Hospital readmissions account for a large proportion of health care spending in the United States, including over $17 billion of Medicare costs annually (
1). In an effort to curb rising health care costs and simultaneously improve quality of care, the Centers for Medicare and Medicaid Services (CMS) implemented a new policy as part of the Affordable Care Act that ties levels of reimbursement for health care to hospital readmission rates (
2). Beginning in fiscal year 2013 (October 1, 2012), hospitals with excessive all-cause rehospitalizations within 30 days of discharge from an index admission for three general medical conditions are penalized by the CMS by reduction in payment for health care services (
3,
4). The three conditions—heart failure (HF), acute myocardial infarction (AMI), and pneumonia—were chosen because they are expensive to treat, are common, and frequently result in readmission (
5–
8). However, over time, the list of conditions subject to the CMS readmission payment policy will likely expand to include all diagnoses (
9).
Because of the current policy and the possibility of impending expansion to other conditions, 30-day hospital readmissions are a major concern for hospitals across the nation (
10). Thus developing effective interventions to reduce readmissions is essential to avoid penalties and to improve the quality of care. Yet a primary question remains: How should interventions be targeted to provide the greatest reduction in readmissions at the lowest cost?
Psychiatric conditions may represent an efficient place to focus interventions. Such conditions are highly comorbid with HF, AMI, and pneumonia as well as with many other chronic general medical conditions. They are known to complicate the care of those conditions. Previous studies using small, localized samples have reported varying levels of association between comorbid mental illnesses and 30-day hospital readmissions for general medical conditions, including the conditions targeted by CMS policy (
11–
13). For example, a recent study of 84 patients with congestive heart failure found that both cognitive impairment and a history of mental health conditions were associated with higher rates of 30-day readmissions (
12). On the other hand, a single-site study of nearly 7,000 patients who were admitted to the hospital for any general medical condition showed that comorbid anxiety and substance use disorders were associated with fewer 30-day all-cause readmissions. There was no relationship between other comorbid psychiatric illnesses and risk of all-cause readmission (
11). These two single-site studies reported conflicting results. Thus the extent to which psychiatric comorbidities influence the likelihood of readmission for HF, AMI, and pneumonia is unclear.
To address this gap in knowledge, this collaborative, multisite study investigated whether comorbid mental illnesses (in combination and by diagnostic category) influenced 30-day hospital readmission rates in a national sample of 11 large health care delivery systems, including more than 160,000 index hospitalizations for HF, AMI, and pneumonia.
Methods
This study was conducted by researchers at the Mental Health Research Network (MHRN), a consortium of 11 large health care systems with affiliated health insurance plans. These systems are part of the larger HMO Research Network, which includes 17 U.S.-based health system members. The MHRN systems serve over 11 million individuals across 11 states with diverse populations. These sites and their primary locations include Group Health Cooperative (Washington), Harvard Pilgrim Health Care (Massachusetts), HealthPartners (Minnesota), Henry Ford Health System (Michigan), Kaiser Permanente Colorado, Kaiser Permanente Georgia, Kaiser Permanente Hawaii, Kaiser Permanente Northern California, Kaiser Permanente Northwest (Oregon), Kaiser Permanente Southern California, and Scott & White Healthcare (Texas). Institutional review boards at each site approved data use for this project.
Each participating site maintains an HMO Research Network Virtual Data Warehouse (VDW), which consists of both electronic medical record and insurance claims data for the site’s health plan patients (
14,
15). Data on encounters, pharmacy fills, diagnoses, procedures, medical tests, demographic characteristics, costs, and other aspects of health care are organized using standardized definitions across sites and are checked for quality locally. Data for this project were extracted from the local VDW at each site by using a common programmatic code distributed across sites.
In this study, the sample included all health plan patients at the participating health systems with an index inpatient hospitalization for HF, AMI, or pneumonia between January 2009 and December 2011. Continuous enrollment in the health plan for the 12-month period prior to admission and the 30-day period after admission was required for inclusion. On average, approximately 85% of members maintain enrollment for at least 12 months, with rates ranging between 79% and 90% at different sites. Thus a portion of the population was excluded from the analysis because they were not continuously enrolled for the full period. In total, 160,169 index patient admissions met eligibility criteria for the sample.
Individuals with hospital admissions for HF, AMI, or pneumonia were identified by using the same
ICD-9 codes used by CMS to calculate admission and readmission (
2,
4,
16). We also pooled individuals with any of these conditions into a combined group. Data were extracted for individuals who had one of these conditions listed as an inpatient discharge diagnosis. Consistent with the CMS policy, each admission that occurred more than 30 days following a prior admission was counted as a new index admission. Thus some individuals had multiple index admissions and were represented in multiple disease groups.
Psychiatric comorbidities were identified by
ICD-9 codes for mental disorders (
16). Individuals were counted as having a psychiatric condition if they received the same diagnosis on at least two occasions in any setting (emergency, inpatient, or outpatient) during the 12-month period prior to and including the inpatient discharge date. For individuals with index hospital admissions in 2009, prior-year data were calculated by using 2008 data. Psychiatric conditions were grouped in the following categories: anxiety disorders (300.00–300.02, 300.21−300.24, 300.3, 309.21, 309.24, and 309.81), bipolar disorders (296.00–296.06, 296.40–296.89, and 301.13), dementia (290.xx and 780.93), depressive disorders (296.20–296.36, 300.4, 309.0, 309.28, and 311), schizophrenia-spectrum disorders (295.xx), other psychoses (297.1, 297.3, 298.8–298.9, and 301.20–301.22), and substance use disorders (alcohol or drug use disorders) (291.xx, 292.xx, 303,xx, and 305.xx). Individuals with any of these conditions were pooled together into a category labeled “any psychiatric diagnosis.”
A 30-day readmission was defined as any admission for any reason to any hospital that occurred no more than days after discharge from the initial index hospitalization for HF, AMI, or pneumonia. Following CMS policy, planned readmissions for revascularization among patients with AMI were not counted as readmissions (
3).
Demographic information on age, sex, race-ethnicity, and insurance type was available from the VDW. Estimated household income and education levels were calculated by using patient addresses and local neighborhood census data.
Statistical analyses began by aggregating descriptive characteristics of the study sample. Then, mean readmission rates for individuals with index hospitalizations for HF, AMI, and pneumonia were calculated by dividing the number of readmissions by the total number of index hospitalizations for each diagnostic subgroup. Readmission rates for the entire sample were also calculated. The sample was divided into individuals with or without a psychiatric diagnosis, and the readmission rate was calculated for each group and for individuals in each group with an index hospitalization for HF, AMI, or pneumonia. Finally, the readmission rate for individuals with an index admission for HF, AMI, or pneumonia was calculated separately for each psychiatric diagnosis. Chi square tests were used to compare rates of readmission among those with and without a psychiatric comorbidity. Odds ratios (ORs) were included to indicate the strength of association between any psychiatric comorbidity and readmission. Finally, annual trends in 30-day readmission rates between 2009 and 2011 were calculated for individuals with and without psychiatric comorbidity.
Results
As shown in
Table 1, there were 160,169 index hospitalizations for HF, AMI, or pneumonia in 2009–2011 across all 11 sites. A majority of the sample was male (53.1%), non-Hispanic white (62.1%), and over 65 years old (63.2%), and most had health care coverage through a Medicare Advantage product (67.0%). Most individuals lived in neighborhoods where the median income was at least $40,000 per year (77.0%) and less than 25% of residents were college graduates (54.0%). Overall, 55.8% (N=89,406) of the patients were admitted for HF, 21.5% (N=34,515) for AMI, and 45.2% (N=72,438) for pneumonia; 22.5% (N=36,190) of the sample were admitted at different points for more than one of these conditions. Also, 29.4% (N=47,140) of the total sample had a psychiatric condition, with depression (15.8%, N=25,301), substance use disorder (11.3%, N=18,160), and anxiety (7.1%, N=11,400) diagnosed most commonly.
Table 2 shows 30-day hospital readmission rates for individuals with index hospitalizations for HF, AMI, or pneumonia, with or without psychiatric comorbidities. All-cause readmission was most common among individuals with index hospitalizations for HF (20.1%) versus individuals with index hospitalizations for AMI (9.9%) and pneumonia (17.5%). The rate of all-cause readmission for the entire sample was 18.1%. The rate of readmission was significantly higher among individuals with a psychiatric diagnosis in the past year compared with those with no psychiatric comorbidity (21.7% versus 16.5%, χ
2=602.5, df=1, p
<.001, OR=1.4). Similarly, rates of readmission after index hospitalization for all three general medical conditions were higher among individuals with any psychiatric comorbidity compared with those with no psychiatric comorbidity (HF, 22.9% versus 19.0%, χ
2=175.2, df=1, p
<.001, OR=1.4; AMI, 12.1% versus 9.2%, χ
2=60.2, df=1, p
<.001, OR=1.4; and pneumonia, 20.2% versus 16.2%, χ
2=180.8, df=1, p
<.001, OR=1.3).
A comparison of 30-day all-cause readmissions among persons with and without psychiatric comorbidity found an increase in readmissions for all psychiatric diagnosis categories (21.7% versus 16.5%, relative risk=1.32, p<.05). Individuals with comorbid anxiety, dementia, and depression had higher rates of readmission than persons with no psychiatric comorbidity regardless of whether the index hospitalization was for HF, AMI, or pneumonia (p<.05). Schizophrenia, however, was not associated with larger proportions of readmissions by specific cause of index hospitalization (HF, AMI, or pneumonia). However, the subgroup sample size was insufficient. Bipolar and substance use disorders were not associated with increased readmissions among those who were originally admitted with AMI. Data were insufficient to test for differences in readmissions among individuals with other psychoses and an index admission for AMI.
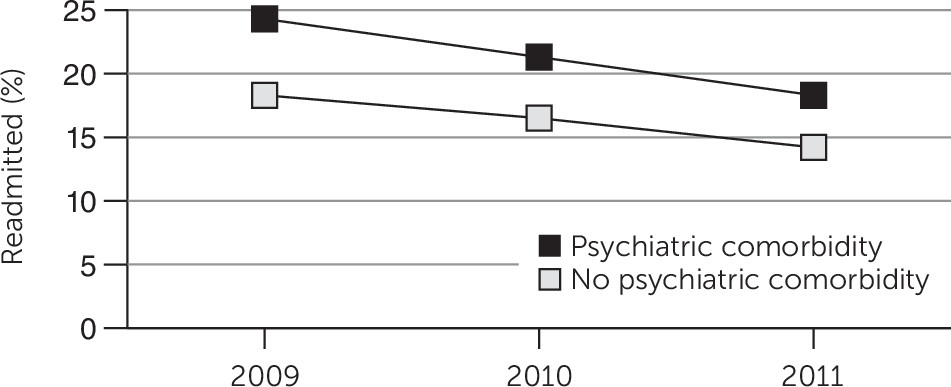
Figure 1 shows changes between 2009 and 2011 in aggregated 30-day readmission rates for individuals with and without any psychiatric comorbidity. Readmission rates for all individuals showed a downward trend over the three-year period. For those with any psychiatric diagnosis, rates fell from 24.3% in 2009 to 21.3% in 2010 and 18.3% in 2011. Similarly, for those without a mental health condition, the rate of readmission fell from 18.3% to 16.5% and 14.2% in 2009, 2010, and 2011, respectively. The annual gap in readmissions between those with and without psychiatric comorbidities converged during the study period from 6.0% in 2009 to 4.1% in 2011.
Discussion
This study represents the largest and most geographically diverse investigation of the contribution of psychiatric illness to 30-day hospital readmission rates for patients with original admissions for HF, AMI, or pneumonia in the U.S. general health care population. Previous studies of smaller, single-site samples reported varying results (
11,
12), but this study of over 160,000 patient index admissions for HF, AMI, or pneumonia found that individuals with psychiatric comorbidities in the previous year were readmitted to the hospital within 30 days from 3% to 5% more often than those without a psychiatric diagnosis. In total, findings from this study suggest that psychiatric comorbidities influence 30-day all-cause readmission rates for individuals with HF, AMI, and pneumonia.
Perhaps even more troubling is the large proportion of individuals in the sample with mental health comorbidities. Nearly 30% of individuals admitted to the hospital with HF, AMI, or pneumonia were diagnosed as having a mental health condition in the previous year. This is a higher percentage than the one reported by a national survey, which found that 26% of the general population reported having a mental health condition in the past year (
17). Most important, individuals with a psychiatric concern probably accounted for an even larger proportion of admissions for HF, AMI, or pneumonia, but because mental health conditions are often not diagnosed (
18), their illnesses were not captured in medical records. However, individuals with a psychiatric diagnosis likely had more severe symptoms, which may have increased the likelihood of readmission. Similarly, it would be interesting to understand whether receipt of different outpatient mental health or general medical treatments had an impact on readmissions. However, those who received treatment likely had more severe conditions, so this relationship cannot be assessed without controlling for severity. Thus, for several reasons, more research is needed to understand the influence of severity of illness on readmissions.
This study is particularly important for consideration of interventions to reduce readmissions for individuals with HF, AMI, and pneumonia. In a recent article, Burke and Coleman (
19) reported five principles to consider when designing readmissions interventions. The last principle is to broaden interventions to specifically target high-risk groups, such as individuals with psychiatric disease. Given the increased risk of readmission among individuals with psychiatric comorbidities and the large proportion of individuals with these conditions, health systems should consider adding elements of mental health assessment, diagnosis, monitoring, and treatment to interventions to prevent 30-day all-cause hospital readmissions. Unfortunately, although numerous interventions to reduce readmissions for individuals with HF, AMI, and pneumonia (
20–
22) have been developed, very few include specific mental health content (
19). However, some interventions to alleviate mental health and general medical comorbidities overall have been developed (
23). It may be possible to draw knowledge from these studies to develop interventions to reduce readmissions.
Although clinical recommendations are not the focus of this study, the results suggest that readmissions-focused interventions should consider adding mental health components. For example, these components may include psychiatric screening and assessment, discharge planning for multiple conditions, and specific follow-up related to mental health. The first step in this process is identification, including screening and assessment (
24–
28). Screening for mental disorders can be accomplished by using a battery of brief instruments (
29–
31). Because depression, anxiety, and substance use disorders appeared to be the most common diagnoses among participants in this study, and because each was associated with increased readmission rates, these disorders may be the most appropriate for health care systems to focus their primary screening efforts.
Previous studies also demonstrated that rates of readmission after psychiatric hospitalization are dramatically lower when individuals receive discharge planning and attend outpatient specialty treatment (
32,
33). A health care provider can assist with coordinating follow-up appointments, monitoring both medical and psychiatric conditions, and supporting individuals regarding their psychosocial and environmental concerns. This is particularly important for individuals with mental health concerns, who are more likely to miss follow-up appointments (
34). Part of this process may involve improving health literacy, which is traditionally low for individuals with mental health conditions (
35). This can include a brief assessment of the patient’s understanding of discharge instructions and postoperative self-care (
36,
37).
The data in this study indicate that the gap between readmissions of persons with and without psychiatric comorbidities appears to be shrinking, but the rates are unlikely to converge without specially designed interventions for both conditions (
19). It is promising that health systems appear to be able to reduce overall readmissions, especially given the high cost of hospitalizations. For example, the average hospitalization related to HF is estimated to cost around $25,000 (
38). The decline in rates of readmission from 2009–2011 is likely due to increased efforts to reduce readmissions in response to impending CMS policy changes, which began in 2012 (
4). It is estimated that well-designed interventions focused on multiple conditions may be even more effective at reducing readmission rates, thereby improving the quality and cost of care and mitigating hefty CMS penalties for health care systems of up to 1%–2%.
This study had several limitations. First, all the participating health systems are well resourced and have affiliated health plans. This combination may provide improved care coordination, which may lower overall rates of readmissions compared with other settings. Second, although this study presented data on a large national sample, the participating hospitals do not cover every geographic region in the United States and may not be representative of poor or uninsured community populations. Third, although the combination of systems (health plan and health system) captured nearly all the participants’ health care, utilization that occurred outside the health system and was not reimbursed by the affiliated health plan may have been missed. Because these visits are typically large expenses, the extent of this issue is likely very low, given that individuals would be more likely to use their insurance to pay for services.
Fourth, it is not possible to disentangle the relationship between many mental health conditions and severity of medical illness, but that relationship is almost certainly bidirectional. For example, depression can lead to worsening of heart disease, and more severe heart disease can contribute to depression. Future research may seek to clarify the important relationship between these variables. Fifth, we were not able to assess whether individuals with mental health conditions were more likely than persons without mental health conditions to experience more difficult hospitalizations, for example, longer stays, or more concerns after discharge, such as drug interactions. We were also not able to determine whether having multiple comorbid psychiatric conditions exacerbated their general medical illness or whether duplication of individuals in different subgroups influenced the magnitude of the findings. Sixth, our ability to capture admissions for HF, AMI, pneumonia, and comorbid psychiatric conditions was limited to the diagnostic codes entered by clinicians at inpatient and outpatient encounters in each health care system. Thus we were not able to assess diagnoses that were present but not coded and the severity of disease.
Seventh, we were not able to present site-specific data in this study. However, the data were consistent across sites. Thus the results of this study were not likely influenced by abnormal rates at a small number of sites. Finally, the data for this study included aggregated counts collected from all the sites, and thus we were not able to perform additional stratified and adjusted analyses that may have shed more light on the relationships. It is possible that readmission rates are related to demographic and diagnostic characteristics. Future research may consider additional investigation along these lines.
Conclusions
Overall, this study demonstrated that psychiatric comorbidities were associated with 30-day all-cause readmissions of individuals with index hospitalizations for HF, AMI, and pneumonia. The large proportion of individuals with HF, AMI, or pneumonia and psychiatric comorbidities suggests that comprehensive interventions for multiple conditions may be necessary. By implementing more comprehensive interventions and targeting individuals at higher risk of readmission, it may be possible to make progress toward the long-term goal of improving the quality and cost of health care and mitigating the risk of hospital penalties for excessive readmissions.
Acknowledgments
This project was supported by funding from the National Institute of Mental Health (U19MH092201) and the Fund for Henry Ford Hospital and by an award (IIR-09-335) to Dr. Copeland from the Health Services Research & Development Service, Veterans Health Administration. The authors thank all members of the HMO Research Network and the Mental Health Research Network, whose contributions to building the Virtual Data Warehouse and to the integrity of the data made this study possible. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
The authors report no financial relationships with commercial interests.