The reforms in civil commitment statutes that occurred in the late 1960s and early 1970s led to profound changes in both substantive and procedural aspects of involuntary hospitalization (
1). One such change, the addition of the requirement that persons affected by mental illness be either a danger to themselves or others or gravely disabled, required that this determination be made before initiation of long-term commitment proceedings and that evidence of the determination be available in a commitment hearing (
2). (The term “gravely disabled” refers to a person who, because of a mental illness, is unable to meet his or her basic needs, including the ability to meet the need for food, shelter, and basic self-care.) Toward that end, most states included an emergency hold period as part of the commitment process, during which a person could be placed in custody while the required determinations were made.
Emergency holds potentially play an important role as a bridge between people in crisis and emergency mental health services that individuals may not have otherwise been willing or able to access. Over the past three decades, this pathway has coexisted with a range of new approaches to the management of people with mental illnesses, including the proliferation of police-based crisis intervention models and other forms of jail diversion (
3). This article examines the current state of emergency hold law and identifies important questions about the emergency hold mechanism in contemporary U.S. mental health systems that today bear little resemblance to the mental health systems in existence when many of these laws were enacted.
The pathway between people in crisis and the portals of local mental health services requires critical examination because of the serious health and social problems worldwide caused by undertreatment of mental illness (
4). In the United States, 40% of people with a severe mental illness are untreated (
5). People with severe mental illness who do not receive treatment are the most likely to end up in an acute mental health crisis in need of emergency hospitalization. Individuals facing a mental health crisis who do not receive treatment may go without care or, in the case of violent or disruptive behavior, be arrested (
6).
An emergency hold (also called a 72-hour hold, a pick-up, an involuntary hold, an emergency commitment, a psychiatric hold, a temporary detention order, or an emergency petition) is a brief involuntary detention of a person presumed to have a mental illness in order to determine whether the individual meets criteria for involuntary civil commitment; an emergency hold does not necessarily entail involuntary treatment (
7). Under an emergency hold, a person may be confined in a health care facility at the behest of one or more categories of requestor. Generally, a requestor must fill out an affidavit or go before a judge to testify that a person has a mental illness and meets the state’s specified criteria for a hold as a result of that mental illness. Neither presentation of the matter to a judge nor prompt judicial review is uniformly required. The duration of an emergency hold is typically a few days, but there is significant variation among states.
Emergency holds are distinct from civil inpatient or outpatient commitment, which entails the involuntary treatment of mental illness over a period of days or weeks. An emergency hold is the shortest form of civil restriction on liberty and is often triggered in anticipation of a commitment proceeding (
8). Emergency holds, and all forms of involuntary commitment, implicate constitutional rights of autonomy, liberty, and due process. Under the “danger standard” articulated in the Supreme Court’s 1975 decision in
O’Connor v. Donaldson, a state cannot involuntarily commit people for treatment simply because they have a mental illness; instead, the state can exercise its police powers to coerce treatment only when individuals present a danger to themselves or others (
9).
O’Connor v. Donaldson established that the state may not confine a nondangerous individual who is “capable of surviving safely in freedom by himself or with the help of willing and responsible family members or friends.” Because of the short-term, emergency nature of emergency hold law, however, the statutory requirements typically differ from those set forth for long-term involuntary commitment (
10).
In theory, emergency holds reduce harm and increase treatment access for people with mental illnesses, but the actual impact of these policies, applied to tens of thousands of individuals each year, has not been evaluated. Indeed, it is not even known reliably how many people are exposed to this intervention every year. Variation in provisions across the states constitutes different “conditions” and a natural experiment for evaluation purposes. This article describes an available online open-source data set designed for multistate evaluations of the current state of law governing emergency holds and raises important research questions.
Results
All states and Washington, D.C., allow a person to be placed and held in a health care facility for treatment, observation, or stabilization without consent. Current laws vary on how and for what reason a person can be held, whether or not judicial review of the emergency hold is required, how long a hold can last, and the rights to which a person is entitled during and after the emergency hold. The most prevalent reason for an emergency hold is being a danger to oneself or others, and the most common maximum length of time permitted for the emergency hold is 72 hours (
Table 1).
There is considerable variation in the categories of individuals who may initiate a hold. Police in all jurisdictions have the authority to detain a person who appears to pose an imminent danger, and 38 states explicitly authorize police and peace or parole officers to initiate the emergency hold process. Police officers are the only legal initiators of emergency holds in two states (Wisconsin and Kansas). In 31 states mental health practitioners (such as psychologists, psychiatrists, and mental health workers) can initiate an emergency hold, in 22 states medical personnel (including physicians and nurses) can initiate an emergency hold, and in 22 states any interested person may initiate the process. Most states allow more than one type of initiator (
Table 2).
Eight triggering criteria appear with varying frequency across jurisdictions. Forty-five states and the District of Columbia allow emergency holds when a person is a danger to him- or herself or to others due to mental illness. The five remaining states allow an emergency hold when a person is a danger to self or others without specifying that the danger is due to mental illness. Nineteen states allow an emergency hold if the person is gravely disabled or unable to meet his or her basic needs. Five states specify that a person who has recently attempted suicide may be held, even in the absence of ongoing suicidal ideation. Georgia is an outlier: the only criterion for an emergency hold is having a mental illness and being in need of treatment (
Table 3).
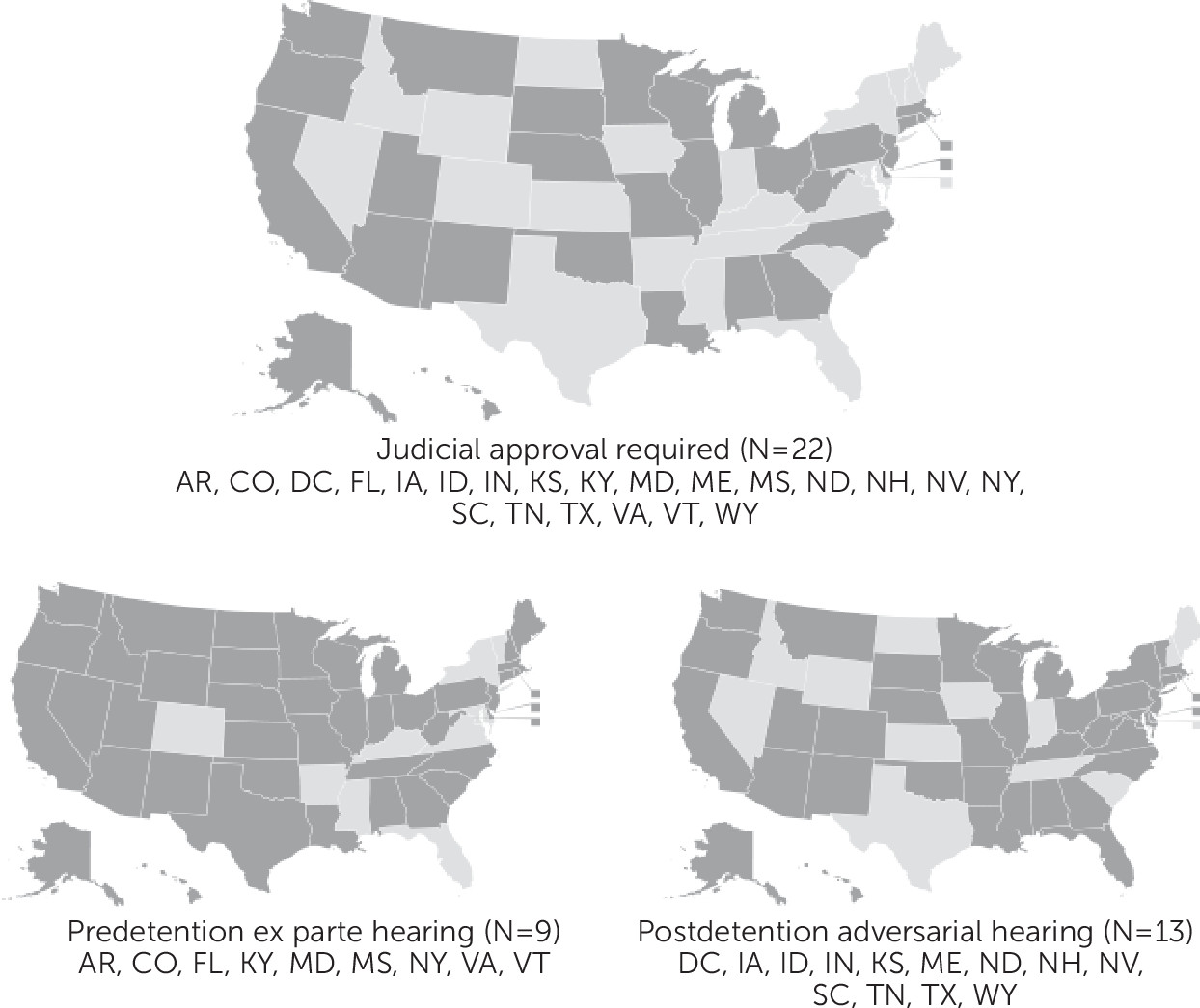
Twenty-two states require judicial approval for an emergency hold (
Figure 1). In nine of these states, judicial approval is required before the admission, and whoever initiates the commitment must show probable cause before a judge or magistrate that the emergency commitment criteria have been met. The hearing may be conducted ex parte (that is, without the person subject to the hold being represented or present). If the judge or magistrate believes that there is probable cause to believe that the person meets one or more criteria for a hold, the judge instructs the police to bring the person into custody and to a hospital where he or she will be examined. If the health care professional believes that the person meets the criteria, the person is placed under an emergency hold. In the other 13 states, judicial review and approval are required after admission. These hearings are conducted ex parte and are based primarily on observations of the patient since his or her hospitalization. If the health care practitioner does not report satisfaction of the hold criteria, then the judge orders the immediate release of the patient.
The length of emergency holds varies by state (
Table 2). The maximum time a person can be held ranges from 23 hours (N=1) to ten days (N=2). Twenty-two states have a 72-hour hold. In eight states, practitioners can extend an emergency hold without a court order.
Kansas, Nebraska, and West Virginia do not specify a maximum length for an emergency hold (
Table 1). Kansas requires a health care professional to evaluate the patient within 17 hours and either release the individual or initiate involuntary commitment proceedings. In Nebraska, a person who is taken into custody must be seen by a health professional within 48 hours. If the health care professional finds commitment to be medically justified, he or she will notify the county attorney, and long-term commitment procedures may begin; otherwise, the person must be released. West Virginia requires a commitment hearing within 24 hours of the person’s being placed on an emergency hold.
Every state but Utah has emergency hold statutes that guarantee specific rights for a person being detained (
Table 4). Twenty-one states require the hospital to allow the patient to make phone calls, 26 states offer the held person the ability to see an attorney, 12 states require that a hospital allow the refusal of treatment, and eight states guarantee the right to appeal the emergency hold. Twenty-nine states require the hospital to provide written notification of the reason for the hold. Ten state laws require discharge transportation for the patient after the hold.
The full LawAtlas data set, the text of the law, and the report, codebook, and research protocol are available for public use at
http://lawatlas.org/query?dataset=short-term-civil-commitment. The LawAtlas Web site includes a “contact us” feature, and people are encouraged to make contact in regard to errors found or updates needed.
Discussion
Every state and the District of Columbia provide for temporary, involuntary hospitalization of people suffering from acute mental illness. The legitimacy and value of these interventions depend on several factors: the statutory criteria and their application, the accuracy of the process for triggering an emergency hold, the degree to which the intervention facilitates (or interferes with) access to care, and the relationship of holds and hold procedures to health and treatment outcomes. There is little research aimed at measuring these factors. This survey of mental health laws creates the foundation for studies to evaluate how emergency hold laws are being used and to assess the impact of the laws on care, community safety, and the treatment system.
The results of the study demonstrate the diversity of criteria that justify holds under state law. Current law generally reflects the standard established in
O’Connor v. Donaldson that people cannot be forced into treatment unless they are at risk of serious harm or of seriously harming another (
12). Many states initially defined dangerousness quite narrowly in state commitment laws. However, over time, concern about lack of treatment has led some policy makers to call for a less stringent standard for involuntary commitment generally, such as “lacking the capacity to consent to treatment,” based on the assumption that the longer people go without treatment after a first episode of psychosis, the worse their illness will become (
12). The data presented here document the expansion of emergency hold criteria outside of the danger standard. Nineteen states allow emergency holds when a person is “gravely disabled” or unable to meet basic needs, which allows the emergency hospitalization of people who do not present an immediate danger to themselves. Most of these additional criteria are consistent with the standard in
O’Connor, but both legal and clinical questions remain unanswered. One study of commitment decisions made in California general hospital emergency rooms suggests that clinicians generally adhere to statutory criteria in their decisions (
13), but there is no research on how criteria are being applied and whether the available criteria are influencing the incidence or appropriateness of emergency holds (and longer-term commitment).
Whether the criteria have an impact on future access to treatment is also unknown. Emergency holds are applied in an environment of chronic deficiencies in treatment capacity. Because there are far more people who meet criteria for a psychiatric hold than there is space to accommodate them in short-term psychiatric facilities (
14–
16), it is certain that the hold process cannot be counted on (or justified) as a reliable gateway to treatment. A lack of short-term inpatient capacity invites the question of whether statutory provisions in many states’ involuntary hold laws can be implemented under these conditions.
Emergency hold laws also may influence community safety. States differ on who can initiate a hold, with police officers, trained mental health professionals, judges, and lay people among the choices. Who may make the decision to hold someone may in turn result in different interpretations of whether a person constitutes a danger to self or others. The effect of these differences on incidence of holds, the hold process, or hold outcomes has not been objectively evaluated. Similar knowledge gaps concern the required procedures and the rights of individuals subject to a hold. Available research suggests that if individuals believe they have been treated fairly and given a voice, their satisfaction and willingness to adhere to treatment may be enhanced (
17–
19), but the comparative effect on public safety is largely unexplored.
The effectiveness of the emergency hold as a tool to stabilize acute symptoms of mental illness also is largely unknown. Ideally, a patient placed on an emergency hold is discharged with a long-term care strategy. Unfortunately, many patients on emergency holds are discharged without a mental health care strategy or lack the resources to follow through on the plan advised and find themselves in a cycle of crisis care (
20). Emergency hold laws do not require the implementation of a long-term treatment strategy, and, remarkably, Alabama, Arkansas, Colorado, and Utah do not mandate that a person on an emergency hold be seen by a health care professional at all. Notably, Pennsylvania does not require an evaluation by a health care professional but mandates that a physician certify the treatment, which must be based on an assessment either before or during the hospitalization.
The difficulty of measuring these statutes in a scientifically valid manner has long presented a barrier to rigorous evaluation of emergency hold policy and, more broadly, of involuntary civil commitment. This research provides an open-source, regularly updated database for capturing the variation in these laws across states. The protocol and coding scheme may be used to create longitudinal data to facilitate quasi-experimental designs with a capacity to support credible causal inferences (
21). The database facilitates future scientific research exploring these myriad, highly important, although presently uninvestigated, documented variations.
Optimal use of involuntary hold laws involves the balance of competing concerns: the welfare of adults with incapacitating mental health conditions, the civil rights of such adults, the public’s concern with safety, the high direct cost of acute inpatient psychiatric services, and the (perhaps even higher) indirect, deferred cost of not providing such services in a timely way to the people who need them. Finding such a balance may implicate public policies and encumber resources at the interface of behavioral health, law enforcement, civil courts, and criminal justice systems. That the features of the relevant state laws vary state by state, in ways that would seem to require correspondingly varying policy solutions and legislative reforms, amounts to a strong argument for more solid state-comparative research on the effectiveness and fairness of emergency commitment practices and their legal underpinnings. The legal database described herein makes such research possible, feasible, and imperative.
This study focused on state statutes dictating the explicit standards regulating emergency hold law. A notable limitation of this study is that it considered only emergency hold laws and did not address the relationship between emergency hold law criteria and statutory criteria for longer-term involuntary commitment. We are developing a database to codify involuntary commitment statutes beyond the emergency hold criteria, which will make this type of analysis possible in the future. Hospital protocols and local law enforcement practices also have a significant effect on whether an emergency hold takes place (
7). Court cases related to emergency hold standards may inform, or even control, how the legal standards are applied. Understanding the impact of state law on local practices is a key area of future research. In order to map out trends, the research team created categories that necessarily lost some finer distinctions in the law; to address this limitation, the database includes a detailed protocol capturing the assumptions the coders implanted during the research phase.