The number of mental health courts (MHCs) has increased from one or two in 1997 to approximately 350 today (
1). These problem-solving courts have become a major response to the burgeoning number of people with serious mental illness in the criminal justice system. Upwards of two million people with serious mental illness are booked into U.S. jails each year, and rates of serious mental illness in U.S. correctional facilities are three to four times the rates in the general population (
2). Effective and efficient alternatives to incarceration are clearly needed. Drug courts are the most visible alternative, with 2,459 in operation in 2009 (
3). More recently, Veterans Treatment Courts have grown from one in 2009 to approximately 200 today (
4).
These alternatives to incarceration attempt to link justice-involved persons with mental illness to community-based services, usually with continuing judicial supervision. Mental health courts identify eligible participants, enroll them voluntarily, and develop treatment plans that participants agree to follow. If participants do not adhere to the conditions, the criminal court can reinstate their charges. For those who are already on probation, having pleaded guilty to earlier charges, the criminal court can charge them with violating the terms of their probation. The logic model underpinning these courts is that if defendants adhere to the services provided, their symptoms will be reduced, their level of functioning and quality of life will improve, and they will be arrested less often and use fewer jail days. If this logic is correct, mental health courts would advance both public health and public safety goals.
First-generation research on MHCs was dominated by case studies. Quite consistently, these studies found reduced recidivism after enrollment compared with the year before the target arrest (
5–
9). Few of these early studies reported on public health outcomes, but those that did found modest improvements (
10–
12). To date, the only multisite study to focus on public safety outcomes also found positive results (
13,
14). The study reported here advances the evidence base by comparing data for detainees before and after MHC enrollment with data for a comparison group of detainees who were not enrolled in an MHC but who received jail-based psychiatric services in the same cities as enrolled participants.
Only two previous studies have examined the costs of MHCs. These studies addressed the degree to which courts shift costs from the criminal justice system to the behavioral health system or result in net cost savings to taxpayers. The cost question is an especially important policy issue because supporters of MHCs argue their value both on humane grounds—that MHCs are a better health option for the participants—and on cost-effectiveness grounds—that MHCs can more effectively manage this population and more efficiently arrange to meet their treatment needs, resulting in cost savings for taxpayers. The RAND study on the Allegheny County (Pittsburgh, Pennsylvania) mental health court found that for the first 18 months there was cost shifting from the criminal justice system to the mental health system and that overall total costs for MHC participants were higher (
15). From 18 to 24 months, total costs for the two systems were less than for a “counterfactual” comparison group, which was assumed to have been convicted at the time the MHC defendants were enrolled. The San Francisco Behavioral Health Court (BHC) study found a similar pattern over a three-year follow-up period (
16). In year 1, for every $2.32 invested in the BHC, there was $1.00 saved in criminal justice costs. In year 2, for every $2.64 invested, there was a $1.00 criminal justice savings. For year 3, for every $.90 invested, there was a $1.00 criminal justice savings.
Our work advances prior scholarship by reporting data from three sites, with a comparison group from each site, and for a long pre- and postenrollment period—three years before and three years after enrollment in the MHCs. To better target defendants for MHC enrollment, we were interested in comparative costs and net taxpayer savings overall and for subgroups. Second-generation research on drug courts has found that those courts achieved only minimal reductions in recidivism and cost for lower-risk defendants (
17); however, for higher-risk clients, recidivism rates were 8–26 percentage points less than for other justice system responses, with substantial cost savings (
3). The as-yet unanswered question is whether MHCs produce the same or better results. Specifically, our main research question was whether there are any differences in costs for MHC participants and comparison group members for three years after their target arrest.
Methods
This study is the final phase of the MacArthur Mental Health Court Study, a multisite, case-control investigation that followed 447 MHC participants and 600 treatment-as-usual (comparison) defendants in four jurisdictions (Hennepin County–Minneapolis, Minnesota; Marion County–Indianapolis, Indiana; San Francisco; and Santa Clara County–San Jose, California) (
13,
18,
19). The cost data reported here were not available for Santa Clara County. The MHC and comparison groups were matched on diagnosis, charges, and gender. All participants were interviewed at baseline—either at MHC entry or in jail shortly after their target arrest. At the six-month follow-up, 70% of the sample (N=497) were reinterviewed. We also obtained permission from participants to access data on their criminal histories and arrests, incarcerations, and behavioral health treatment during the follow-up period. The study design has been described in more detail elsewhere (
13,
18,
19). All instruments, procedures, and approach scripts were approved by a federally assured institutional review board (IRB) and by local IRBs when required. On the basis of available utilization data, the sample included 296 MHC participants and 386 comparison jail detainees.
We calculated costs for the three years before the target arrest (years 1 to 3), and the three years after release from the target arrest incarceration (years 4 to 6). Service use was measured by Medicaid-reimbursable services at each site by using county and state administrative databases. Criminal justice contacts were determined by Federal Bureau of Investigation rap sheets obtained for all study participants. MHC records were abstracted at each site to measure all court hearings. For each service event, each arrest, and each MHC appearance, a cost was attached from which total costs in each category were calculated.
Unit service costs were estimated from two sources. When possible, we used the Medical Expenditure Panel Survey (MEPS), a two-year panel survey conducted by the Agency for Healthcare Research and Quality (AHRQ). These data are publicly available from the AHRQ Web site (
MEPS.ahrq.gov). In 2006, MEPS recorded information for slightly more than 34,000 individuals in two distinct panels. These individuals are a random sample of the noninstitutionalized population, with oversampling of minority populations and accompanying weights. In MEPS, panel members are interviewed about their contacts with the health system (for example, hospital, office, emergency room, and prescription events). These events are then cross-referenced with medical provider records to establish the actual claim filed and total payments, as well as the source of the funds. We used MEPS event files to calculate the average payment for elements of treatment.
Many MHC clients receive services for some independent evaluations or nonmedical support services. The MEPS data are less reliable for these types of services. In these instances, we obtained cost estimates for ancillary services associated with mental health support in the community from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) (
20). The CATIE effectiveness trials included a population similar to the MEPS. All unit costs were adjusted to the 2008 Consumer Price Index by using the urban consumer yearly averages available from the Bureau of Labor Statistics.
The criminal justice costs came from three sources. McCollister and colleagues (
21) provided jail and prison costs. The New Hampshire study by Clark and colleagues (
22) was used to estimate arrest, transportation and booking costs. The court per-hearing costs were taken from Lindberg’s (
16) 2009 San Francisco study.
All costs were also calculated separately for each of the six study years: three years before and three years after the target arrest. For participants with very long target arrest periods—that is, those who were detained in jail for many months before adjudication—we extrapolated three years after the target arrest. This extrapolation was necessary for the overall three-year period after the target arrest but not for the year-by-year information.
The participants in the MHC and comparison groups were not randomly assigned, and it is possible that despite attempts to match them on gender and criminal charge, some differences remained in demographic variables, diagnoses, and other personal characteristics. We tested for differences between the MHC and comparison groups for several demographic, diagnostic, and behavioral health variables: age, gender, race-ethnicity, marital status, diagnosis, prior hospitalizations, alcohol use, and drug use. Several statistically significant differences were noted. The MHC group had a larger proportion of participants with diagnoses of schizophrenia than the comparison group (45% versus 18%), a smaller proportion with diagnoses of depression (16% versus 50%), and a larger proportion with diagnoses of bipolar disorder (30% versus 20%). The MHC group also had a smaller proportion of participants with at least one day of drug use in the past 30 days (48% versus 66%) and with at least one day of alcohol use (49% versus 66%). The MHC group had a larger proportion of participants with prior psychiatric hospitalizations (83% versus 67%). Differences in the other investigated variables were not statistically significant.
To balance the MHC and comparison groups, we employed the coarsened exact matching (CEM) algorithm (
23). An exact matching method may leave some intervention cases without a match in the comparison group.
We included the costs for years 1–3 in the exact matching procedure because our main research question required comparison of costs. Therefore, the MHC and comparison groups were matched on five variables: prior cost (years 1–3), diagnosis, alcohol use in the past 30 days, drug use in the past 30 days, and prior psychiatric hospitalizations, obviating any biases from the distribution differences observed.
Results
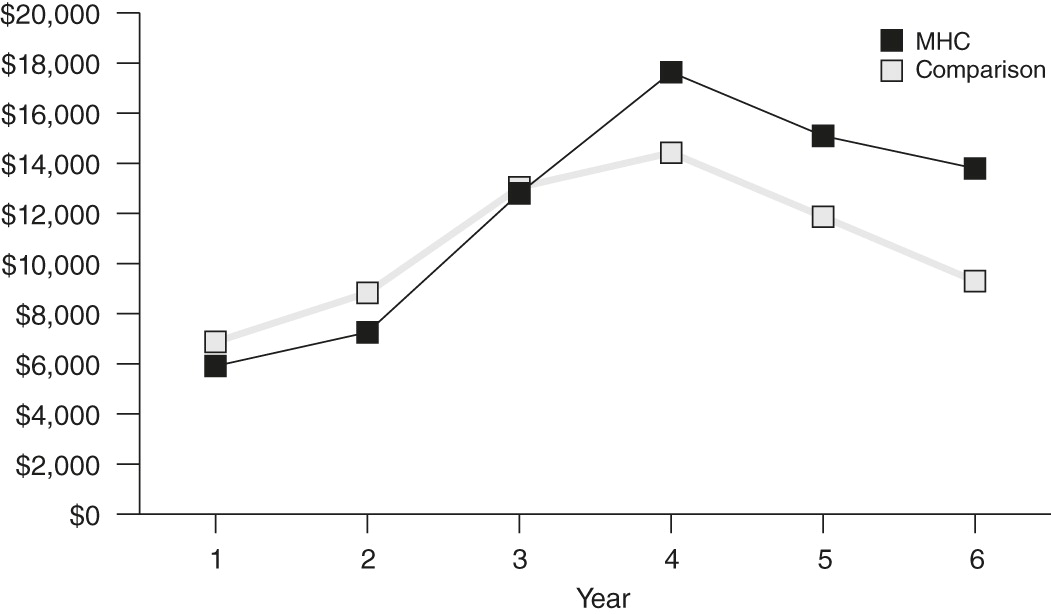
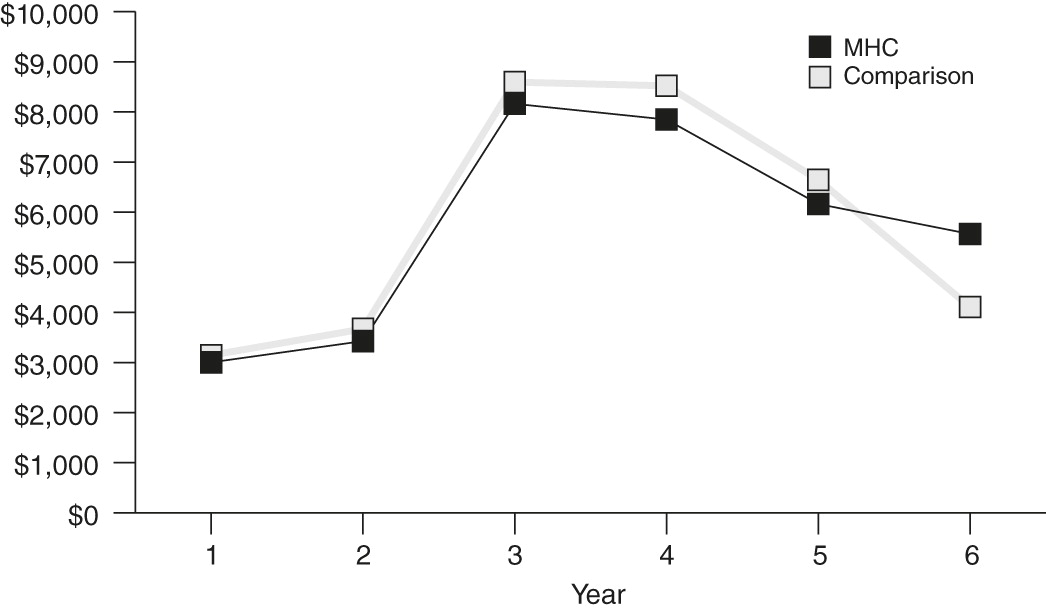
Figures 1,
2, and
3 present the total costs, the criminal justice costs, and the treatment costs, respectively, for the three years before the target arrest and the three years after release to the community from the target arrest incarceration. All data presented are CEM weighted.
Data for the period before the target arrest showed a sharply upward trend for both total costs and criminal justice costs, peaking in the year of the target arrest. Total costs on average for the MHC participants jumped from about $6,000 in year 1 to about $13,000 in year 3 (217% increase) immediately before the target arrest, and criminal justice costs jumped from $3,000 in year 1 to about $8,000 in year 3 (267% increase). Of note, about 86% of the increase in average criminal justice costs occurred in the year immediately before the target arrest. Behavioral health treatment costs, in contrast, were more attenuated in the period before the target arrest, rising from about $2,500 in year 1 to $3,600 in year 3 (44% increase). These escalating costs undoubtedly helped bring participants to the attention of the MHC program.
MHC participants had substantially higher total costs after enrollment for all three years after the target arrest, a difference of approximately $4,000 per year more than for the comparison group. The source of this difference is also clear. The additional costs resulted from much higher treatment costs (about $6,000 higher than the comparison group in year 4, $5,000 in year 5, and $4,500 in year 6). The higher treatment costs were not offset by lower criminal justice costs, which were slightly lower for MHC participants than for the comparison group in years 4 and 5 and slightly higher in year 6.
The next question we examined was whether we could identify any subgroup of MHC participants who were particularly high-cost participants. This question became particularly important when we determined that there were very large differences by study site in the proportion of MHC participants who had reduced total costs across the three-year follow-up compared with their costs in the years before the target arrest. In Hennepin County (Minneapolis), 61% of MHC participants had reduced costs after the target arrest, compared with 40% in Marion County (Indianapolis) and only 20% in San Francisco. The difference was computed from the actual unweighted costs for the period after the target arrest minus the costs for the period before the target arrest and any decrease—that is, if the cost in the post period was greater than the cost in the pre period, it was recoded as 1 and the rest were recoded as 0 for the same or increasing cost. Chi square tests were applied to assess significance.
Among all the variables, only two were significantly and strongly related (Spearman’s rho >.2) to having increased costs in the period after the target arrest compared with the period before the target arrest: a greater number of arrest incarceration days in the period before the target arrest and a diagnosis of a co-occurring substance use disorder. Total costs decreased after the target arrest for only 33% of those with a co-occurring substance use disorder, compared with 55% of those without a co-occurring substance use disorder. Thus MHC participants with more prior jail days had greater total costs in the period after the target arrest than did MHC participants with a co-occurring substance use disorder.
Another question that emerged from these cost data was whether the MHC participant costs were unduly influenced by a few outliers. In the CEM technique, outliers are dropped from the analyses because they do not have a match. Thus they have no influence on the final results. To further ensure that there was no outlier problem, we examined the unweighted data before the CEM technique was used. In the three follow-up years, we noted two huge outliers, with total costs of $239,253 and $436,496, compared with average total costs of $42,807. Excluding these two cases reduced the mean cost to $41,940, which again demonstrated that there was no outlier problem.
Discussion
The findings presented here call into question some of the assumptions of MHC advocates who argue that participation in these courts will result in more cost-effective and efficient interventions for jail detainees who have a serious mental illness. Our findings suggest that broad claims of cost savings over time for MHCs as they currently operate are not supportable. That is not to say that MHCs are not effective in reducing subsequent arrests and subsequent jail days. They are. However, the added treatment costs exceed for many participants the criminal justice cost savings.
The three MHCs studied here exhibited cost patterns that are inconsistent with those reported for the Allegheny County MHC (
15) and the San Francisco BHC (
16). In those studies, after 18 to 24 months the total criminal justice and mental health treatment costs of the MHC participants were lower than those of the statistically generated comparison group. When we analyzed three years of data from our three study sites for the period after the target arrest, we found that the MHC participants had higher total costs than a jail comparison group during each of the three years. Our data also are clear that MHC participants who were the most costly were those with co-occurring substance use disorders and more incarceration days before MHC enrollment.
One unexpected finding was the length of time from the target arrest to enrollment in the MHC, which resulted from two major dynamics. First, the MHC was sometimes a court of last resort after the participant had failed in a drug court or in some other type of specialty treatment court. Second, before the participant could be enrolled in the MHC and released from incarceration (that is, when the three-year follow-up began) a fully implementable treatment plan needed to be in place. The housing piece of the treatment plan was often the most difficult feature to implement and resulted in extensions of the target arrest incarceration. Neither of these dynamics was relevant to the comparison group.
How this extended period might have affected the cost analyses is unclear. Both the MHC group and the comparison group were getting treatment while incarcerated after their target arrest. They would have been getting treatment in the same jail by the same treatment staff, so there would not have been any systematic differences in that period except that the MHC group could have been incarcerated longer. Our belief is that the delayed release of the MHC group did not have a substantial impact on our results.
Conclusions
Ultimately, it is not clear what conclusions to draw from these results. We would argue that to contain costs MHCs should not exclude participants with a co-occurring substance use disorder and those with numerous prior incarcerations. It is, in fact, exactly this group that may most need MHCs and for whom MHCs may ultimately be most beneficial. As evidenced-based practices for persons with co-occurring disorders, such as integrated dual-disorder treatment, become available to MHC treatment providers, MHCs can expect not only to reduce recidivism and improve behavioral health outcomes but also to reduce taxpayer costs across both behavioral health and criminal justice systems. MHCs can target high-need, high-risk individuals as long as they can mandate the delivery of evidence-based services that have been shown to work with this justice-involved population.
The relatively unquestioned value of MHCs needs to be reexamined. These courts can be very successful, but only if they enroll defendants for whom appropriate and adequate services targeting both behavioral health and criminogenic factors are actually available. MHC personnel identify, engage, monitor, and support their participants. They do not treat them. They supervise and encourage them. They link participants to community-based services that represent the primary interventions. It is fruitless to enroll MHC participants if the community-based services appropriate to their clinical conditions are not available. The courts are conduits to services and ensure appropriate supervision while a person is under criminal justice control. There will not be total cost savings for all courts or all participants in every court unless the right people get the right services. That is the message from the cost data we have presented here.
Acknowledgments and disclosures
This research was supported by the John D. and Catherine T. MacArthur Foundation’s Research Network on Mandated Community Treatment directed by John Monahan, Ph.D.
The authors report no competing interests.