Assessing pathways to psychiatric care allows a better understanding of patients’ access to care and provides valuable insight into service planning. Many studies have shown that most patients initiate help seeking through a general practitioner (GP), whereas others describe different prevalent routes of access, including direct access to psychiatric care or emergency services. According to the Goldberg-Huxley model (
1), this can be considered a bypass to care filters, with involuntary admission among the possible negative consequences (
2).
Although there is evidence of an association between social deprivation and psychiatric admissions (
3), few pathways studies have examined sociodemographic determinants, and all of them have focused on first-episode psychosis. Among other findings, these studies found that being single predicted late presentation—first contact more than one month after illness onset, for example (
2)—and that unemployment and living alone predicted involuntary admission (
4). Literature about specific pathways to admission is also predominantly focused on patients with first-episode psychosis, with few exceptions (
5,
6), and it is important to acknowledge the burden of other, nonpsychotic mental disorders, because evidence shows that any severe psychiatric illness leading to hospital admission causes considerable suffering and high treatment costs (
7).
In this study, we focused on all first-time psychiatric hospitalizations over a two-year period, with the objective of characterizing pathways to care and describing their relationship with patients’ sociodemographic features. Apart from one multicountry pathways study (
8), we found no other published studies from Portugal. This is also the first pathways study focused on first admissions, regardless of diagnosis, with sociodemographic and clinical characterization of patients for each pathway.
Methods
This study enrolled patients admitted for the first time to the inpatient unit of the psychiatric department of Hospital Fernando Fonseca, in the municipal district of Lisbon. This is a comprehensive community-oriented service and, adopting the model established by the Portuguese National Mental Health Plan in 2007, includes an inpatient unit, day treatment hospital, consultation-liaison unit, a psychiatric emergency service, four community mental health units, and two psychosocial rehabilitation facilities (
9).The psychiatric department provides care for an estimated population of 300,000 inhabitants (2011 census), which is a probable underestimate because of a large number of unregistered African immigrants. Minimum age for psychiatric admission is 16 years. Both community and hospital mental health units (including the emergency department) belong to the same trust and are financed in the same way. All units are closed on weekends, except for the psychiatric emergency and inpatient units. Patients must be admitted through the emergency department.
According to the Portuguese National Health Service rules, every citizen has the right to schedule an appointment with a GP or to seek care at a public hospital emergency department. The Portuguese mental health model is based on a gatekeeping model: referral to public mental health services must be made by a GP (most frequently), a hospital physician, a psychiatric emergency department, or a private psychiatrist. Resources are allocated so that each public psychiatric department has exclusive catchment areas. Private psychiatry is accessible to anyone who can pay for this type of care. Private psychiatric inpatient units usually do not have an emergency department, and admissions need to be scheduled.
We focused on patients belonging to the Massamá-Queluz catchment area who were admitted to the inpatient unit for the first time in 2009 and 2010. Massamá-Queluz is a predominantly urban, young, socially heterogeneous area, with high demographic fluctuation and an estimated 120,000 inhabitants.
Patients were selected from the inpatient unit database. Inclusion criteria were first-ever admission to this inpatient unit during 2009–2010 and belonging to the defined catchment area. Exclusion criteria were admission to any other psychiatric service in the past 20 years (N=5) or severe cognitive deficits (N=2). A total of 112 patients met inclusion criteria. Eleven were unreachable, nine declined, and eight were deceased, leaving 84 patients. Included and excluded patients did not differ in age, gender, or diagnosis.
Data were gathered during the first half of 2011, through interviews between patients and trained research assistants. Information about the pathways to admission was collected with a validated Portuguese translation (
10) of the Encounter Form, a World Health Organization instrument (
8). An additional semistructured questionnaire was used to obtain more detailed sociodemographic data related to time of admission. To account for missing or unreliable data, we turned to patients’ relatives, clinical records, or both.
Ethical approval was obtained from the Hospital Fernando Fonseca Institutional Review Board. All the patients gave their informed consent. Race-ethnicity was assigned by the method of self-ascription.
Diagnosis using ICD-10 criteria was defined on discharge by the inpatient unit’s psychiatrists.
Sample characterization used means with standard deviations, median, and interquartile interval for continuous variables and absolute and relative frequencies for categorical variables. Delays between symptom onset and first mental health contact or admission on the treatment pathway and associations with sociodemographic and clinical variables were calculated with the Mann-Whitney test, the Kruskal-Wallis test, and Spearman’s correlation coefficient. Statistical significance was defined at p<.05. All statistical analyses were performed with SPSS, version 15, software.
Patients were assigned to four groups, according to their pathway to care. The “emergency department only” group included patients who went directly to the psychiatric emergency department, with no mental health or primary care contact in the previous year for the current episode. The “emergency department with public GP/psychiatry” group included patients who contacted a GP, the local public psychiatric services, or both in the past year before seeking emergency treatment. The “emergency department with private/alternative” included patients who used private care, alternative medicine, or both in the past year before seeking emergency treatment. The “emergency department with all other” group encompassed “emergency department with public GP/psychiatry” and “emergency department with private/alternative” groups. Groups were compared according to sociodemographic and clinical characteristics with the use of the chi square test, Fisher’s exact test, or the linear test for trend to compare proportions and Student’s t or Mann-Whitney tests for continuous variables. Logistic regression with the backward selection procedure was used to test for confounding factors.
Results
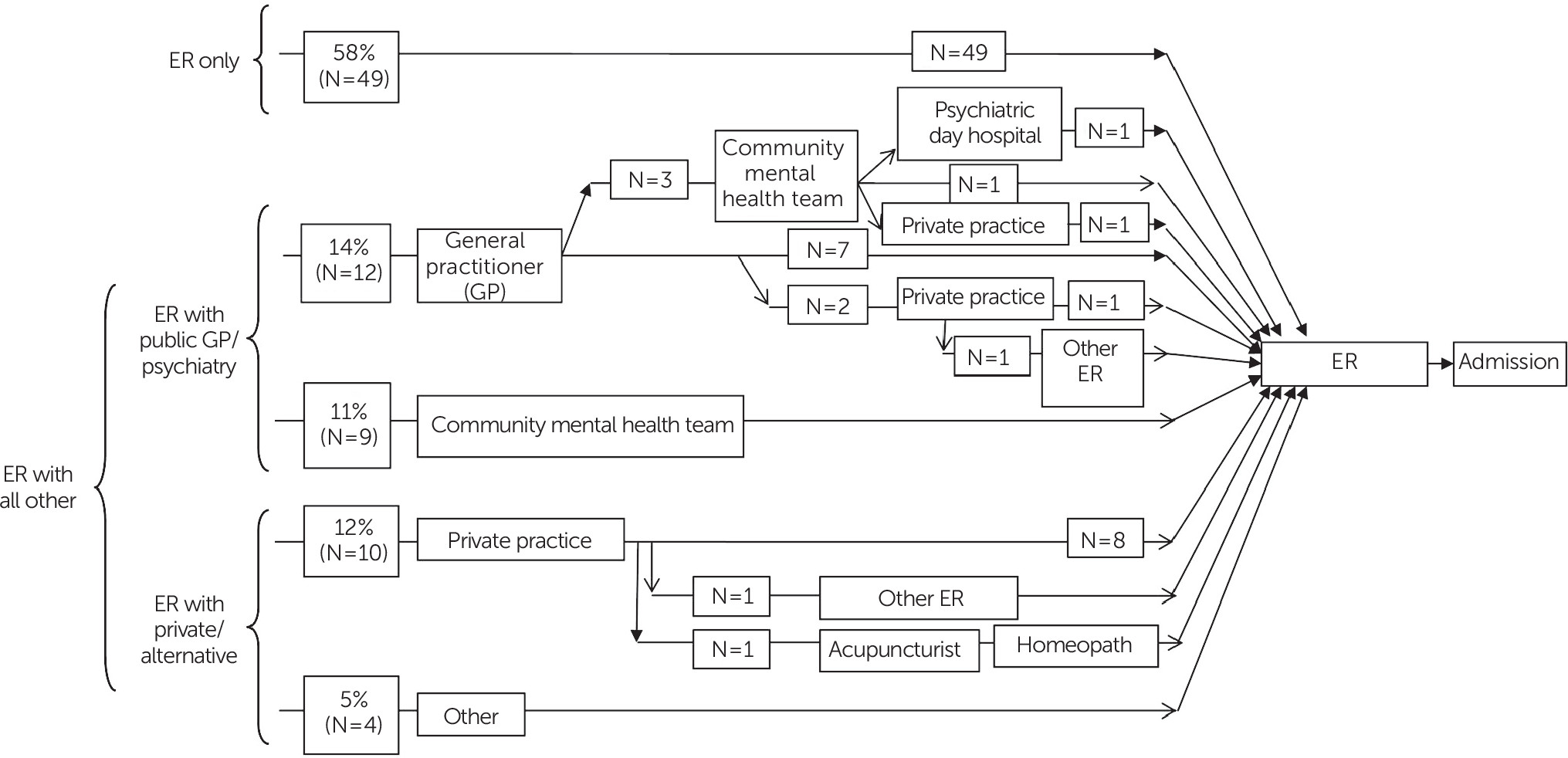
A diagram of the pathways to care is shown in
Figure 1. A majority of admitted patients made their first help-seeking contact at the psychiatric emergency department (58%). The next most common pathways were via a public GP (14%), private practice (12%), and the community mental health team (11%). Twelve patients (14%) brought to the psychiatric emergency department by the police were involuntarily admitted.
The patient’s family was the most frequent facilitator in the patient’s care seeking (N=49, 58%), followed by the previous care provider (N=14, 17%) and no one—meaning the patient sought care by him- or herself (N=12, 14%).
Symptoms were significantly associated with median delays between symptom onset and first contact (p=.001), with depressed mood (12.0 weeks, N=23) and anxiety (9.5 weeks, N=6) resulting in longer delays and disturbed behavior (1.0 weeks, N=22), psychosis (4.0 weeks, N=12), and suicide attempt (1.0 weeks, N=12) having shorter delays. The delays between symptom onset and admission showed a similar pattern of association. No significant associations were found for the other variables.
Compared with the “emergency department only” group, the “emergency department with public GP/psychiatry” patients had a significantly higher association with self-referral or referral by a care provider (with family more relevant in the “emergency department only” group), living in a house with more persons per room and more people in the household, lower chance of being involuntarily admitted, longer median delay between symptom onset and admission, and a history of contact with mental health services (unrelated to the current episode). With logistic regression, number of people living in the household was no longer significant in the multivariate analysis, after we adjusted for confounding factors (age, gender, marital status, and diagnosis).
No significant associations were found when comparing the “emergency department only” group with the “emergency department with private/alternative” group.
Compared with the “emergency department only” group, the “emergency department with all other” group was significantly associated with referral by a previous care provider or with the patient’s seeking emergency treatment directly, living in a house with more persons per room and more people in the household, higher household income, being employed, and longer median delay between symptom onset and first contact or admission. Multivariate analysis showed that only average family monthly income and number of persons per room remained statistically significant after we adjusted for confounding factors. Male gender was significantly associated with the “emergency department only” group in the multivariate analysis.
Discussion
The results confirmed that for first admissions, a large number of patients were admitted through the psychiatric emergency department without a previous contact with a public GP or any mental health service for the current episode. Also, these patients had specific sociodemographic characteristics that differed from those of the other groups. The only published pathways study in Portugal (
8) focused on new referrals to a psychiatric service and found that most patients initiated their pathway through a GP, a common finding of European studies. One of these studies (
11) additionally focused on the subgroup of patients who were later admitted and found that, in contrast to the other studies, none of the patients had contacted a primary care provider. A large sample study in Belgium (
12) found that the psychiatric emergency department was the first-ever treatment setting for one-third of patients, which is in accordance with our finding that the emergency department represents an important gateway for some patients, including those with severe illness who need hospitalization. Most specific studies about pathways to admission have focused on psychosis, but Moodley and Perkins’ study (
5) included all psychiatric diagnoses, even though most patients had previous admissions, and found a large proportion of patients who went directly to psychiatric services as well as a low level of referral from GPs.
Several reasons can explain why most patients were directly admitted through the psychiatric emergency department. Portugal’s gatekeeping model, where community mental health teams cannot be directly contacted by a new patient and where an appointment with a public GP must be scheduled several days (or weeks) ahead, might not be able to offer a quick treatment response in case of acute illness. Our hospital’s psychiatric emergency department provides immediate treatment, which, along with good accessibility, makes it a quicker and easier contact for these patients.
The studied catchment area is also known for high social inequality and high demographic fluctuation, leading to a considerable degree of disruption of social networks, impairing both the patient’s capacity to seek adequate help and the psychiatric service’s ability to detect and prevent these cases. These factors are worsened by a shortage of public GPs and insufficient human resources in the psychiatric department, with unavoidable long waiting lists for consultations and intervention.
Increasing the number of GPs in the public sector and the number of mental health workers is probably the most urgent measure to reduce filter bypass. Other measures to promote a more effective and timely intervention could include the implementation of mental health awareness campaigns and stronger collaboration with local sociocultural associations, allowing an earlier detection and referral of cases.
In addition, our analysis showed that different results emerged when we compared patients who took different pathways. A history of previous contact with mental health services and a lower chance of involuntary admission were exclusively associated with the “emergency department with public GP/psychiatry” group, underscoring the importance of easily accessible and assertive community care for patients with severe mental illness. Higher average family income was exclusively associated with the “emergency department with all other” group because it included patients using private care. Male gender was found to be associated with the “emergency department only” group compared with “emergency department with all other” group, showing that gender also influenced filter bypass.
This study had some limitations. It was an exploratory study from a single setting, the small sample size suggests that caution should be used in statistical inference, there was the possibility of recall bias because of the retrospective nature of data collection, and diagnoses met the ICD-10 criteria but no structured diagnostic interview was used.
Conclusions
The most striking feature of the pathways to inpatient care described in this report was the high prevalence of direct access to the psychiatric emergency department, with subsequent admission, showing a bypass of primary and community psychiatric care. This pathway was significantly associated with male gender, involuntary admission, referral by a family member, fewer people per room in the household, and lower probability of previous contact with mental health services for other episodes. Our findings could be the first step to improve early detection of need for mental health services and referral of patients through targeted social and clinical interventions.
Acknowledgments
This study was funded by a restricted grant from H. Lundbeck A/S. The authors thank Bruno Trancas, M.D., João Graça, M.D., Marina Martins, M.D., João Ribeiro, M.D., João Marques, M.D., and Catarina Gabriel, R.N.