In response to the large proportion of persons with chronic mental illness cycling through the criminal justice system, court officials in jurisdictions throughout the United States, Canada, and Australia have established mental health courts (MHCs) with separate dockets and periodic status hearings (
1–
4). Like other problem-solving courts, MHCs attempt to change offending behavior by addressing its underlying causes. A team of legal and clinical professionals create a treatment and service plan for each defendant who volunteers for MHC. During the MHC program (usually 12–18 months), the team monitors compliance, giving encouragement, support, and sanctions and, at times, making plan adjustments, to assist behavior change. If participants comply with court mandates, their criminal charges are dropped or their sentences are negated, depending on whether they entered the MHC program pre- or postadjudication (
2,
5).
Studies of MHCs have found that they achieve their primary goal, reduced criminal recidivism, reporting that participants are less likely to offend after than before entering an MHC (
2,
6–
16) and are either less likely or no more likely than comparison groups to reoffend (
2,
7–
9,
12,
15–
19). Most of these studies have examined recidivism after MHC entry for a limited follow-up period when defendants were still in the MHC program. This time frame is problematic because the behavior patterns that MHCs try to modify are long established; indeed, MHC teams expect participants to lapse into old ways, and thus they continue to work with participants (
2,
14,
20,
21). Most participants who reoffend while in an MHC program do so early in the program, but many ultimately change their behavior and complete the program (
9,
12); thus, arrests during MHC participation do not necessarily represent failure.
Seven studies have followed defendants after MHC exit (
6,
8,
9,
11,
12,
14,
19). All have reported reduced recidivism, but because of methodological problems in their designs, effectiveness after MHC exit remains in question. With one exception (
12), these studies had no measure of prior criminal offending, no comparison group of offenders with mental illness, or no follow-up of noncompleters. With one exception (
12), studies with a comparison group had no control for treatment and services. Whereas mental health treatment and services are integral to an MHC program, comparison groups may receive minimal or no treatment. Thus these studies do not allow us to discern whether treatment and services brought change in participant behavior or whether the MHC process—that is the legal procedures, team approach, monitoring, sanctions, support, and encouragement—made a significant difference in that change (
21–
24).
Here we report on a study that addressed two unanswered empirical questions. Can MHC participation lead to reduced criminal recidivism (below the pre-MHC level) for an extended period after participants leave the MHC program? Is recidivism of MHC participants after they leave the program less than that of comparable defendants with mental illness in traditional criminal court (TCC) who are provided individualized plans from the same package of supervision, case management, and services from the same pretrial services agency and community professionals? The study is important not only because it addressed these unanswered questions but also because it constituted a longer postexit follow-up (two years) than all but two other studies (
14,
19) and examined a court designed to be of shorter duration than other MHCs (six months versus 12–18 months) that deals solely with misdemeanors, the most common offenses of persons with severe mental illness (
25).
Methods
Setting
The study MHC, which serves the District of Columbia, accepts arrestees with severe mental illness who are competent, are charged with misdemeanors, and have no pending charge or conviction in the prior five years of a dangerous or violent felony. The MHC monitors participants for treatment and behavior compliance at monthly status hearings. When participants demonstrate four to six consecutive months of substantial compliance with court mandates, they graduate and have their charges dismissed. Those who repeatedly fail to meet court mandates are returned to TCC for adjudication.
Unlike most MHCs, this court benefits from a federal pretrial services agency that screens all arrestees for severe mental illness the day after arrest and dedicates a specialized services unit (SSU) to provide individualized supervision and services (case management and linkage to mental health service agencies, plus drug testing and treatment for participants with co-occurring mental and substance use disorders) during pretrial release to persons who screen positive, whether their cases are diverted to the MHC or remain in TCC. On receiving an MHC-eligible defendant, an SSU case manager is expected to refer that person to MHC shortly thereafter.
The study MHC follows the basic procedures of most MHCs that distinguish them from TCCs (
2,
5). The judge engages defendants in ensuring that they understand the process, especially its voluntary nature and the treatment and behavior mandates, and in discussing their progress or lack thereof. The judge, as well as the MHC team, is supportive, encourages behavioral changes, and focuses on problem solving rather than on offenses and adjudication of guilt (
9,
12,
21,
24,
26).
Comparison Group
Controlling for possible confounders, we compared recidivism over two years between MHC participants after they left the MHC program and MHC-eligible defendants in TCC who were also under SSU supervision on pretrial release and who received individualized plans from the same package of services and supervision from the same pretrial services and community agencies. We hypothesized that MHC participants would have fewer arrests in the two years postexit than they did in the two years prior to their key arrest and that they would have lower recidivism than the comparison group. We also hypothesized that MHC completers (graduates who fulfilled their individualized mandates) would have lower recidivism than noncompleters (those ejected for noncompliance with court mandates or who chose to opt out) because completers get a “full dose” of MHC (
2).
Data Collection
We used administrative data from the pretrial services agency for MHC participants (N=408) and MHC-eligible defendants (N=687). The comparison group was defined as all misdemeanor arrestees who screened positive for severe mental illness, who did not have a recent (current or past five years) violent or dangerous felony charge or current domestic violence charge, who were released pretrial to SSU during the first two years of the MHC’s operation (October 2007–November 2009), whose cases were not disposed of by another diversion court, and who had complete data. Because of data availability, our violence and dangerous criterion for the comparison group was broader than that for the MHC participants (charge rather than conviction), yielding a more conservative estimate of recidivism for the TCC sample. From the MHC sample, we excluded those sent back to TCC at their first MHC hearing (N=37); those who did not attend their first MHC hearing (N=3); and those who had administrative case closures because of death, sickness, or other reasons (N=6) (final sample N=408). Data included sociodemographic, court supervision, and arrest information (in the District of Columbia) from two years before the key arrest that brought each person into the sample through two years after disposition of the key arrest in the MHC or the TCC. MHC judges’ records on processing participants supplemented these data. The institutional review boards of the two universities ((North Carolina State University and Georgetown University) as well as the pretrial services agency and the MHC judges approved the research.
Measures
The dependent variable was postexit recidivism, measured over the two years after the key arrest disposition (for MHC completers, the key arrest disposition occurred at exit from the MHC). The four measures were any rearrest, number of rearrests, any felony arrests, and time to rearrest. We excluded from postexit recidivism any rearrests that occurred after the key arrest but before court exit or court disposition. These rearrests occurred before our follow-up period; in addition, the MHC in this study often forgives such rearrests as slip-ups. However, we employed these rearrests as predictors of postexit recidivism, because they indicated noncompliance with MHC mandates and continuation of old behavior. We did not count the key arrest among the prior arrests. To predict recidivism in multivariate models that controlled for possible confounders, we employed logistic regression. To predict time to rearrest, the Cox proportional hazards model was employed. Possible confounders included sociodemographic variables (age, gender, and race), illegal drug use (a positive screen for illegal drugs at the first check-in with the case manager), prior arrests (in the two years before the key arrest), and any predisposition arrest (that is, between the key arrest and court disposition).
Results
Sample Description
The MHC and TCC groups were similar in age (MHC, 41.4±10.99; TCC, 40.7±11.63). The TCC group had a larger proportion of men, compared with the MHC group (N=435, 63%; and N=204, 50%; χ
2=18.69, df=1, p=.001). Among MHC participants, 90% (N=367) were African American, and 10% (N=41) were white. Among TCC participants, 93% (N=636) were African American, 7% (N=48) were white, <1% (N=2) were Asian, <1% (N=1) was coded as other. The groups differed in prior criminal offending. A larger proportion of the TCC group tested positive for illegal drug use at first check-in (N=439, 64%, compared with N=220, 54%; χ
2=10.64, df=1, p=.001). Also, as shown in
Table 1, the TCC group had more arrests than the MHC group in the two years before the key arrest (2.32 versus 1.76; t=5.31, df=1,093, p=.001).
Among MHC participants, completers (N=238) and noncompleters (N=170) were similar in sex and age, but noncompleters differed significantly by race. Among noncompleters, the proportion of whites was lower than among completers (N=7, 4%, compared with N=34, 14%; χ
2=11.34, df=1, p=.001). In addition, a larger proportion of noncompleters tested positive for illegal drug use at first check-in (N=131, 77%, compared with N=89, 37%; χ
2=62.79, df=1, p=.001). As shown in
Table 1, noncompleters also had more arrests than completers in the two years before the key arrest (1.92 versus l.64, t=2.19, df=406, p=.033). A larger proportion of noncompleters than completers had a drug offense as their key arrest charge (N=79, 47%, compared with N=85, 36%; χ
2=4.77, df=1, p=.029).
Recidivism
Table 1 presents a pre- and postarrest comparison for the TCC group and MHC completers and noncompleters. In each group, most participants were not rearrested. However, MHC participants were significantly less likely than TCC participants to be rearrested in the follow-up period (38% versus 48%; χ
2=10.99, df=1, p=.001). The mean number of rearrests was significantly lower in the MHC group compared with the TCC group (.75 versus 1.16; t=4.27, df=1,093, p=.001). Most rearrests were misdemeanors; less than 15% of either group was arrested for a felony, and the difference between the groups was nonsignificant (not shown).
In all groups, a significant decline in the average number of arrests was noted—from over two in the two years before the key arrest to less than one in the two years after court exit or court disposition. At the two-year follow-up, the proportion rearrested was smallest among MHC completers (25%), and this group also averaged the lowest number of rearrests (.42), whereas noncompleters had the largest proportion of rearrested participants (55%) and the highest mean number of rearrests (1.21). These findings indicate that the completers were responsible for MHC participants’ having a significantly smaller mean number of arrests than the comparison group.
Multivariate Analysis
Because of differences between samples, we controlled for possible confounding variables with logistic regression to determine whether MHC participants had lower two-year recidivism rates than the TCC group. We first modeled the effect of MHC participation on odds of rearrest and then sequentially added three sets of possible confounders: sociodemographic variables of age, gender, and race; criminogenic factors of illegal drug use and number of prior arrests; and the process variable of any predisposition arrest. Models comparing the full MHC and TCC samples (not shown) indicated that when the models did not control for confounding variables, the MHC participants were less likely (odds ratio [OR]=.66, p<.001) than the TCC sample to be rearrested in the two years after court exit or court disposition. When the models controlled for sociodemographic variables, the MHC participants continued to have lower odds of rearrest (OR=.69, p<.004). However, MHC participation lost significance as a factor in rearrest in subsequent models that added illegal drug use, number of prior arrests, and any arrest between key arrest and court disposition.
Table 2 presents the same logistic regression analyses but with MHC participants separated into completers and noncompleters (the reference group is the TCC group). The first model shows that MHC completion made an even larger difference than MHC participation in lowering the odds of arrest after court exit. Compared with the TCC sample, completers were approximately two-thirds less likely (OR=.37) to be rearrested, whereas rearrest among noncompleters was not significantly different compared with TCC defendants. In each subsequent model, MHC completion maintained its significant effect. By the final model with all confounders included, completers were significantly less likely (OR=.52) than the TCC sample to be rearrested. Older participants and female participants were significantly less likely than younger and male participants to be rearrested, and each arrest in the year before the key arrest and any predisposition arrest increased the likelihood of rearrest. Illegal drug use was not a significant predictor of rearrest. Noncompletion of the MHC program became a significant predictor of rearrest in the third and fourth models, increasing the likelihood of arrest over that of the TCC group.
We found similar results explaining differences in time to rearrest after court exit or court disposition. Controlling for predictor variables from the final logistic regression models, Cox regression analysis indicated that MHC participation alone was not significant but that completion was significant (hazard ratio=.58, p=.001).
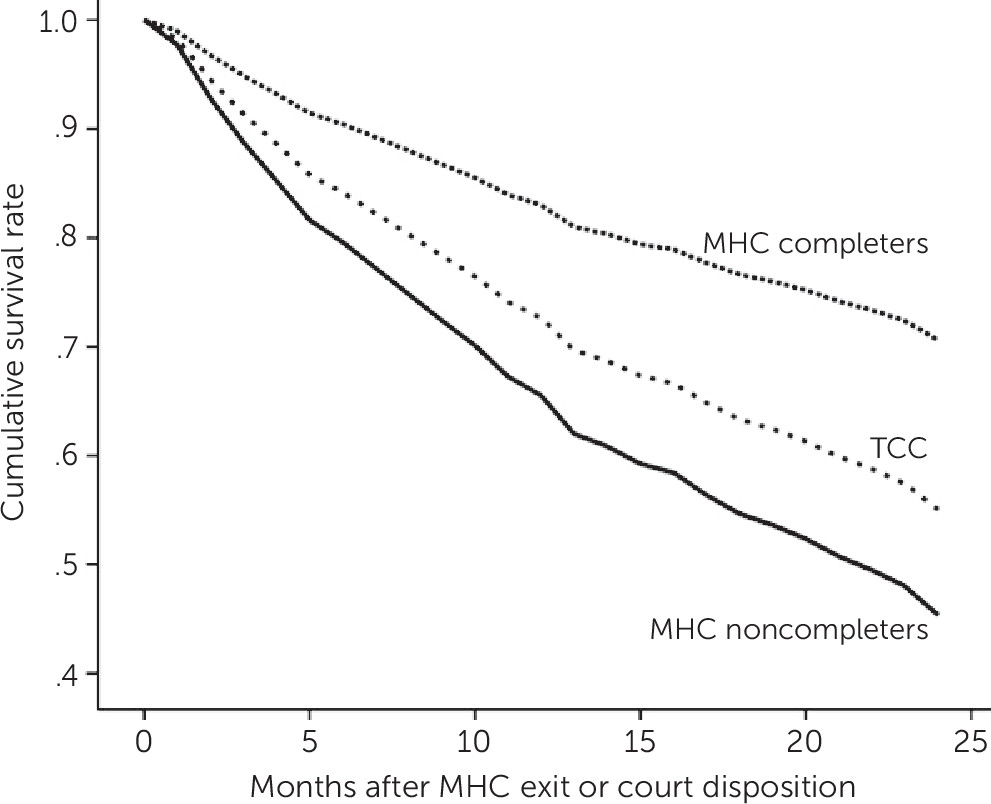
Figure 1 shows the estimated cumulative probability of rearrest at specified intervals for MHC completers and noncompleters and the TCC group. MHC completers had the longest time to rearrest, whereas the TCC group had a significantly shorter time and MHC noncompleters had the shortest. The distance between curves is the estimated postdisposition positive effect of MHC completion at any time point; thus, at 18 months, for example, 20% of completers had been arrested, compared with 47% of noncompleters and 40% of the TCC group.
Discussion
This study advances understanding of the effects of MHC participation on recidivism by examining an MHC with short maximal monitoring and by following for two years after MHC exit a large sample of MHC participants charged with misdemeanors, the most common offenses of defendants with mental illness. Findings for the number of rearrests, proportion rearrested, felony arrests, and time to rearrest two years after exit from an MHC suggest that reports in previous studies of a reduction in criminal offending after MHC entry may continue for two years after participants leave the MHC program, even though individuals are no longer under its supervision and no longer receiving benefits of encouragement, supports, treatment, and services.
This study also advances understanding of the effects of MHCs on recidivism by using data to address the major competing explanation for recidivism reduction: receipt of treatment and services. It did so by comparing recidivism among MHC participants and a large sample of MHC-eligible defendants in TCC in the same jurisdiction who were provided individualized plans from the same package of case management, substance abuse and mental health treatment, and other services from the same professionals. Both groups showed reduced recidivism in the two-year follow-up, indicating the effects of treatments and services. Declines in recidivism were greater among MHC participants, but when the analysis controlled for past offending and drug use plus rearrest during the MHC program, differences between the two groups disappeared. Only when MHC participants were divided into completers and noncompleters did we see significant effects of MHC participation on recidivism beyond that of the TCC group when the analysis controlled for confounding variables.
For the many MHCs that serve only defendants with misdemeanors, these results suggest that they can be effective when using monitoring schedules of shorter duration and fewer court hearings. But it must be emphasized that this study’s MHC provided treatment and services. Its case management and substance abuse treatment, plus linkage to community agencies for mental health treatment and social services, represent more resources than many MHCs can deliver. Nevertheless, team members spoke of the inadequacy of services to address all participants’ criminogenic conditions (
25,
27), especially insufficient housing options for homeless participants.
The major criticism of MHCs is that they are unnecessarily coercive and that provision of adequate treatment and services could prevent offending without MHC involvement (
28). All three groups in this study experienced a decline in arrests after provision of treatment and services; however, because MHC completers had a significantly greater decline, the findings suggest that the MHC itself can have an additional impact. It could be argued that treatment and services were not equivalent for the MHC and TCC groups. Here it is necessary to distinguish between providing and receiving treatment and services. TCC defendants were offered individualized plans from the same package as the MHC defendants; however, they were not in the MHC program because they were unwilling to be subject to its control or because of their early noncooperation with case managers. Therefore, an unknown proportion of TCC defendants were unlikely to have participated to the same extent as MHC participants in treatment and services. Furthermore, TCC defendants did not have regular MHC hearings, with monitoring, encouragement, and support designed to assist them in overcoming obstacles to treatment adherence and cooperation with the law. Nonetheless, unlike other MHC evaluations in which unknown or little treatment and services were provided to the comparison group, this study’s comparison group was provided case management, individualized treatment plans, and linkage to community treatment and services equivalent to those for MHC participants.
MHC noncompleters experienced the MHC program for only a short time. Like TCC defendants, they probably did not receive the same treatment and services as completers because of their unwillingness to follow or comply with mandates. Noncompleters may have done worse than MHC-eligible TCC defendants because noncompleters included a substantial proportion who entered the MHC program only to avoid punishment. We observed that these recalcitrant persons either opted out of the MHC program when they realized that their activities would be constrained or were ejected after monitoring revealed violations of court mandates. Noncompliance leading to early exit meant loss of MHC supervision and support, and these persons were less likely to participate in treatment and services.
Like almost all MHC studies, the current study was of a single court, albeit one with the essential elements of an MHC (
29). At the same time, it had components, notably short duration and in-house case management and drug treatment, that are not present in most other MHCs. Therefore, care should be taken in making generalizations. Like most studies of diversion programs, there was no random assignment. Thus MHC participants were likely subject to selection bias among team members who perceived them to be more cooperative and ready to change (
12,
23,
30,
31). In addition, because of the voluntary nature of MHC participation, participants were likely to be more willing to accept treatment and supervision and more motivated to change. However, as noted above, we observed that some participants in this and other MHCs seemed to enroll only to avoid criminal charges and possible incarceration and did not count on close supervision. Although we were able to control for differences in sex, substance abuse, and criminal history in multivariate analyses, we could not control for these sources of bias. Similarly, selection bias occurred in the division of the MHC sample into completers and noncompleters (
32–
34).
Conclusions
This study adds to the accumulating evidence that MHCs meet their major goal, reduction of criminal recidivism, and that reductions can extend beyond court exit and may result from more than the provision of treatment and services. Elements of MHCs that lower recidivism are only beginning to be explored. Researchers have proposed procedural justice (
22,
24,
29,
35,
36), reintegrative shaming (
21), and therapeutic jurisprudence (
23) as mechanisms. Some empirical work has supported the effectiveness of those processes (
21,
23,
37), but more needs to be done to understand how MHCs work if we are to structure them not only to reduce recidivism but also to improve the lives of persons with severe mental illness.