Second-generation antipsychotics were introduced in the 1990s. Thought to be more effective and safer than first-generation antipsychotics, they captured a majority of the antipsychotic market in many countries and have contributed to the expansion of antipsychotic use (
1). In the United States, for example, antipsychotic use increased from 5.6 monthly treatments per 1,000 U.S. inhabitants in 1998 to 9.5 in 2008 (
2), with most of the growth attributed to use for nonpsychotic disorders (
3).
However, evidence published in the 2000s, suggests that, with the exception of clozapine, second-generation antipsychotics may be no more effective than first-generation antipsychotics in treating schizophrenia and that they come with significant risks and higher costs (
4).
Some studies have provided patient- or population-level data about the response to this new evidence (
5–
7), but little is known at the physician level. Even though debate persists over how to interpret the findings of comparative effectiveness studies, physicians may have changed their prescribing practices. They may have prescribed fewer antipsychotics or they may have changed their preferences for specific agents. Ideally, a physician’s preferred agent is the one with the best benefit-risk ratio for his or her patient population; however, studies suggest that physician preferences for specific medications are weakly associated with patients’ clinical characteristics (
8,
9).
Little is known about the antipsychotic prescribing behavior of general practitioners (GPs) despite the fact that in some countries they account for most antipsychotic prescriptions (
10). We conducted a longitudinal study of antipsychotic prescribing by GPs in France. By 2010, French physicians faced a choice of 15 first-generation and five second-generation antipsychotics. No economic or regulatory barriers limited their choice, because no prior authorization is required and, theoretically, full coverage is offered to all patients receiving antipsychotics for approved conditions (on label) (
2). We expected that during the 2000s, GPs may have shifted their preference for antipsychotic drugs or stopped prescribing certain drugs on the basis of new data about cost-effectiveness (which would favor first-generation antipsychotics) and benefit-risk ratio (which would favor switching from antipsychotics with high metabolic risk to those with a lower risk). We examined GPs’ changes in preferences, which may reflect physicians’ responsiveness to new information or other market-level changes.
Methods
We used data from the Disease Analyzer database of IMS Health, which is a database of electronic records from a panel of GPs since 2000. These data provided a longitudinal follow-up of physicians and their patients. The data are intended primarily for use by commercial entities, but they have also proven useful for research purposes (
11,
12). Included GPs were randomly selected from the lists of physicians who were using software compatible with IMS Health’s requirements. GPs voluntarily participated in the Disease Analyzer database and received financial compensation for their computer costs. Of those contacted, about 10% of GPs participated.
According to IMS Health, included GPs are representative of the 60,832 French GPs in terms of age, volume of consultations, and practice characteristics (for example, specializes in homeopathy, acupuncture, or mesotherapy), and patients are representative in terms of age and sex of all patients in France who have consulted at least one GP.
To study a cohort of regular prescribers of antipsychotics, we restricted the database to GPs who had prescribed at least 12 prescriptions for antipsychotics in 2003 and in 2010 and at least one antipsychotic prescription every year in 2004–2009.
Antipsychotics were defined as drugs with a code starting in “N05A” in the anatomical, therapeutic, and chemical classification, excluding lithium, veralipride, and chlorproethazine, which are not labeled for use in psychosis. Furthermore, in accordance with previous work (
13), we excluded cyamemazine and levomepromazine because these low-potency antipsychotics (which represented 20.3% and 22.0% of total antipsychotic use in France in 2003 and 2010, respectively) are typically used as hypnotics or anxiolytics in France. Amisulpride, clozapine, olanzapine, risperidone, and aripiprazole (the latter available since June 2004) were categorized as second-generation antipsychotics.
We report mean annual number of antipsychotic prescriptions and patients by physician and by year. For each year and physician, we determined his or her preferred antipsychotic drug in two steps. First, we defined the GP’s preferred drug for each patient. Then among patients of each GP, we determined the drug preferred for most of that physician’s patients. If there was a tie, physicians were grouped together in a “more than one preferred drug” class. For each year and physician, we calculated the percentage of prescriptions issued for the preferred agent. Finally, we classified physicians into three groups according to their preference: physicians preferring one or more first-generation antipsychotics, one or more second-generation antipsychotics, and no preference (that is, prescribing first- and second-generation antipsychotics equally over the year). Comparing the preferred drugs in 2003 and 2010, we focused on GPs who changed from preferring first- to second-generation antipsychotics. We compared mean rates of use of each product and share of use for the various antipsychotic drugs between 2003 and 2010 by using matched-pairs t tests, and we used a transition matrix to represent changes in GPs’ preferences. Statistical analyses were performed with SAS, version 9.3. Our study did not require approval by our institution’s Ethics Committee because we used existing data free of personal identifiers.
Results
Among the 1,261 GPs who had a record of any antipsychotic prescribing in the database, 347 (28%) GPs met our inclusion criteria. Most were men (N=324, 93%), and the mean±SD age of the sample was 55.8±6.2 at the end of the eight-year period. In 2010, they had prescribed antipsychotics in about 1.1% of their consultations, for a mean of 14.0±8.3 patients. [Characteristics of prescribers are summarized in a table in an online data supplement to this report.] Overall, 20,361 patients had received at least one antipsychotic prescription at some point in the period. Data on indication for the antipsychotic prescription were available for 11,349 patients (55.7%). The most common indications were anxiety (25.1%), schizophrenia and other psychoses (24.1%), depression (19.9%), bipolar disorders (10.6%), pain (8.6%), and dementia (6.7%).
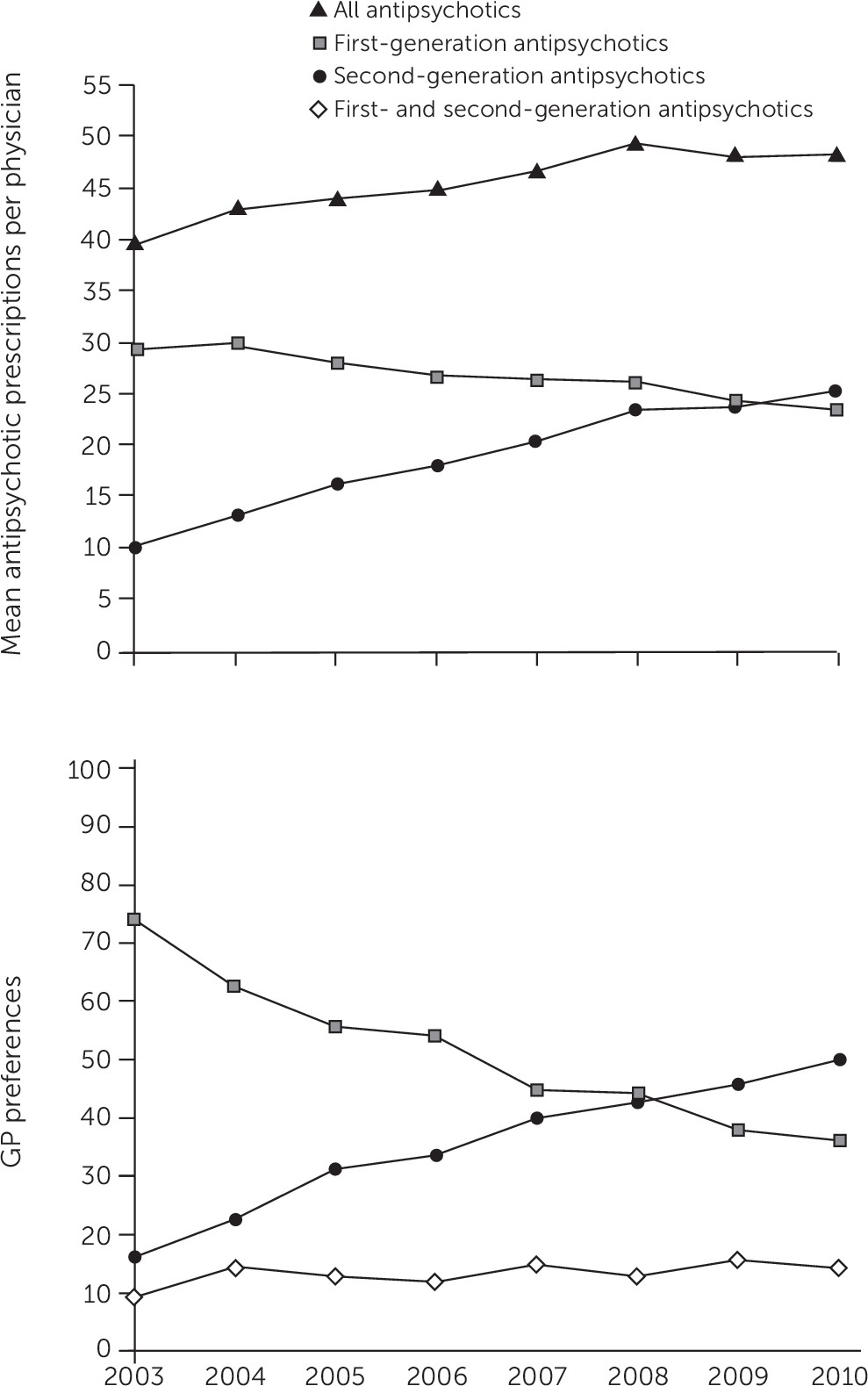
Figure 1 shows the number of antipsychotic prescriptions and GP preferences over the period. The mean annual number of antipsychotic prescriptions per physician increased from 39.6±29.5 in 2003 to 48.4±37.0 in 2010 (p<.001), whereas the number of patients using antipsychotics per physician remained stable (14.2±10.0 in 2003 and 13.7±8.2 in 2010). In 2003, first-generation drugs were the most commonly prescribed antipsychotics (sulpiride and haloperidol represented 23.5% and 13.8% of prescriptions, respectively). By 2010, second-generation antipsychotics captured most of the prescriptions, with risperidone alone accounting for 22.5% of overall prescriptions. [A figure in the
online supplement presents results for individual agents.]
On average, GPs prescribed 6.4±2.1 different antipsychotic medications in 2010 (3.4±1.6 first-generation agents and 2.9±1.0 second-generation agents). The share of prescriptions for the preferred drug decreased slightly over the period (39.9%±18.1% in 2003 versus 37.3%±17.4% in 2010, on average, p=.036). This share was similar for physicians who preferred first- or second-generation agents in 2010 (38.7%±19.1 versus 36.3%±16.0).
The percentage of GPs who preferred a second-generation antipsychotic increased from 16% in 2003 to 50% in 2010 (
Figure 1). Among the 257 GPs who preferred first-generation antipsychotics in 2003, 42% (N=108) switched to preferring second-generation drugs and 15% (N=38) to prescribing second- and first-generation drugs equally in 2010. Transitions from first- to second-generation antipsychotics varied according to the preferred molecule. Among physicians who preferred haloperidol in 2003, 61% shifted to a second-generation antipsychotic in 2010. Among those who preferred tiapride in 2003, 51% shifted to a second-generation antipsychotic in 2010. Conversely, only 33% of physicians who preferred sulpiride in 2003 had switched to preferring a second-generation antipsychotic in 2010. [A table in the
online supplement presents results of these analyses.]
Discussion and Conclusions
To our knowledge, our study is the first in Europe, and second worldwide (
14), to examine changes in physicians’ preferences for antipsychotic drugs. We observed significant changes in preferences over the eight-year period, but the percentage of prescriptions for the preferred drug remained stable. Between 2003 and 2010, half of the GPs switched from preferring first- to second-generation antipsychotics.
The observed trends in antipsychotic use in France are consistent with previous findings from population-based studies and showed a slower uptake of second-generation antipsychotics in France compared with other countries (
1,
2). This delay may be partly explained by the lack of availability until November 2011 in France of quetiapine, a drug representing a large share of second-generation antipsychotic use abroad (
2). Our results do not suggest an overall response of French GPs to the new evidence. Indeed, we did not observe any decrease in antipsychotic use, any increased preference for the most effective drug for treating schizophrenia (clozapine) or for more cost-effective drugs (first-generation antipsychotics), or any decreased preference for the drug with the highest metabolic risk profile (olanzapine). This finding about olanzapine contrasts with the U.S. response regarding its use (
14). Indeed, the proportion of GPs in France who preferred olanzapine increased from 2% to 9% between 2003 and 2010, whereas the proportion of U.S. physicians who preferred olanzapine dropped from 30% in 2002 to 10% in 2007 (
14). However, dissemination of new evidence differed between the two countries because the French drug agency did not issue any warning about metabolic risk in 2003 and use of olanzapine in France was low.
Our study had some limitations. First, our sample of GPs may not have been representative of all GPs in France; in particular, women were underrepresented. Second, we had no way to identify prescriptions that were initiated by psychiatrists. Therefore, prescriptions that were not initiated by GPs were included in determining their preferred drug. However, we suspect that many patients’ treatment was initiated and managed solely by their GP because most antipsychotic prescriptions were for treating nonpsychotic disorders (such as anxiety and depression). Third, data on diagnosis were missing for nearly half the patients, and thus we were unable to examine changes in preferences by indications. Last, our study was not designed to infer a causal relationship between the release of new evidence and changes in prescribing behavior.
Despite its limitations, this study is the first to provide physician-level data on antipsychotic prescribing in Europe. Physicians’ preferences changed dramatically between 2003 and 2010, with about half switching their preference to second-generation antipsychotics.