Nowhere was this change more evident than in the system’s effort to reduce the use of restrictive procedures. The initial goal was to enhance safety for everyone involved and to avoid traumatizing an already highly traumatized population.
The state’s forensic services providers have also adopted the goal of recovery. Previously, the goal of forensic services was the safe custody, care, and control of the individual. The focus of treatment and discharge planning was returning the person to jail or prison. In contrast, the forensic recovery approach focuses on providing individuals with overall access to the services of the hospital system and, whenever possible, advocates for community discharge. During this ten-year span, the emphasis of forensic mental health services has shifted to teaching individuals to live safely in the community by managing their illness. Avoiding contact with the criminal justice system is considered an aspect of recovery.
Over the past 20 years, much has been written and reported about the use of seclusion and restraint within inpatient settings. Because of greater transparency governing the use of these measures, successful strategies were identified on how to decrease their use (
3,
4). However, there have also been reports that reducing the use of restraint and seclusion exposes staff to increased assaults (
5,
6). Legislative bodies in several states have challenged mental health authorities to explain how the use of seclusion and restraint in forensic settings affects the level of violence (
7–
9). Furthermore, recent news accounts suggest that a conflict exists between the treatment needs and security requirements of people served in forensic settings. This conflict has frequently ended in tragedy (
10–
12).
Seclusion and restraint use continues to be an important metric of quality in measuring the effectiveness of inpatient care. However, treatment in forensic settings is seldom examined separately from inpatient treatment overall, so it is difficult to compare the use of seclusion and restraint in forensic settings with use in other inpatient settings.
The objective of this prospective study was to assess the use of restraint and seclusion in Pennsylvania’s forensic centers and determine its effect on patient-to-patient and patient-to-staff assaults from 2001 through 2010.
Results
From 2001 to 2010, 4,805 unique individuals were served by the centers, and on December 31, 2010, the last day of the study, 12% (N=23) of the 196 individuals in the forensic centers claimed veteran status on admission.
The forensic census increased from 185 in January 2001 to 196 in December 2010. Days of care increased from 69,523 in 2001 to a high of 76,759 in 2010. A total of 4,805 people were admitted and discharged from the service, of whom 3,894 (88%) came from and were discharged to local correctional agencies. During this decade, the mean length of stay was 118 days and the median length of stay was 69 days.
The study included all 2,741 procedures used during 2,176 events with 801 unique people during the past decade. Of the 2,176 events, 565 were complex, requiring the use of more than one procedure type.
The frequency of use and duration of containment procedures declined during the 120 months of this study (
Table 1).
Of the 801 unique people for whom a containment procedure was used, 447 were involved in one-time events. Ninety-seven individuals were involved in five or more containment events, and 11 were involved in 20 or more events.
Mechanical Restraint
The high point for the use of mechanical restraint was 2002, when it was used 1.7 times per 1,000 days, for a total of 372 hours. By 2010, its use had significantly declined to .04 episodes per 1,000 days and lasted a total of two hours (p<.001). The mean±SD minutes in restraint declined significantly, from 191 minutes per event in 2002 to 39 minutes in 2010 (p<001).
Seclusion
In 2001, there were .89 episodes of seclusion per 1,000 days, for a total of .95 hours per 1,000 days. By 2010, seclusion was used only three times, for a total of 1.6 hours. The time spent in seclusion declined significantly, from 69 minutes per event in 2004 to 32 minutes in 2010 (p<.001).
Physical Restraint
Physical restraint use declined during this span. In 2003, it was used 4.28 times per 1,000 days, and by 2010 it was used 3.09 times per 1,000 days. However, the average duration in physical restraint increased from 3.8 minutes in 2002 to 6.5 minutes in 2010.
Proximal Cause
Following each incident, staff reported the immediate cause that resulted in the use of a containment procedure. During this study, 4,440 assaults were reported statewide in the forensic centers to the risk management system. However, only 25% (N=1,102) resulted in the use of a containment procedure.
Of the 2,176 events involving the use of a containment procedure, aggression, defined as threatening another, was the leading reason for the use of a containment procedure, accounting for 36% (N=777), followed by patient-to-staff assaults (30%, N=653), patient-to-patient assaults (21%, N=449), and self-injurious behavior (7%, N=157).
Injuries
State policy requires that an individual who is subject to a containment procedure be examined for injuries following the use of the procedure. The most severe injuries attributed to the use of containment procedures were lacerations requiring the use of sutures, reported in 17 incidents (.8%). Injuries involving bruises or skin abrasions were reported in 13% (N=288) of the events, and 79% (N=1,716) resulted in no injury.
Assaults
Pennsylvania’s assault data were first publicly reported in September 2003 at the request of union leadership (
17). There was concern that the declining use of containment procedures had increased assaults. During this study, an assault was defined as any aggressive act by a patient involving physical contact with another person that may or may not result in injury (
18).
Between 2001 and 2010, more than 34% of assaults (N=1,685 of 4,945) involved an injury. Patient-to-staff assaults resulting in staff injury accounted for 6% (N=310) of all assaults, and patient-to-patient assaults resulting in patient injury accounted for 28% of assaults (N=1,375).
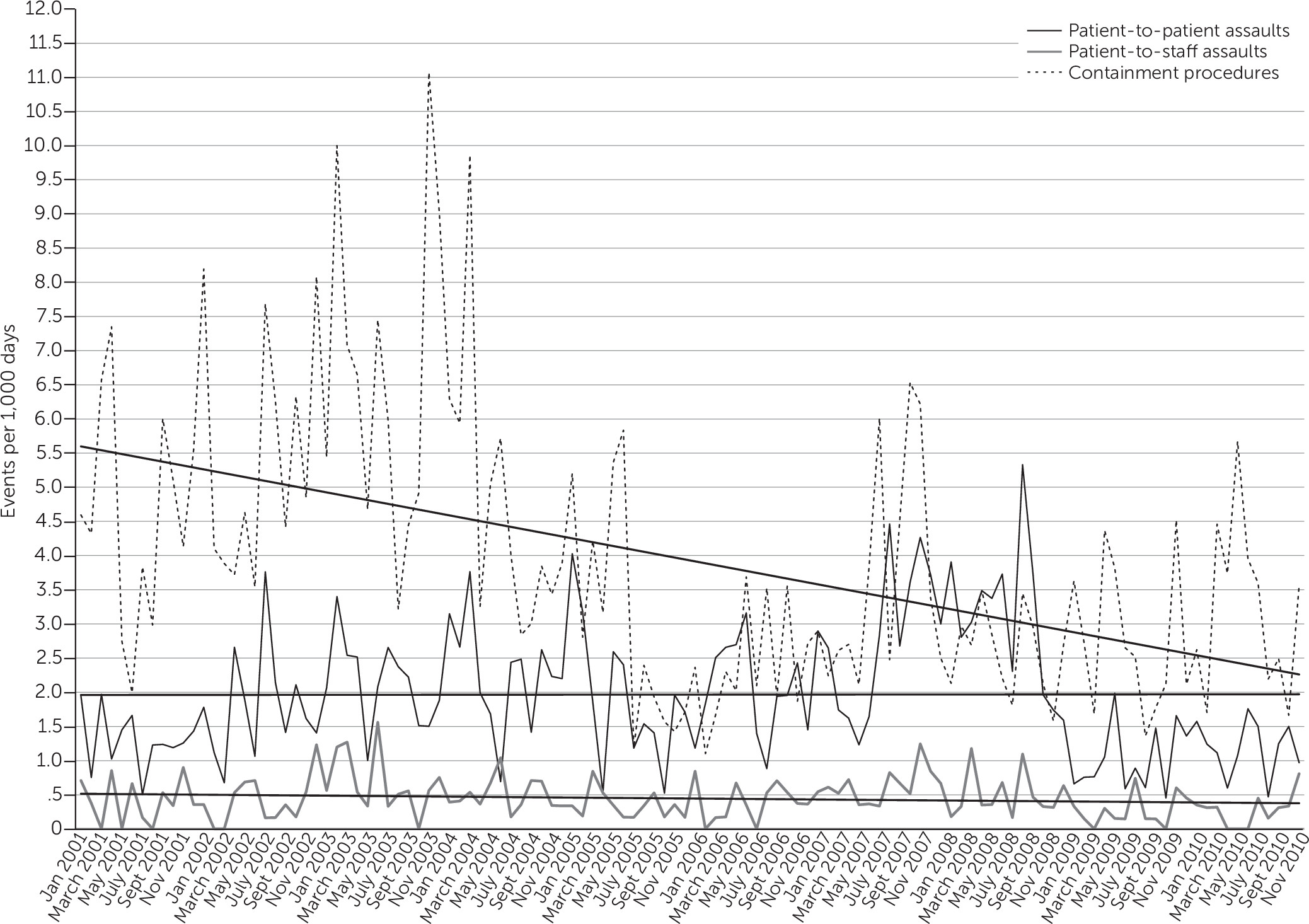
During this study, the mean rate of patient-to-patient assaults resulting in patient injury did not change (1.95 per 1,000 days) (
Figure 1). However, the rate of patient-to-staff assaults resulting in staff injury declined from .5 per 1,000 days in 2001 to .4 per 1,000 days in 2010.
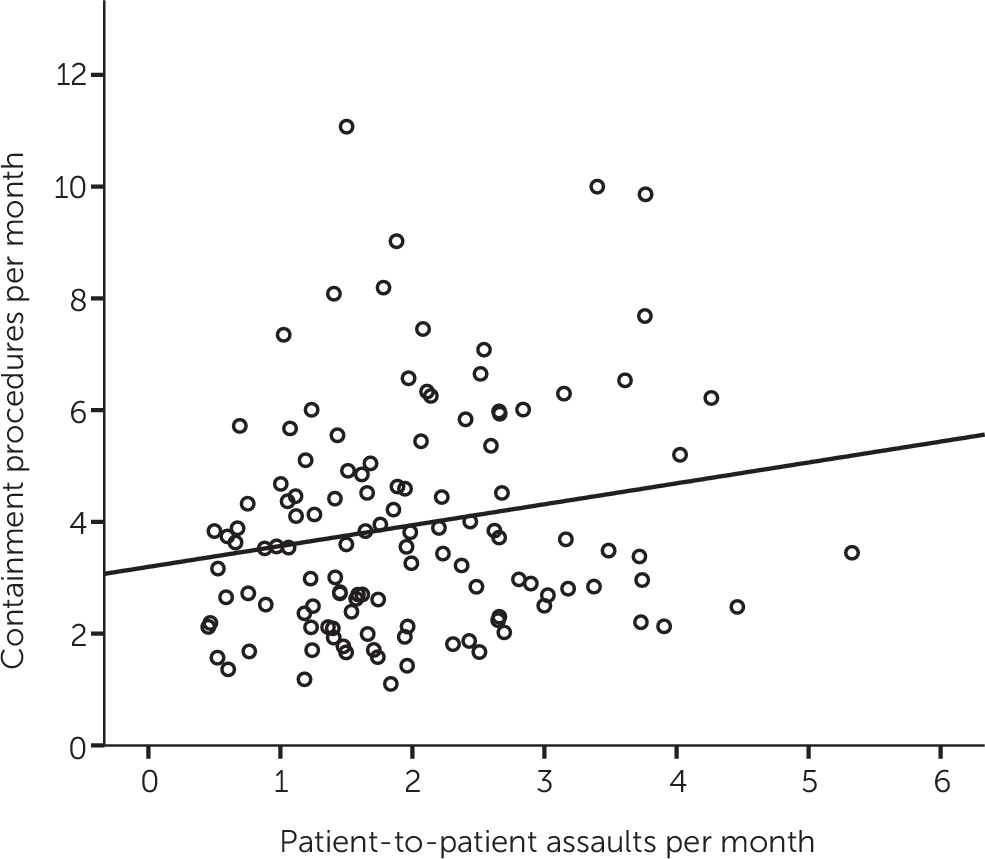
A correlation analysis of these data showed a positive association between the rate of patient-to-patient assaults and the declining use of all containment procedures (r=.223, N=120 months, p<.02) (
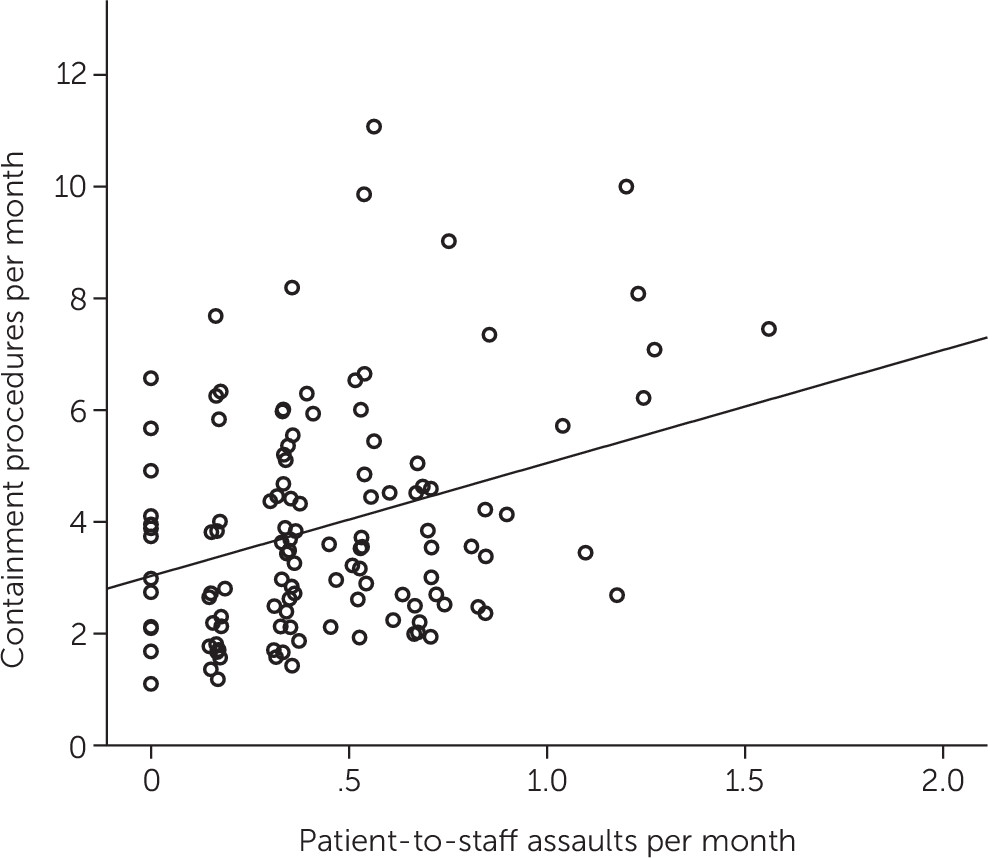
Figure 2). Similarly, a stronger, positive association was shown between the declining rate of patient-to-staff assaults and the declining use of containment procedures (r=.334, N=120 months, p<.001) (
Figure 3).
The analysis also showed a wide variance in the use of procedures in response to an assault. A procedure was used in 75% of patient-to-staff assaults (N=653 of 870) versus 13% of patient-to-patient assaults (N=449 of 3,570).
Unscheduled Medication Use
Starting in March 2004, the centers began reporting unscheduled use of medications for psychiatric indications. Unscheduled medications were defined as any medications given by PRN or provided by stat physician’s order (
19). During March 2004 the centers administered 112.5 unscheduled medications per 1,000 days (N=646) (mean=112.5±78). By March 2006, statewide use of unscheduled medications had declined to 18.6 per 1,000 days (N=108) (mean=18.6±.8). Per state policy, effective March 2005, the centers discontinued the use of PRN orders for psychiatric indications and required that stat orders be predicated upon an examination by a physician (
19,
20).
Treatment Changes
Following any containment incident, a psychiatrist is required to review the patient’s treatment plan (
18). In 999 (46%) of the 2,176 events involving the use of a containment procedure, counseling, education, or patient debriefing was added to the treatment plan; a medication change occurred in 19% (N=405) of the events. Placing a patient under greater supervision was ordered in 22% (N=70) of events involving the use of seclusion (N=317), compared with 9% (N=163) of events involving physical restraint (N=1,932) and 17% (N=86) of events involving mechanical restraint (N=492). Differences noted here are attributed to safety concerns for the patient and peers. Information from the debriefing process was not fully recorded until 2003.
Diagnostic Differences
Of the 4,805 people served by forensic services during this study, 49% (N=2,341) had an axis I diagnosis of schizophrenia or psychotic disorder. This group accounted for 53% (N=1,155) of the events reported. People with a mood disorder diagnosis (all subtypes) represented 23% (N=1,088) of the population served by the forensic service and accounted for 24% (N=532) of the events reported. People with intellectual disabilities, who represented .25% (N=12) of the population, accounted for 9% (N=204) of the events reported and 86 hours of total use.
Gender Differences
During this decade, 915 women and 3,890 men were served in the centers. Of the 915 women, 19% (N=175) were restrained or secluded, accounting for 616 of the procedures used. Of the 3,890 men, 16% (N=627) were restrained or secluded, accounting for 1,560 procedures. Overall, the variation in rates of exposure (N=3.52 events per woman and 2.48 events per man) are attributed to differences in acuity and responsiveness to treatment during the first month following admission to the forensic service.
Racial and Ethnic Differences
During this study, participants in forensic services represented more than six different racial and ethnic groups, including 2,775 whites (58%), 1,744 blacks (36%), and 235 Hispanics (5%). Whites accounted for 1,151 (53%) of the events reported versus 872 (40%) for blacks and 126 (6%) for Hispanics.
Overall, whites were held the longest in mechanical and physical restraint (35±11 minutes, compared with 24±11 minutes for blacks and 13±11 minutes for Hispanics). However, when the 492 episodes of mechanical restraint were examined separately, the differences widened. Whites, on average, were held for 141±63 minutes, compared with 85±63 minutes for blacks and 15±63 minutes for Hispanics. In regard to seclusion, which was used 317 times during the study, whites were held for 57±1 minutes, compared with 56±1 minutes for blacks. In regard to physical restraint, which was used 1,932 times, whites were held for 5±1 minutes versus 4±1 minutes among blacks and Hispanics.
Day of Week, Work Shift
This study also examined whether use of containment-related events differed by day of the week and work shift. Use was highest on Thursdays, accounting for 17% (N=366) of the episodes reported. The fewest episodes occurred on Saturdays, which accounted for 9% (N=190) of the events reported.
Most episodes of containment occurred on the first shift, from 7:00 a.m. to 3:00 p.m., accounting for 50% (N=1,088) of the episodes reported. The second shift, from 3:00 p.m. to 11:00 p.m., accounted for 44% (N=960) of episodes, and the third shift accounted for 6% of episodes (N=127).
Age and Length of Stay
Nearly half of all events, 47% (N=1,026), involved people between the ages of 20 and 29. People between the ages of 18 and 21 accounted for 14% (N=299) of the events reported.
During this study, 14% (N=304) of the events reported occurred within the first week of admission, and 41% (N=903) occurred within the first 30 days of admission.
Discussion
This study confirms findings related to the reduction in use of containment procedures in Pennsylvania’s civil hospitals and thus extends the efficacy of Pennsylvania’s approach to the use of containment to a forensic population (
21).
These results are in marked contrast to reports that efforts to reduce seclusion and restraint utilization were met with increases in patient-directed assaults, leading to the conclusion that such initiatives are “not without risk” (
6).
The major difference between this study and the study quoted above is that our findings are associated with the use of an approach for over a decade (
6). Perhaps the most important feature of the study, however, is Pennsylvania’s emphasis on staff training and focus on deescalation techniques.
In recognition of the risks associated with changing the use of containment procedures, Pennsylvania referred to its new initiative as a “cultural transformation.” The foundational core behind this change was to support the recovery of individuals served and safety. Nevertheless, when a historical practice becomes less readily available, it may lead to “staff frustration” (
6) and overreporting of the incidences of violence. To address these concerns, staff were encouraged to “over-report/report every incident” to assure the hospital community that leadership wanted to ensure data integrity, maintain transparency, and respond when challenged about the efficacy of each intervention.
These changes also accounted for, in part, the decreases reported in patient-to-staff assaults resulting in injury, given that any use of a procedure is a violent act that is difficult to control, resulting too frequently, regardless of the precautions taken, in physical or emotional injury. Over time, decreasing the use of containment procedures led to decreases in patient-to-staff assaults resulting in any injury.
The ongoing effort to reduce the use of these procedures can result in clinical environments that provide safety and support to the entire community without further traumatizing the individuals served and their caregivers.
In addition to providing workforce training, this effort included the development of response teams that assured an organized intervention to a crisis. Discontinuing the use of PRN orders for psychiatric indications in 2005 was pivotal because it decreased the likelihood of using medication as a chemical restraint (
20).
Policy changes were essential because they unified and limited the use of these procedures. They also ensured that the use of restraint or seclusion was the last resort in supporting a person in crisis.
Using data at all levels of the agency was a fundamental change that enabled the monitoring of performance by unit and patient. Clinical alerts were a valuable tool that raised attention to specific individuals who were receiving high amounts of medication or engaging in frequent assaults.
Our analyses of the reasons for the use of containment procedures were limited to the proximal cause. The study did not assess the underlying rationale that may have led to the use of a containment procedure nor how this information was used to reduce patient aggression. Future studies on restraint reduction should evaluate the effectiveness of this proactive process and how it is used to reduce patient aggression.
This study also showed that patient-to-patient assaults were unaffected by changes in the use of containment procedures.
Using data to identify periods of high activity for assaults on individual units and use of procedures by work shift and to adjust routines accordingly should have a positive effect on reducing aggression. Forensic staff should be proactive in this regard and use historical data as a tool to plan for a safe environment. In addition, applying information obtained during the initial patient assessments can help develop personalized crisis plans for people who have significant histories of violence.
Acknowledgments
The authors thank the security staff, nurses, doctors, and program services staff who work in the Pennsylvania forensic service. Their support of the nonrestraint approach to psychiatric care and services is sincerely appreciated. The authors also recognize the state hospital performance improvement staff for their contributions to the data reported here and John Deegan, M.S., for his assistance. They also gratefully acknowledge the work and leadership of Charles G. Curie, M.A., A.C.S.W., George A. Kopchick, M.S., Bonnie Hardenstine, B.S., Roberta J. Altenor, M.S.N., Louise A. Cochenour, R.N., Jeffrey Darling, R.N., Hannah Fry, R.N., Marcie Hepner, M.S., John Pedrazzani, M.S., and Gail Vant Zeldfe, Ph.D.