Depression is a highly prevalent comorbidity among patients engaged in HIV care, affecting 20% to 30% of such patients (
1,
2). Depression is associated with a range of adverse behavioral and health outcomes among HIV-infected patients, including reduced antiretroviral medication adherence (
3), poorer treatment outcomes (
4), and higher mortality rates (
5). Effective medication- and therapy-based treatments for depression are well understood and are effective for HIV patients (
6,
7). However, depression remains widely underdiagnosed and undertreated in this population because of stigma, health system fragmentation, access barriers, and other factors (
8,
9).
Integration of decision support models for antidepressant management in HIV clinical care is a promising avenue for large-scale improvement of the diagnosis and treatment of depression among HIV-infected patients (
10). In such models, also called collaborative care models (
11), a member of the clinic staff, such as a social worker or nurse, is trained to regularly assess key patient metrics, for example, depressive severity and medication side effects. The staff member uses an evidence-based algorithm as a guide for providing decision support to a nonpsychiatric provider for initiation and ongoing management of antidepressant treatment. The staff member is supervised by a mental health specialist. The evidence base for the use of such models in primary care is well established (
12), and the models have recently been adapted for HIV care (
10).
Such decision support models have the potential to efficiently expand the availability of evidence-based antidepressant treatment in HIV care. However, their success depends on patients’ and providers’ willingness to take advantage of them. This brief report describes the uptake of an evidence-based depression treatment intervention at two high-volume HIV clinics after integration of a decision support model into clinical care.
Methods
We adapted a measurement-based care depression treatment decision support model (
10) into routine HIV care at four HIV clinics, three based in academic medical centers and one in the community. The integration of the model into routine care was part of a multisite, randomized controlled trial to test the effect of depression treatment on HIV outcomes (the SLAM DUNC Study [
13]). Primary inclusion criteria for study enrollment included a positive screen (score ≥10) on the Patient Health Questionnaire–9 (PHQ-9) (
14), confirmed current major depressive disorder, and current or imminent antiretroviral treatment (because the study’s primary outcome was antiretroviral medication adherence). Primary exclusion criteria included past or current bipolar or psychotic disorder (
13). Trained staff members used the Mini International Neuropsychiatric Interview to assess psychiatric diagnoses.
For patients with an eligible PHQ-9 score, study staff first consulted with the HIV medical provider to ask whether the patient was an appropriate candidate for the study. With the provider’s approval, study staff then approached the patient to describe the study. Interested patients provided informed consent and completed additional eligibility assessments (primarily diagnostic assessments to confirm major depressive disorder and rule out bipolar and psychotic disorders). Participants who met all eligibility criteria were assigned at random to receive either usual care or measurement-based care.
Results
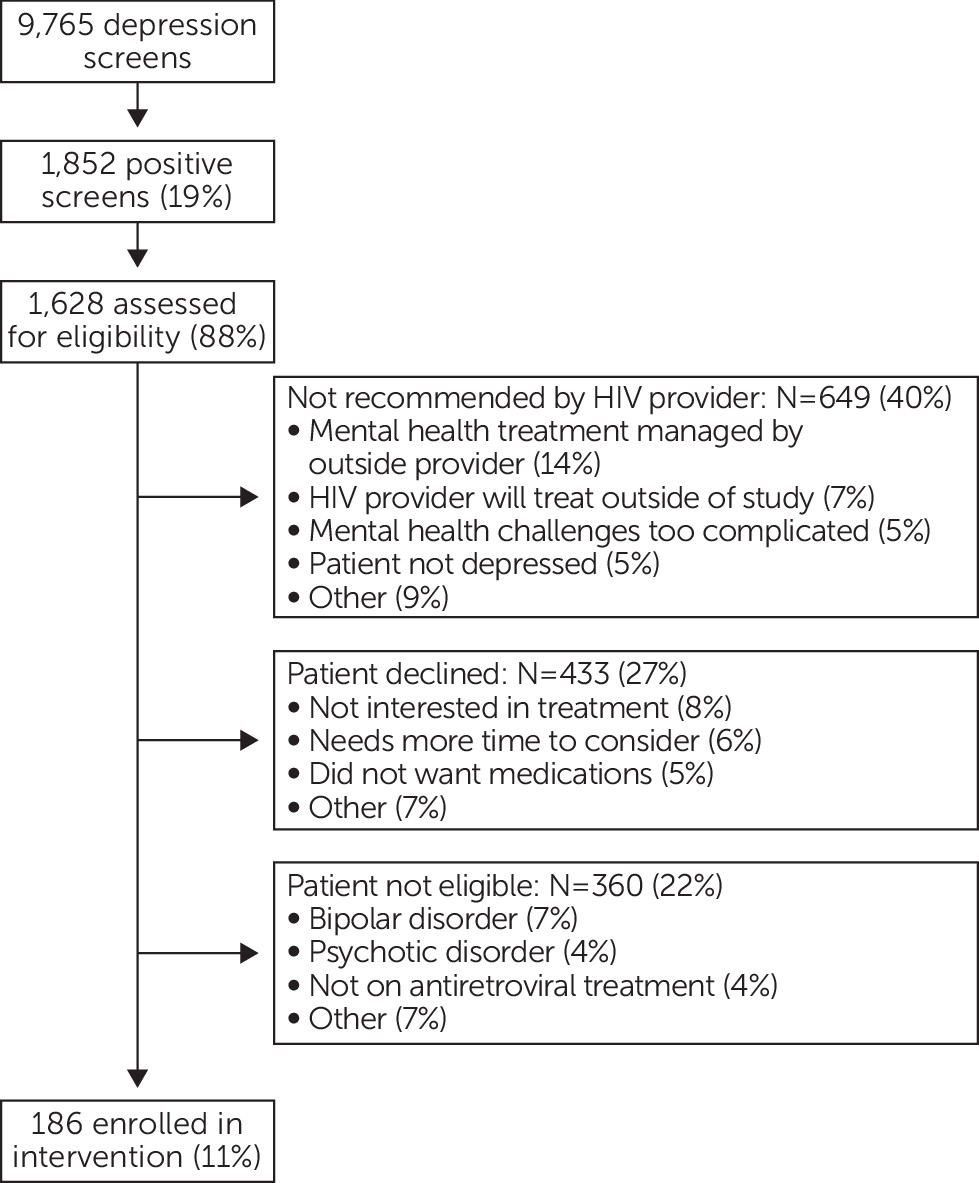
Two clinics initiated routine depression screening of all patients and kept detailed records of screening, eligibility, and enrollment outcomes over a 33-month period. A third clinic conducted routine screening but screening logs could not be utilized because of institutional review board constraints, and a fourth clinic performed targeted screening. Because screening outcome data did not capture patient identifiers, the results are reported as number of screening events rather than number of patients. During this time, 9,765 PHQ-9 depression screens, including multiple screens for many patients, were completed at the two sites. A total of 1,852 (19%) screens were positive, and of those, 1,628 (88%) were assessed for study eligibility (
Figure 1).
Of the positive screens that were assessed, 186 (11%) resulted in study enrollment. Among the positive screens that did not result in enrollment, in 649 cases (40%) the HIV provider did not recommend enrollment, in 433 cases (27%) the patient declined to enroll, and in 360 cases (22%) the patient did not meet study inclusion criteria.
When providers did not recommend enrollment, the most common reason was that the patient’s mental health treatment was being managed by a mental health provider outside the HIV clinic. Other common reasons for not recommending enrollment included an intention to follow up on the depression independent of the study, a belief that the patient was not depressed, or a concern that the patient’s mental health picture was too complicated to be addressed by the study’s depression care management approach.
For patients who declined to enroll, the most common reasons were not being interested in depression treatment generally or in medication specifically, wanting more time to consider whether to enroll, and facing transportation barriers to additional appointments.
For patients who consented to participate but were found ineligible, the most common reasons were past or current bipolar disorder or psychotic disorder and no current or planned antiretroviral regimen.
These results reflected multiple screens per patient. We repeated these analyses restricting attention to successive six-month periods in which screening would largely reflect unique patients and found substantively similar results. Detailed screening outcomes were not recorded at the other two study sites, but reports by study staff of enrollment experiences at those sites were similar to the results presented here.
Discussion
This study identified a high need for depression treatment at two high-volume HIV clinics, with nearly one in five screens over three years identifying a level of depressive symptoms that indicates likely untreated or undertreated depression. Yet despite the availability (supply) of a free and relatively low-burden and accessible depression treatment intervention, demand was strikingly modest. Only one in nine positive screens resulted in study enrollment. Even after excluding from the denominator screens for patients who were likely not eligible for treatment (receiving mental health treatment elsewhere, perceived as not depressed, or considered ineligible for the study), the proportion of potentially treatment-eligible screens leading to study enrollment was approximately one in five.
Some reasons for nonenrollment were study specific, such as a requirement for current antiretroviral therapy, or in all likelihood could not be modified, such as history of a bipolar or psychotic disorder that would require a different treatment approach. Other reasons for nonenrollment, however, indicated potentially modifiable barriers to engagement at the patient, provider, or intervention level. For example, in more than half of the cases in which patients declined to enroll after a positive screen, the patient attributed the decision to a lack of interest in treatment or a desire for more time to consider enrollment. A preintervention outreach component that addresses patients’ motivation for treatment could increase the reach of the depression treatment model. For example, the component could use motivational interviewing to attempt to move patients at the precontemplation stage of the Stages of Change to the action stage (
15). In one-quarter of positive screens resulting in a patient’s decision not to enroll, the patient attributed the decision to a desire to avoid taking another medication, even though the costs of antidepressants are generally not barriers for this population because of AIDS drug assistance programs and the availability of low-cost generics; an intervention that offers patients a choice of counseling and medication management could address this barrier. In addition, providers’ concerns about referring patients with more complex mental health challenges could be addressed by an integrated counseling arm flexible enough to address common co-occurring anxiety, posttraumatic stress, or substance use disorders.
Conclusions
This study is in line with many other studies that have identified a high need for depression treatment among patients engaged in HIV care. However, we found very low uptake of such care among patients with high depressive symptoms, even when study enrollment was free and the intervention represented a relatively low burden for both patients and HIV providers. Addressing modifiable barriers to engagement in depression treatment will be critical to maximize the reach of depression treatment services for HIV patients.
Acknowledgments
This study was supported by grant R01MH086362 (Dr. Pence, principal investigator [PI]) from the National Institute of Mental Health (NIMH) and the National Institute of Nursing Research, National Institutes of Health (NIH). This publication was made possible through NIH-funded programs (2P30 AI064518, John Bartlett, M.D., PI; P30 AI50410, Joseph Eron, M.D., PI) at the Duke University Center for AIDS Research (CFAR) and the University of North Carolina at Chapel Hill CFAR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the NIH.
Dr. Thielman serves as a consultant to Trius, a Cubist Company, but reports no conflict of interest with the subject matter of this manuscript. The other authors report no financial relationships with commercial interests.