Substance use disorders are prevalent among persons living with HIV/AIDS (
1). Use of illicit drugs and alcohol can increase sexual risk-taking behaviors (
2), reduce adherence to antiretroviral therapy (
2,
3), and decrease the likelihood of accessing or using HIV-related care (
4).
Nearly 20% of HIV-positive individuals are not aware they are infected and thus are at greater risk of spreading the disease (
5,
6). To enhance early identification and treatment of the virus, several U.S. public health agencies have called for increased integration of substance abuse treatment with specialized services for HIV/AIDS (
7). However, many barriers to integrating HIV services into substance abuse treatment have been cited (
8), including limited funding, lack of therapist training for working with persons with comorbid conditions, high therapist caseload and turnover, stigmatizing attitudes among staff and self-stigma from clients about HIV, and negative interactions between medications for substance abuse treatment and antiretroviral medications (
9).
The degree to which substance abuse treatment facilities are moving toward integrating HIV services into substance abuse treatment remains unknown. Using a national survey of over 13,000 substance abuse treatment facilities in the United States, we examined the prevalence of facilities that do and do not offer specific HIV services and the organizational factors associated with the provision of these HIV services. Identifying factors that are correlated with the provision of HIV services in substance abuse treatment facilities will direct stakeholders to areas for improvement so that significant gaps in prevention and treatment needs can be addressed.
Methods
Data were drawn from 13,720 eligible facilities participating in the 2011 National Survey of Substance Abuse Treatment Services (N-SSATS), which is a survey of public and private substance abuse treatment facilities in the United States conducted annually by the Substance Abuse and Mental Health Services Administration (SAMHSA) and made publicly available. More information about the sampling methodology and procedures is available on the SAMHSA Web site (
www.samhsa.gov/data/substance-abuse-facilities-data-nssats).
Outcome measures included whether the following four HIV services, as noted in the N-SSATS questionnaire, were offered at each facility (yes-no): HIV testing; early intervention for HIV; HIV/AIDS education, counseling, or support; and specially designed substance abuse treatment program or group exclusively for persons with HIV or AIDS.
Correlates were selected from previous studies that used the N-SSATS data and from correlates known to be associated with HIV services (
1,
2,
10,
11). These included primary treatment focus of the facility (substance abuse treatment, mental health, or both), private versus government operated, regional location (Northeast, Midwest, South, West, or U.S. jurisdiction or territory), setting and service-related factors (providing methadone, hospital inpatient and outpatient treatment services, and number of non-HIV ancillary services), funding source (accepts government insurance, including Medicaid, Medicare, or government earmarks; offers no-charge or free treatment), and licensing authority (licensed by a mental health department, licensed by a state health department, and licensed by a state substance abuse treatment agency).
Prevalence estimates of the four separate HIV services and the overall provision of any HIV service were calculated. Separate multivariable logistic regression models were used to examine each HIV service and calculate the adjusted odds ratios and 95% confidence intervals. Statistical significance was set to α=.05. Correlations between all variables were examined, and in cases where two variables were moderately (r≥.50) and significantly correlated, only one was assessed in the adjusted model. Variables that improved the model fit based on the Akaike information criterion were included in the fully adjusted model. With this approach, the four adjusted models differed according to which variables were included. Statistical analyses were performed with SAS, version 9.3.
Results
Prevalence estimates indicated that 28% of facilities offered HIV testing; 26% offered HIV early intervention; 58% offered HIV/AIDS education, counseling, or support; and 8% offered special HIV/AIDS programs.
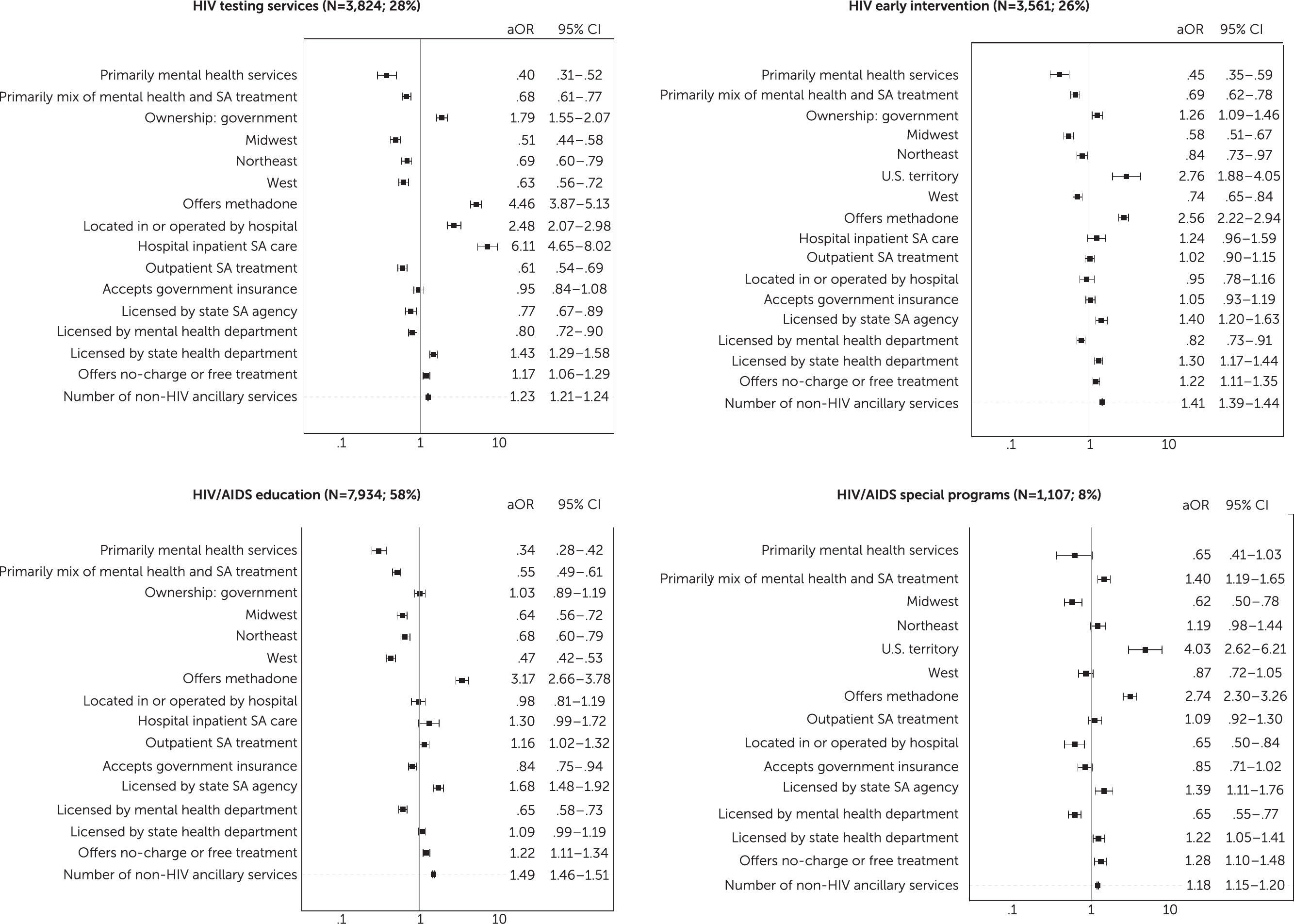
Final multivariable models are displayed in
Figure 1. Across all services, facilities that offered methadone treatment, no-charge services, or a greater number of non-HIV ancillary services and those that focused primarily on substance abuse treatment rather than on mental health treatment (either alone or in conjunction with substance abuse treatment) were more likely than facilities with a primary focus on substance abuse treatment to offer any type of HIV service. Specifically, facilities offering methadone treatment were at least 2.5 times as likely to offer HIV services (all p values <.001). Substance abuse treatment facilities providing no-charge or free treatment had at least 17% higher odds of providing any HIV services (p<.01) compared with facilities that charge for treatment. Facilities were more likely to offer any type of HIV service if they provided a greater number of non-HIV ancillary services (p<.001). Facilities with inpatient substance abuse care had over six times the odds of providing HIV testing services; however, the results were not significant when we assessed availability of any other HIV service. Facilities offering early-intervention and special programs for HIV were more likely to be located in U.S. territories and less likely to be located in the Midwest or Northeast than in the South.
Discussion
Given the high rates of substance use among persons living with HIV, the prevalence of facilities offering HIV services was surprisingly low in most domains—only 8% for special programs and only slightly more than half (58%) for HIV education (counseling or support). Integrating HIV prevention, testing, and support services into programs that address substance abuse is urgently needed given the high rate of comorbid HIV and substance abuse.
Multivariable logistic regression models showed that correlates differed across type of HIV service offered. Providing methadone treatment emerged as the most robust correlate across all services offered; facilities offering methadone treatment were significantly more likely to offer any type of HIV service. Most notably, facilities that provided inpatient substance abuse treatment were six times more likely than other facilities to offer HIV testing. As such, substance abuse treatment programs may be the first place to identify the presence of HIV. Offering HIV testing at the point of entry to a facility specializing in substance abuse treatment, such as during inpatient hospitalization, could increase awareness of the virus, decrease barriers to HIV treatment seeking, and prevent further spread of the virus (
6). Of note, facilities offering early-intervention and special programs for HIV were more likely to be located in U.S. territories. This is a promising trend given the example of Puerto Rico, a U.S. territory, where a primary source of HIV transmission has been documented to be high rates of injection drug use (
12).
The link between funding source and licensing authority to HIV service provision varied considerably across type of service. For example, facilities that accepted government-financed or low-cost or free treatment were more likely than other facilities to offer HIV early intervention and education but not testing or special programs. This might suggest a breakdown in the continuum of care that could be offered within substance abuse treatment programs. New payment and policy mechanisms, such as financial and staff training incentives, might facilitate better integration of HIV services into facilities offering some substance abuse care. Further, facilities licensed by a mental health department were less likely to provide any of the services offered. Further, facilities licensed by a state health department were less likely to offer HIV testing but more likely to offer early intervention—two types of services that should be offered in tandem. Finally, across all services, facilities that focused on offering any type of mental health care (alone or in conjunction with substance abuse treatment) were less likely than others to provide any type of HIV service. This is disheartening, given that interventions addressing co-occurring drug abuse and mental health issues have been found to be more effective at reducing the occurrence and consequences of HIV (
4,
13,
14).
Several limitations of this study are worth noting. This was a secondary analysis of a preexisting data set with limited information available. HIV services were broadly defined and may overlap with each other. Causal interpretations cannot be made without more information about whether or not services were accessed. Finally, we were not able to assess certain client-level characteristics that could be relevant, such as individual substance abuse diagnoses, mental and general medical comorbid conditions, quantity and frequency of substance use, and demographic factors. Future work should examine these factors and how they might affect organizational correlates of HIV service delivery and adoption into substance abuse treatment facilities.
Conclusions
Unlike previously published work, this study focused on a variety of HIV services and used a very large national data set of both private and publicly operated facilities. Substance abuse treatment facilities identified as needing enhanced resources include those offering mental health care, those operated by or financed by a government entity, and those that are licensed by a state mental health board. Funding barriers and knowledge gaps regarding the adoption and implementation of HIV services in these types of substance abuse treatment facilities should be addressed. Doing so requires consideration of other factors associated with adoption and implementation of such services, such as reducing counselor burden and stigma toward HIV, enhancing staff training and supervision to address comorbid conditions, and environmental factors that may be beyond the control of the facility or organization. Findings from our study highlight the strengths and weaknesses that need to be addressed to improve provision of integrated services that accommodate the links between substance abuse and HIV.