Individuals with serious mental illness have high rates of treatment discontinuation. Between 30% and 45% either fail to attend initial scheduled clinic visits or routinely discontinue treatment (
1–
4), and fewer than 50% receive continuous treatment for 12 months (
5). Inadequate follow-up is a strong predictor of inpatient readmission, homelessness, and incarceration (
3,
4,
6,
7). Evidence-based practices are available for engaging individuals who frequently discontinue services (
8–
10), but it is unclear how best to identify individuals who may benefit from outreach.
One approach involves examining patterns of service use for populations of individuals. From 2009 to 2011, the New York City (NYC) Mental Health Care Monitoring Initiative used Medicaid claims and other administrative data to monitor service use by defined cohorts of individuals in NYC with serious mental illness and high service needs (
11). In calendar year 2010, care monitors reviewed service use for 4,314 of these individuals who met predefined criteria suggesting disengagement from services and confirmed that 2,388 (55%) were not receiving adequate care (
11). This report describes rates of reengagement in services for 2,834 individuals (2,388 individuals plus another 446 subsequently identified) over a 12-month period after initial determination that the individual was disengaged from care. We describe rates of reengagement for individuals grouped according to individual characteristics and availability of outreach resources.
Methods
The monitoring and review procedures for the Mental Health Care Monitoring Initiative are described elsewhere (
11). The initiative focused on high-need Medicaid beneficiaries with serious mental illness who were receiving federal Supplemental Security Income benefits. High-need cohorts were defined on the basis of prior service use and included individuals who received court-ordered outpatient services at any time since NYC implemented its outpatient commitment program in 2000, received assertive community treatment or case management services in the prior 12 months, received mental health services in a state forensic prison program in the prior five years, or had two or more inpatient stays or emergency room visits in the prior 12 months. The cutoff periods for the three latter groups were identified on the basis of preliminary estimates of the size of each cohort and the resources available to implement reviews (the initially identified high-need group included nearly 9,000 individuals).
Each month, the cohorts were updated, and Medicaid claims were examined by using the following “notification flags” to identify individuals potentially in need of outreach: continued frequent psychiatric hospitalizations (two or more hospitalizations in the previous four months), lack of engagement in outpatient services (no outpatient visits for a mental or substance use disorder in the previous four months), or lack of adherence to psychotropic medications (no psychotropic medication prescription fills in the previous two months).
Project care monitors (licensed clinicians supervised by a managed care vendor with which the state contracted for the initiative) spoke with providers who had served the individuals to determine whether the notification flags accurately identified individuals who were disengaged from services. The 2,834 individuals confirmed to be disengaged were grouped into four categories. The first category was provider notified of need for active outreach (provider notified–active; N=657); for these individuals the vendor identified a mental health provider able to conduct outreach. The second category was provider notified of need for enhanced outreach (provider notified–enhanced; N=14); these individuals were confirmed to be in the community and were determined to be in need of immediate outreach to prevent a situation of potential imminent danger to self or others. The third category was incarcerated (N=611); these individuals were confirmed to be in prison or jail at the time of review (individuals serving prison sentences longer than three months were not coded as disengaged in this initiative). The fourth category was lost to care (N=1,552); for these individuals, no provider could be identified who was able to conduct outreach and contact the individual.
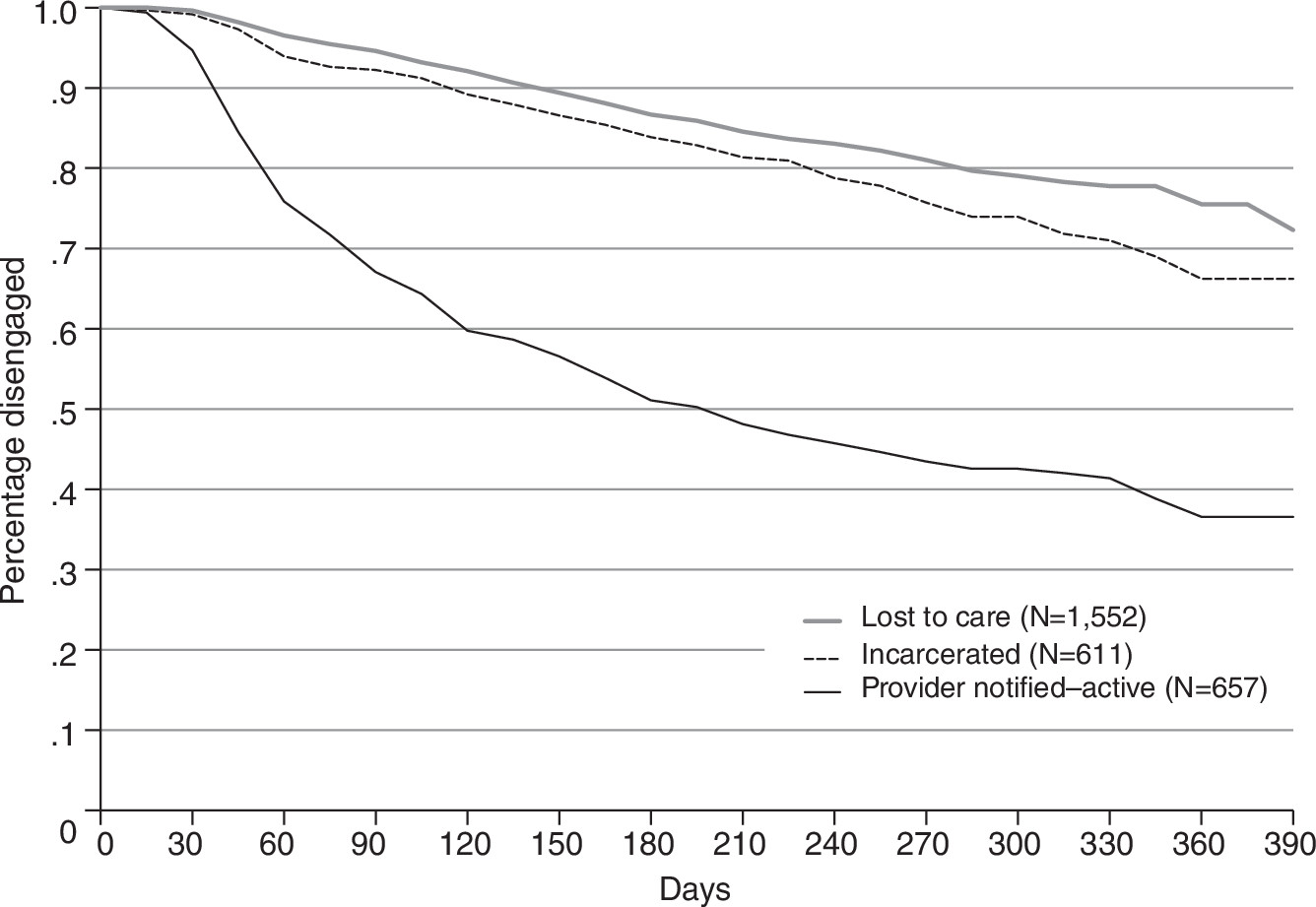
Care monitors reviewed claims data and contacted providers at least monthly for follow-up for disengaged individuals. An individual was coded as reengaged in care when a provider reported that the individual was receiving mental health services that the care monitor believed were appropriate to the individual’s needs. We created Kaplan-Meier survival curves illustrating rates of reengagement for the 12 months after an individual triggered a notification flag. The Central Office Institutional Review Board of the New York State Office of Mental Health approved the project as a quality improvement activity that did not constitute research involving human subjects.
Results
Figure 1 shows time to reengagement for three of the four categories of individuals. No survival curve is shown for the provider notified–enhanced group because of its small size; ten of the 14 individuals in this group reengaged by month 3, and 12 reengaged by month 12. Reengagement rates at three months for the provider notified–active, incarcerated, and lost-to-care groups were 33%, 8%, and 5%, respectively. By one year, reengagement rates for these groups were 63%, 34%, and 24%, respectively.
Discussion
Engagement in services is driven not only by individual characteristics but also (and perhaps more importantly) by the nature of provider outreach and the quality of the relationship developed between the individual and provider. In the Mental Health Care Monitoring Initiative, reengagement rates for individuals confirmed to be disengaged from services varied by both individual characteristics and the nature of provider outreach. The provider notified–enhanced group showed the highest rates of reengagement, which may be understandable given the small number of individuals in this group and the care monitors’ encouragement of assertive provider outreach because of the determination of potentially imminent risk of danger. The much larger group of individuals in the provider notified–active group showed similar rates of reengagement in the first three months, tapering off throughout the remainder of the follow-up period. We did not have a comparison group on which to base conclusions regarding the impact of providers’ outreach efforts, and it is possible that these individuals would have reengaged at a similar rate without outreach.
Individuals in the lost-to-care group reengaged at lower rates, which would be expected given the absence of an identified provider able to conduct outreach. The similarly low rates of reengagement for individuals in the incarcerated group are concerning given that the care monitors were aware of these individuals’ incarceration status and in a position to recommend postrelease referrals and outreach. Such recommendations, if made, did not result in increased rates of engagement. Incarcerated individuals with serious mental illness have complex service needs that are often not adequately addressed (
12). These individuals also disengage for policy-related reasons. In New York State, Medicaid benefits are not terminated when an individual is incarcerated, but they are suspended and must be reinstated upon release. Individuals may be more likely to disengage if their Medicaid coverage remains suspended because the state Medicaid program was not notified in a timely way of an individual’s release from incarceration. Clearly, there are many missed opportunities to reengage these individuals on reentry to the community.
Limitations of these data include the inability to distinguish between individual versus provider characteristics that influence reengagement. We were also unable to determine whether care monitor reviews had an impact on provider engagement efforts or reengagement rates. Finally, we were unable to discern cases in which the disengagement from treatment represented a rational and appropriate decision made by the individual.
Conclusions
The NYC Mental Health Care Monitoring Initiative demonstrated that administrative data could help identify individuals in need of outreach. Subgroups of disengaged populations had different rates of reengagement, and active outreach might have had an impact for some of these individuals. Future research and clinical efforts should refine the impact of such care monitoring initiatives and further strengthen public health safety nets.
Acknowledgments and disclosures
This work was supported by the New York State Office of Mental Health. The authors thank Dana Cohen for assistance.
The authors report no competing interests.