a given service area and the total cost per year to staff those teams. Fields that are user-modifiable variables are noted with “(V).” The calculations begin with the population in the service area (in this case, the state of New York) from the most recent U.S. Census (line 1). The estimate of FEP incidence per year (population multiplied by the incidence rate) is based on published incidence rates of 20 to 30 cases per 100,000 population (line 2) (
9,
10). Even under ideal conditions, outreach efforts would be unlikely to reach all incident cases; therefore, estimates of the percentage of cases that can be contacted and the estimated enrollment rate among those contacted are presented in lines 4 and 6. These variables combine to generate the estimated total number of new clients enrolled per year in the service area (line 7).
The number of slots opening per team per month is calculated by dividing the number of active cases per team by the average number of months in treatment (line 10, annualized in line 11). The number of teams needed in the geographic area is calculated by dividing the total number of active clients by the number of new individuals each team can take per year (line 12). The tool then estimates the population size needed to support one team (line 13). The tool also estimates the total annual costs per year (line 15) on the basis of current salary levels in New York City. Total program costs per year for a full-time team (line 19) are calculated by multiplying the annual cost per team by the number of teams needed.
The tool allows policy makers to compare costs and treatment team sizes by varying the estimates of inputs. The example shown in
Figure 1 presents a high, a low, and two medium estimates under varying assumptions.
The tool also estimates the number of teams needed for smaller geographic areas in the state: selected counties and cities and the five regions into which OMH divides the state. [These figures are illustrated in the second tab of the interactive tool available in the
online supplement.] The formulas in each cell are linked to the calculations in the first tab and are automatically updated when any variable changes. Costs for the initial year are the most difficult to automate, because they are dependent on the number of slots opening per team per month and the number of clients a team can support. The calculation is illustrated in tab 3 and automatically populates to the first tab. In addition, because the majority of persons targeted by FEP teams are young adults, we have estimated the percentage of the population age 15–35 in each geographic area (tab 4). A list of additional expenses that have not been calculated but that may be incurred by FEP teams is included in tab 5 [see tabs in the
online supplement].
How OMH uses the tool
The tool is being used by OMH in the design of its statewide FEP initiative. The tool provides OMH with estimates of how many teams a given geographic area can support. The tool estimates the total staffing costs to cover the full state or a smaller geographic region under varying assumptions; it also estimates the number of teams that could be supported by a fixed amount of resources. For example, the areas of greatest need are in Brooklyn, Queens, and Manhattan and several smaller cities in the state also have a population base large enough to support a fully dedicated team.
By determining the size of the population needed to support a fully dedicated team (about 500,000 under the medium estimates in
Figures 1), administrators can identify areas with a sufficient population within a reasonable travel distance to base a team. Similarly, any entity bidding on a partially or fully capitated contract to provide such services can estimate the number of individuals with FEP for which it would be responsible. In addition to estimating costs, information from the tool can be useful in outreach and program planning. For example, the tool estimates the number of new clients that teams can take each year under varying user-defined assumptions (line 11). Program officials can then modify their outreach strategies accordingly, to minimize the risk of generating waiting lists or having excess staffing, and can project how more or less thorough strategies would affect program size and costs by modifying the variable representing the estimated fraction of incident cases seeking services (line 6).
Applicability to other settings
The tool can be adapted easily for use in other treatment settings. Variables can be added or removed—for example, to include additional cost categories or to adapt to other FEP treatment models, such as the clinic model or hub-and-spoke model. The tool can also be used to estimate the number needed and costs of other treatment programs (for example, the number of assertive community treatment teams or the number of Head Start programs) by modifying the relevant variables, such as incidence and treatment team costs.
The tool has limitations. The estimates of costs and resources needed are only as strong as the assumptions that underlie them. On the other hand, part of the utility of the tool derives from how helpful it is to “turn one estimating dial,” given the large uncertainty associated with some of the variables to be estimated (such as the incidence estimate) and to see how turning the dial affects the number of teams needed and other variables. By dial spinning, one can see that, for example, the number of months an average person stays on a team’s case load has much less impact on costs than does the estimate of incidence or enrollment.
Limited information about estimating costs of FEP teams is available to policy makers, particularly in U.S. health care settings. Therefore, this tool provides a useful means of estimating the need for FEP teams in one large, geographically diverse state, and it is readily adaptable to other settings and program types.
Acknowledgments and disclosures
Work on this project was supported by the New York State OMH Policy Scholars Program via funds from OMH to the Division of Mental Health Services and Policy Research, New York State Psychiatric Institute, and the Department of Psychiatry, Columbia University. The authors thank Norman Brier for support in tool development for OMH and for helpful comments on the manuscript.
The authors report no competing interests.