For individuals with severe mental disorders, such as schizophrenia and bipolar disorder, noncompliance with treatment is usually associated with repeated relapses (
1,
2). After discharge, patients who receive treatment in a hospital for such conditions usually do not use outpatient services regularly and a majority, it seems, do not adequately comply with treatment (
3). Possible reasons for noncompliance include lack of insight (
4,
5), delusions (
6,
7), and simultaneous alcohol and substance abuse (
8). All patients with severe mental disorders experience repeated hospitalizations, and it is estimated that 30% to 50% of patients with severe mental disorders require rehospitalization within one year after their discharge from the hospital (
9).
The literature shows that providing continuous care and follow-up services in the community may decrease the odds of future hospitalizations. These aftercare services decrease the need for rehospitalization, improve patients’ clinical status and compliance with treatment, and increase patient satisfaction (
10–
12). Evidence supports the use of specific aftercare services, including follow-up care (
13–
15), family psychoeducation (
16–
18), and social skills training (
19–
21).
Home visits and telephone prompts are the two common models of follow-up care. Studies have shown that home visits significantly decrease the risk of relapse and rehospitalization among persons with severe mental disorders and can improve patients’ clinical symptoms and reduce the severity of the disorder (
21,
22). Also, evidence indicates that this service can reduce treatment-related costs (
12,
13). A Cochrane systematic review demonstrated that telephone follow-up increases the odds of presenting to outpatient clinics (
23). According to MacDonald and others (
14), telephone follow-up increased the odds of patients’ keeping their first appointment.
Lack of social skills among patients with severe mental illness has a close association with repeated relapses and rehospitalization and is an influential factor in prognosis (
24). Moreover, patients with chronic mental disorders often have low self-esteem (
25), which prevents them from establishing effective relationships and has a negative impact on their capability for adaptation to stress. Social skills training decreases the severity of symptoms and number of relapses and rehospitalizations and improves patients’ performance in terms of social skills (
26–
28).
Several studies have reported that family interventions that include psychoeducation are effective in improving the emotional expression of the family (
29,
30). However, because family psychoeducation is often combined with other interventions, it has been difficult to determine the extent of its contribution to patients’ recovery (
31). Family interventions with the aim of educating and supporting patients’ families have been effective in reducing relapses, number of hospitalizations, and stress on the families. Such interventions also improved the adaptation skills of the families (
32–
34). In recent years, old beliefs that held the family responsible for the disease have given way to a focus on cooperation with the patient’s family that is based on their capabilities and requirements (
35,
36).
Aftercare services are comprehensive interventions that provide continuous care for patients and prevent relapse and rehospitalizations. Every community that uses aftercare services should be able to produce evidence that documents their efficacy. The objective of this study was to compare the effectiveness of aftercare services and treatment as usual among patients with severe mental illness. Treatment outcomes included the severity of psychopathology, number of rehospitalizations, and length of hospital stay. We also tested the hypothesis that patients who received aftercare services would have reduced length of hospital stay. Findings of this study are part of a larger multicenter project evaluating the efficacy and cost-effectiveness of aftercare services and their impact on different measures of patients’ outcomes during a 12-month follow-up period (
37). In this study, the follow-up period was extended to 20 months. Thus the results reported in this study are based on a 20-month follow-up.
Methods
A total of 120 patients with severe psychiatric disorders at Iran Mental Hospital were selected for this study after informed consent was obtained from the patients and their family. The project coordinator in charge of screening hospital wards conducted patient selection. Patients with schizophrenia and schizoaffective and bipolar disorders between ages 15 and 65 were selected. The other inclusion criterion was living with at least one family member. Severe physical disability, concurrent neurological conditions, and mental retardation were among the exclusion criteria. Patients who did not sign an informed consent agreement were excluded from the study and received treatment as usual. A detailed description of the methodology of this study can be found in the study protocol paper (
37).
Patients who entered the study were equally divided into an intervention group that received aftercare services and a control group that received treatment as usual by using stratified balanced blocked randomization with allocation concealment (allocation ratio 1:1). Randomization was provided by an independent statistician at the medical university affiliated with the hospital. First, patients were assigned to two groups on the basis of disorder severity (high or low), depending on number of hospitalizations and compliance with treatment. Next, patients in each group were divided into intervention and control subgroups. For example, patients with high severity of disorder were randomly assigned to one of the two subgroups mentioned. [A description of the randomization process is available as an online supplement to this article.]
Intervention Group
Aftercare services included three components: follow-up care (home visits or telephone follow-up), family psychoeducation, and social skills training for patients.
Treatment follow-up.
Aftercare services were provided for two groups of patients: those who required more assertive follow-up because of poor compliance with treatment and those who required less serious follow-up services because of better compliance. Patients who required more assertive follow-up received home visit services. Patients who required less serious follow-up services received telephone follow-up prompts to attend the outpatient clinic for follow-up visits, which usually occurred on a monthly basis. Both follow-up modes were different components of the active intervention, and patients could cross between them on the basis of their improvement or deterioration during the study period. All assignments were made by the supervising psychiatrist of the research team on the basis of clinical judgment.
Family psychoeducation.
The goal of family psychoeducation was to provide psychosocial care for the family members of patients with severe mental disorders. This program had three stages: establishing a primary rapport with the patients’ family, enhancing the knowledge and strengthening the coping skills of the patients’ family, and providing support services for the family. To enhance knowledge and coping skills, families of patients in the telephone follow-up group attended six weekly two-hour multiple-family group sessions, and families in the home care group participated in six weekly two-hour single-family sessions. Support services included crisis intervention services and contact with local nongovernmental organizations and self-help groups. This part of the intervention was designed according to a manual adapted to the Iranian culture (
38).
Social skills training.
Social skills education for patients started after the family began psychoeducation, usually three months after the inclusion of patients in the study. For the telephone follow-up group, this service included ten weekly sessions of education in an outpatient clinic. For the home visit group, the home visit team offered nine training sessions to patients on a monthly basis in the convenience of their own home. The framework of this intervention included psychoeducation, modeling, shaping, and reinforcement.
Control Group
The control group and the intervention group participated in similar assessments, but the control group did not receive the aftercare services. They received routine clinical services, including a first visit two weeks after hospital discharge followed by monthly visits by a psychiatrist or a psychiatric resident. This schedule of visits was the usual care provided by the hospital following discharge. However, not all the patients in the control group complied with this process.
Outcomes and Data Collection
The primary outcome measures were length of hospital stay and number of psychiatric rehospitalizations during the 20 months after discharge. Data regarding rehospitalizations of patients and length of hospital stay were collected during follow-up sessions and recorded in a questionnaire designed by the research team. The questionnaire contained questions for patients and their family members. Also, medical records of patients were reviewed, if required.
Secondary outcome measures were the severity of psychopathology and the severity of illness. The tools used for data collection were the Positive and Negative Syndrome Scale to assess psychotic symptoms (
39), the Young Mania Rating Scale to assess manic symptoms (
40), the Hamilton Rating Scale for Depression to assess depressive symptoms (
41), and the Clinical Global Impression to assess illness severity (
42). Data regarding the intervention and control groups were collected by an experienced trained clinician at baseline (inclusion in the study), at discharge, and at three, six, 12, and 20 months postdischarge in an outpatient clinic or at a patient’s home.
Considering the high rate of loss to follow-up in such studies (
43), a follow-up strategy was designed at the study onset. It should be noted that because the follow-up evaluations were conducted by clinicians who were in direct contact with patients, it was not possible to blind the clinician from knowing whether a patient was assigned to the intervention or the control group.
Analyses
Descriptive summaries of sociodemographic and clinical data were compiled for both groups; these included means and standard deviations or proportions of background variables. Each patient’s clinical ratings on the four secondary outcome measures were summarized by total score and by percentage of change from baseline measures. An “intention to treat” approach was employed. Baseline nominal or ordinal variables for the intervention and control groups were compared by chi square test; baseline quantitative variables for the two groups were compared by using t test or Mann-Whitney U test, considering the assumptions of each test. The quantitative primary and secondary outcomes measures for the two groups were compared by using general linear model (GLM) repeated-measures analysis (repeated-measures GLM). We used repeated-measures GLM to detect differences of within-subject variations over the whole study period between the study groups. We used t test to compare the cumulative hospital stay in each period of follow-up (three to six, six to 12, and 12 to 20 months after discharge). The Statistical Package for Social Sciences, version 18.0, was used for data analysis.
Ethical Considerations
Before entering the study, patients and their family members were informed about the study conditions and processes, and written informed consent was obtained from them and their guardians (
37). Our study design was approved by the Ethics Committee of Tehran University of Medical Sciences (#130–6-2441) and was in complete agreement with the 2008 Declaration of Helsinki.
Results
Characteristics of the Study Population
The recruitment period for the study was March 2009 to December 2010. The 120 participants were randomly divided into intervention and control groups, each with 60 participants. At the onset of the study, 31 (52%) patients in the intervention group were assigned to telephone follow-up prompt, and 29 (48%) were assigned to home visits. However, because switching between subgroups was allowed, the telephone follow-up and home visit subgroups were evaluated as one group. At the end of the 20-month follow-up, all 60 patients in the control group were accessible and were evaluated, but three patients in the intervention group had been excluded from the study, two because of death (one due to ischemic heart attack and the other due to electric shock) and one because the patient had relocated to another city. There were significant differences between the two groups in terms of marital status, level of education, and history of aggressive behaviors, but otherwise background variables for the two groups were comparable.
Table 1 shows the demographic characteristics of patients in the intervention and control groups.
Comparison of Outcomes
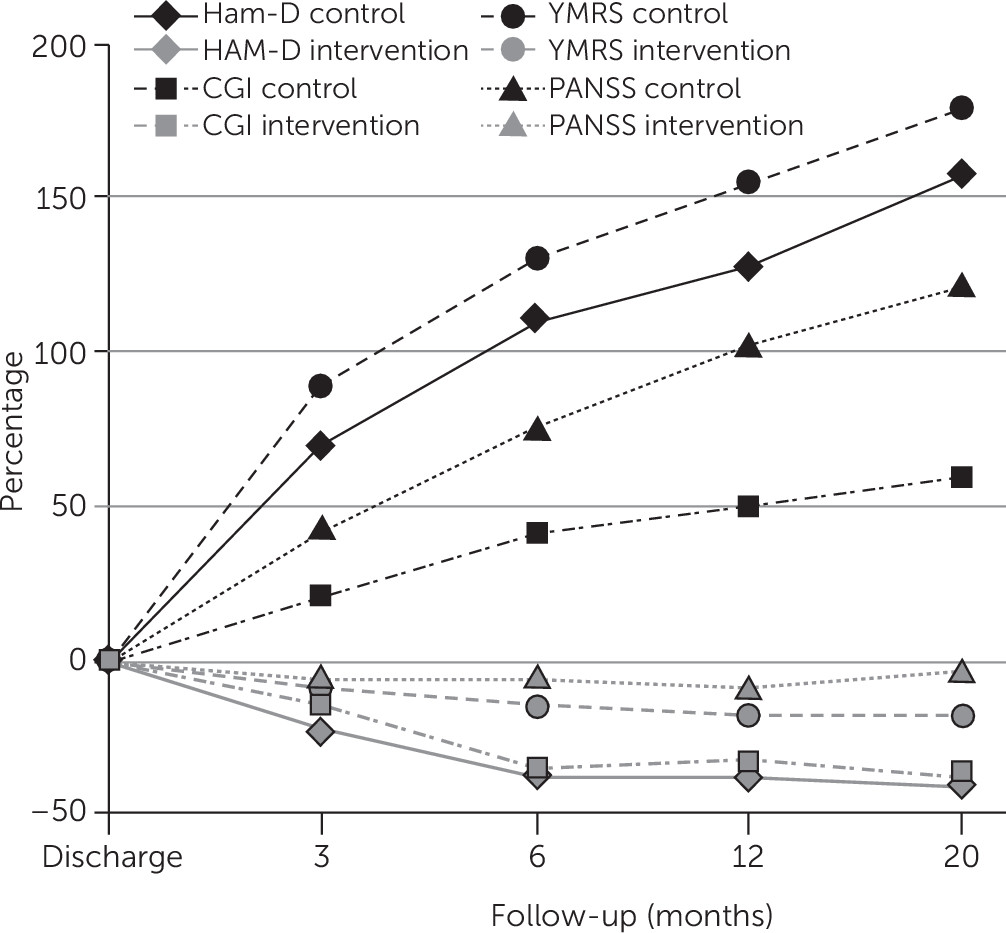
Table 2 shows the trend in severity of psychopathology among the intervention and control groups between admission and the last follow-up session. After the onset of intervention, there were statistically significant differences between the mean scores on the four rating scales of the two groups at each follow-up. Repeated-measures GLM also revealed significant differences between the two groups over the whole study period.
Figure 1 shows the percentage of change in severity of psychopathology for both the intervention and control groups. Between the time of discharge and the last follow-up, severity of illness and psychopathology decreased among participants in the intervention group and increased among participants in the control group. The slope of the escalating trend for the control group during the 20-month period was sharper than the decreasing trend in the intervention group.
Table 3 shows number of hospitalizations due to the relapse of psychiatric disorder among the two groups. Cumulative number of hospitalizations during the first 20 months after discharge (onset of intervention) was 55 for the control group and 26 for the intervention group. Mean length of hospital stay (days) was greater in the control group compared with the intervention group at all follow-up periods (
Table 3). The highest monthly rate of hospitalizations in both groups occurred three to six months after discharge. The rate ratio of both hospitalizations and length of hospital stay (a comparison of the rate in the control group to the rate in the intervention group) was greatest during the 12 to 20 months after discharge. Repeated-measures GLM indicated that length of hospital stay during the follow-up periods was higher in the control group than in the intervention group (p=.01).
Discussion
This study aimed to compare the efficacy of aftercare services and routine clinical services during a 20-month period following hospital discharge. Aftercare services caused a significant improvement in all of the study variables compared with outcomes for treatment as usual, which indicates the effectiveness of the intervention. Number of hospitalizations and length of hospital stay (days) were significantly lower among patients who received aftercare services compared with patients who received treatment as usual. Our study results revealed that during the 20-month follow-up of patients, psychopathological symptoms were significantly less severe among patients in the intervention group than among patients in the control group. It is noteworthy that we found a relatively similar trend during each follow-up period.
In a 2001 meta-analysis, Burns and others (
44) demonstrated that home visit interventions could decrease the rate of relapse and rehospitalization of patients. The results of two other meta-analyses revealed that instruction of social skills could decrease the severity of symptoms, rate of relapse, and rehospitalizations among psychotic patients (
26,
45). In a Cochrane study, a meta-analysis was conducted of the results of ten randomized controlled trials of psychoeducation of patients with schizophrenia (
30). In nine of the studies, psychoeducation of patients’ families was part of the intervention, and it was shown that family psychoeducation reduced the rate of relapse and rehospitalizations at the nine- and 18-month follow-ups.
In our study, comparison of psychopathological indicators between the control and intervention groups indicated that the intervention had a significant effect on these variables. Psychopathological variables for the two groups were not significantly different during primary assessments and at the time of hospital discharge, which shows an acceptable randomization in this respect. However, postdischarge assessments revealed significant differences between the two groups at different follow-up periods and repeated-measures analysis also revealed significant differences between the two groups in all studied indicators.
Previous studies have shown that each part of the intervention could have played a role in reduction of the severity of symptoms (
46,
47). However, it is not possible to determine the share of improvement attributable to each part. For instance, when patients’ family members participate in psychoeducation sessions, it leaves a positive impact on patients’ acceptance and compliance with treatment; consequently, the severity of symptoms and rate of relapse decrease (
46,
47). The results of a study by Tsang and Pearson (
48) revealed that instruction of social skills to elderly patients improved their skills and decreased the severity of negative signs and symptoms. Different studies have shown that active follow-up and continuation of care after hospital discharge can decrease the severity of patients’ psychopathological symptoms (
22,
49,
50). Because pharmaceutical therapy plays a critical role in treatment of schizophrenia and bipolar disorder (
51,
52), regular patient visits and supervision of treatment can lead to a prescription for and continuation of pharmaceutical therapy. Regular patient visits can control the psychopathological signs of disease and subsequently decrease the rate of relapse and rehospitalization. The outcome of this supervision will be more prominent among patients with poor compliance with treatment.
Comparison of the number of hospitalizations between the intervention and control groups revealed that hospitalizations among patients in the control group exceeded those of the intervention group by a rate ratio of >1.00 for all assessments. This difference was more significant during the last two follow-ups (12 and 20 months postdischarge). Similar results were obtained for length of hospital stay. In other words, the difference between the two groups in days of hospital stay during the six-to-12-month and 12-to-20-month follow-up periods was significant. It should be noted that the magnitude of difference between the two groups increased over time as aftercare services continued (with the exception of a drop in rate ratio of hospitalization days from the first to the second three-month period after discharge), an indication that the continuation of the intervention was associated with stable efficacy of services, longevity of the outcome, and achievement of more favorable results.
The number of studies of the efficacy of community-based aftercare services in developing countries is small, but there are some studies from Iran and India that have reported the effectiveness of these interventions for improvement of mental health outcomes. Khankeh and colleagues (
53) provided self-care education for patients with chronic psychiatric illnesses after discharge from the hospital, where they had demonstrated relative improvement. At six-month follow-up, the patients showed significant improvements in self-care. Karamlou and others (
54) reported that family psychoeducation significantly improved cohesion and expressiveness. Chatterjee and others (
55) reported that community-based rehabilitation interventions enhanced the social function capabilities of patients with chronic psychiatric illnesses. Sharifi and others (
21) provided home visit services for patients with severe psychotic disorders after their discharge from the hospital. These services decreased the rate of rehospitalization, improved clinical symptoms, and increased the rate of satisfaction among patients.
In developing countries, studies of aftercare services have concentrated mostly on limited interventions and small populations of patients, mainly because of a shortage of resources and funding. One strength of this study was the inclusion of a variety of services in the design of the service pack and the use of home visits or telephone follow-up to provide continuous care and follow-up. On the other hand, by performing family psychoeducation, our study also focused on the family role as an influential factor in the course of treatment. By teaching skills to patients, we focused on the rehabilitation of patients so they can rejoin society. Another strength of this study was regular coherent and continuous follow-up of patients in a 20-month period; the appropriate and efficient communication of the follow-up team and the services offered to patients and their family members were the main reasons for the extended follow-up and the loss of a limited number of patients to follow-up. Thus comparison of the two groups was feasible in all phases of evaluation with the least amount of missing data.
Providing the package of aftercare services seems feasible, at least in all big cities of Iran. For introducing these services, financial and equity implications should be considered. Although the intervention itself imposes some extra costs to the health system, the decrease in the hospitalization rate and better psychopathological profile of the recipients of services have compensatory effects.
The study also had limitations. Although patients were randomly assigned to the intervention and control groups, some background variables—including marital status, education, and history of aggressive behaviors—did not have equal distribution among the two groups at baseline. The possible effect of these differences on intervention outcomes must be taken into account as a limitation of this study. Limited information is available to make a clear judgment about the methods used to address bias at various stages of the study. This introduces the possibility of selection bias and limits the generalizability of the findings to the larger universe of patients. On the other hand, this study was designed to assess the efficacy of a pack of aftercare services. Thus it is not possible to determine the share of efficacy of each intervention separately, which may also be considered as a limitation of this study. Based on the study design, patients in the intervention group could be switched during the course of study between the home visit and telephone follow-up subgroups on the basis of the supervisory psychiatrist’s judgment of the patients’ clinical status and treatment compliance. Therefore, comparison of the subgroups was not an objective of this study. Another limitation of our study was that blinding of raters was not possible because they were in direct contact with patients during the assessments. To reduce this confounding effect, caregivers did not complete follow-up assessments of patients for whom they provided treatment. One other limitation was that the results of this study cannot be generalized to persons who are homeless or who live alone because those living conditions were among the exclusion criteria of our study. Thus caution should be used when generalizing the results of this study to such patients.
Conclusions
On the basis of our results and the results of similar studies, we may conclude that aftercare services have a profound positive effect on the outcome of patients with severe psychiatric illnesses. These services not only decreased the number of hospitalizations and length of hospital stay but also improved the psychopathological symptoms of patients. Considering that at present the number of active beds in Iranian mental hospitals is half the estimated required rate, decreasing the number and length of hospital stays among patients with severe mental disorders is among the most important achievements of offering such services, given that in Iran, psychiatric beds are mainly occupied by patients with severe disorders. Extension and continuation of these services can compensate for the shortage of psychiatric beds and can begin a transition of services from a hospital-based, traditional system to a community-based system; such a transition is an accepted strategy for improving the quality of services and patients’ quality of life.