Improving the overall health of people with mental illness is now recognized as a public health priority. Clients of the public mental health system who have been diagnosed as having a major mental illness, such as major depressive disorder, bipolar disorder, and schizophrenia, die younger by between 14 and 32 years compared with the average person (
1). Much of this disparity in mortality is caused by high rates of chronic diseases among patients with mental illness (
2). The high burden of morbidity and premature mortality associated with mental illness translates into substantial societal costs, estimated to be over $300 billion in direct and indirect costs in 2002 (
3).
A critical step to address the high morbidity and associated health care costs among people with mental illness is to better understand health care utilization in this population. Previous studies have documented the association of mental illness and heavy utilization of certain types of health services, including inpatient care (
4–
6) and emergency department (ED) visits (
7–
10). In particular, the high volume of psychiatry-related ED visits is believed to have an adverse impact on hospital resources and to be partially responsible for overcrowding and prolonged waiting times in the hospital ED (
11,
12). Heavy utilization of health care leads to high medical expenditures (
13), which, in turn, may cause significant cost barriers to care among people with mental illness (
14).
This study compared national trends in health care utilization patterns from 2003 to 2014 between adults with and without serious psychological distress. Utilization was measured by outpatient office visits, hospitalization, and ED visits. SPD was measured by the six-item Kessler Psychological Distress Scale (K6) (
18), a nonspecific indicator of mental health problems. The K6 was developed to identify persons in the general population with a high likelihood of having a diagnosable mental illness and associated functional limitations by using as few questions as possible (
18). Nonspecific SPD has been used in previous studies as a proxy indicator of a probable serious mental illness (
2).
Methods
Participants
Individual-level data came from the National Health Interview Survey (NHIS) series of 2003–2014. The NHIS is a nationally representative annual survey of health care access and utilization among U.S. residents in the civilian, noninstitutionalized population and is sponsored by the National Center for Health Statistics. The NHIS collects information for all the individuals in selected households and more detailed information for a randomly selected adult and child from each household. Detailed information on the NHIS survey design, questionnaires, and relevant data are available on its Web portal (
www.cdc.gov/nchs/nhis.htm). Among the sample of 356,736 adults (ages 18 and older) interviewed from 2003–2014, a total of 6,695 participants were excluded because of missing data on SPD. The remaining 350,041 participants were included in the analysis. This study involved secondary data analysis of deidentified, publicly available data and was therefore not considered human subjects research and did not require additional approval from the University of Illinois at Urbana-Champaign Institutional Review Board.
Measures
Serious psychological distress.
SPD was measured by the K6. The K6 asks participants to rate the frequency of six symptoms of psychological distress over the past 30 days on a 5-point Likert scale, with 0 indicating none of the time; 1, a little of the time; 2, some of the time; 3, most of the time; and 4, all of the time. The symptoms include feeling nervous, hopeless, restless or fidgety, so depressed that nothing could cheer you up, that everything is an effort, and worthless. The total K6 score ranges from 0 to 24, with higher scores indicating more severe psychological distress. SPD was defined as a score of 13 or higher on the K6. Selected on the basis of results from receiver operating characteristic analysis, this cutoff point had a sensitivity of .36 and a specificity of .96 in predicting past-year serious mental illness (
19). Detailed information on the psychometric property of the K6 can be found elsewhere (
19).
Outpatient office visits.
Participants were asked how often they had seen a doctor or other health professional about their health at a doctor's office, a clinic, or other location during the past 12 months. They were instructed to exclude overnight hospitalizations, visits to hospital emergency rooms, home visits, dental visits, or telephone calls. In the analysis, the original responses were collapsed into a dichotomous indicator of having had four or more outpatient office visits.
Hospital admissions.
Hospitalization was measured by a dichotomous indicator of any overnight stay in a hospital (excluding overnight stays in the emergency room) during the past 12 months.
ED visits.
Respondents were asked how often they had gone to a hospital emergency department about their own health (including emergency room visits that resulted in a hospital admission) in the past 12 months. The original responses were collapsed into a dichotomous indicator of having had two or more ED visits.
Individual Characteristics
The following individual characteristics were used to adjust multivariate logistic analyses: age (18–26, 27–44, 45–64, and ≥65), sex, race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other or multiple races), education (less than high school, high school graduate, some college, associate degree, and college graduate), marital status (never married, married or cohabiting, and separated, divorced, or widowed), household income as a percentage of the federal poverty level (<100%, 100%−199%, 200%−399%, and ≥400%), health insurance status (any private insurance, public insurance only, and uninsured), and self-report of physician-diagnosed chronic diseases (asthma, cancer, chronic lung disease, diabetes, heart disease, kidney problems, and liver problems).
Data Analysis
Descriptive statistics of sample characteristics were stratified by SPD status. Analyses by subgroup were conducted to test overall trends in health care utilization by using logistic regression and adjusting for sociodemographic characteristics, health insurance coverage, and chronic conditions. Statistical analyses were conducted by using Stata, version 12.1 SE, and accounting for the complex survey design of the NHIS. Because coefficients from different models of logistic regression may not be directly comparable, postestimation procedures using the margins command were conducted to obtain predicted average annual change in utilization by SPD status. In addition to performing an overall trend test assuming changes in utilization were linear, we conducted supplementary analyses when visual inspection of the raw data suggested nonlinear changes.
Results
Table 1 presents sample characteristics stratified by SPD status. In the study sample, 12,568 (3.2%) respondents had SPD. Compared with adults without SPD, adults with SPD were more likely to be female (61.3% versus 51.5%), to be non-Hispanic black (13.2% versus 11.6%), to have less than a high school education (29.6% versus 14.6%), to have an income below the federal poverty level (32.6% versus 12.1%), and to be covered by public health insurance only (40.8% versus 17.1%). Compared with adults without SPD, adults with SPD also reported significantly higher prevalence of all chronic conditions, including asthma (23.8% versus 11.4%), cancer (11.5% versus 7.7%), chronic lung disease (18.7% versus 4.7%), diabetes (16.6% versus 8.0%), heart disease (20.2% versus 9.7%), kidney problems (7.1% versus 1.5%), and liver problems (6.0% versus 1.2%). SPD was associated with more outpatient office visits (63.0% versus 36.6%), hospitalization (22.3% versus 8.8%), and two or more ED visits (27.2% versus 6.6%).
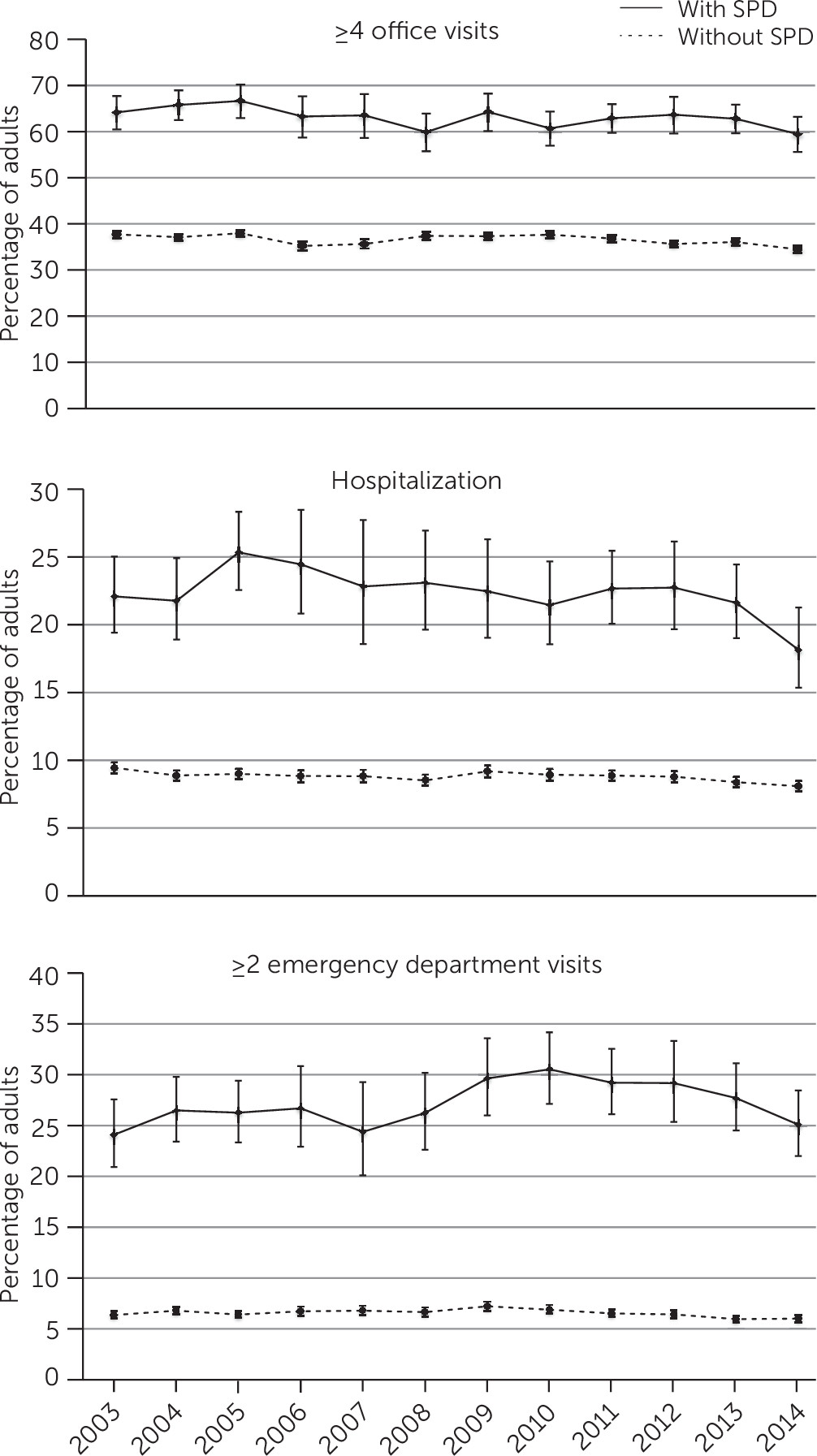
Figure 1 shows the unadjusted prevalence of four or more outpatient office visits, hospitalization, and two or more ED visits among U.S. adults from 2003 to 2014, stratified by SPD status. Adults with SPD consistently reported substantially higher health care utilization through the years compared with their counterparts without SPD. Results from adjusted analyses (results not shown) confirmed these differences. SPD was associated with increased odds of having four or more outpatient office visits (odds ratio [OR]=2.4, 95% confidence interval [CI]=2.3–2.6, p<.001), increased odds of hospitalization (OR=1.8, CI=1.7–2.0, p<.001), and increased odds of having two or more ED visits (OR=2.6, CI=2.5–2.8, p<.001) in the past year. The rates of health care utilization appeared to be relatively stable among adults without SPD, whereas there seemed to be an overall increasing trend in the prevalence of two or more ED visits among adults with SPD.
Table 2 reports results from logistic regressions stratified by SPD status and adjusted for sociodemographic characteristics, health insurance coverage, and chronic conditions. The prevalence of four or more outpatient office visits and hospitalization slightly decreased over time for both groups. Specifically, the percentage of adults with four or more outpatient office visits decreased each year by .4% among adults without SPD and by .5% among adults with SPD. The percentage of adults with a hospital admission decreased each year by .1% among adults without SPD and by .3% among adults with SPD. The CIs for these changes by SPD status overlapped significantly, suggesting that the decreases in outpatient and inpatient health care utilization by the two groups were comparable. The percentage of adults with two or more ED visits decreased by .1% each year among adults without SPD compared with a significant yearly increase of .2% among adults with SPD.
Visual inspection of the raw data suggested that the percentage of adults with SPD who had two more ED visits reached its peak point in 2010 and showed steady decline afterward, suggesting a nonlinear relationship between survey year and ED utilization. To test whether trends in ED utilization among adults with SPD changed after 2010, two separate logistic regression models were estimated, one for the time period from 2003 to 2010 and one for the time period from 2010 to 2014. From 2003 through 2010, the percentage of adults with SPD who had two or more ED visits increased each year by .6% (OR=1.04, CI=1.01–1.07, p<.01). After 2010, the percentage of adults with SPD who had two or more ED visits declined by 1.0% each year (OR=.94, CI=.89–.99, p<.05).
Discussion
Using data from a nationally representative survey, this study tracked trends in health care utilization from 2003 to 2014 among adults with and without SPD. Adults with SPD consistently reported higher health care utilization. Although utilization of outpatient and inpatient care appeared to have decreased for both groups in the past decade, ED utilization increased among adults with SPD. The increasing trend in ED utilization among adults with SPD appeared to have leveled off since 2011.
Consistent with reports from previous studies (
7,
9,
20,
21), adults with SPD reported higher utilization of outpatient, inpatient, and emergency care compared with adults without SPD. In particular, the high volume of people with mental illness seeking treatment in the ED has received heightened attention from hospital stakeholders (
22,
23). Using 2001–2006 data from the National Hospital Ambulatory Medical Care Survey, Slade and colleagues (
12) found that the duration of all ED visits increased at an annual rate of 2.3% and that the average duration of ED visits was 42% longer for mental health–related visits compared with visits for other reasons. Larkin and others (
24) estimated that the number of ED visits for mental illness increased from 17.1 to 23.6 visits per 1,000 U.S. adults from 1992 to 2001. A 2004 survey of emergency physicians reported that six in ten believed that the increase in psychiatric patients seeking treatment at emergency rooms negatively affected access to emergency medical care for all patients, causing longer wait times and limiting the availability of hospital staff (
23). By comparing trends in ED utilization by mental health status, our study added to the literature by documenting that the prevalence of repeat ED visits increased significantly among adults with SPD but declined significantly among adults without SPD.
Several authors have suggested that the increase in ED utilization among individuals with mental illness is a symptom of lack of access to appropriate primary care and mental health treatment (
24,
25). A major reason for overutilization of emergency rooms is lack of access to primary care (
26). In addition to lack of health insurance, it is known that inconvenient office hours, difficulty getting appointments, and shortages of providers who accept certain health insurance plans can all result in lack of access to primary care. Because people with mental illness are more likely to be uninsured or to rely on Medicaid and other public health insurance, they may be at higher risk for lack of primary care, resulting in increased ED utilization. People with mental illness also tend to have high rates of medical comorbidity, which poses additional barriers to access to timely care. In the meantime, the deinstitutionalization movement and state budget cuts have decreased inpatient and residential psychiatric beds and posed severe constraints on the capacity of community mental health care (
24,
25). The impact of state budget cuts may be more severely felt during times of economic recession, when demand for public assistance in accessing general medical and mental health care is especially high. That could explain why there was a hike in ED utilization among adults with SPD from 2007 through 2010 (
Figure 1). Because EDs are generally poorly equipped to address mental health needs, the quality of care received by patients seeking psychiatric care in an emergency room is often suboptimal (
25). In particular, psychiatric boarding, defined as housing psychiatric patients in emergency rooms as they await an inpatient bed or transfer, has become a serious national concern among multiple stakeholders (
25).
The increasing trend in repeat ED visits among adults with SPD appeared to have slowed down since 2011. Recent policy changes, namely implementation of the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 and the ACA, offer some plausible explanations. Implemented in early 2010 in most plans, the MHPAEA requires health insurers to provide the same level of benefits for mental health and substance use services as apply to medical and surgical treatment. There is some evidence that MHPAEA has lowered out-of-pocket spending for mental health treatment and preserved resources for individuals with a diagnosis of more severe mental illness (
27). This decrease in access barriers to mental health care may have prevented some individuals from seeking care in the emergency room since 2011.
In addition, a number of provisions of the ACA that are of particular relevance to adults with mental illness have been implemented since 2010, which could have contributed to the decline in repeat ED utilization among adults with SPD. Specifically, the preexisting condition insurance plan (PCIP) and extension of adult dependent coverage to age 26 were implemented in 2010. Given that first onset of mental illness usually occurs in adolescence and young adulthood (
28), extending dependent coverage for adult children up to age 26 ensures continuity in access to care during these important periods. Early onset of mental illness may have precluded many adults with mental illness from getting health insurance coverage because of insurance policies barring persons with preexisting conditions. The PCIP, which ended in 2014, addressed this issue by creating a temporary program to provide health insurance coverage to individuals with preexisting conditions.
The Medicaid health home state plan option was created in 2011 to provide comprehensive care coordination for Medicaid beneficiaries with chronic conditions, which could have improved access to behavioral health services and supports for adults with serious mental illness, many of whom receive Medicaid. However, the study design did not allow us to make a causal inference regarding the impact of these policy changes. Well-designed studies evaluating the impact of the ACA on use of EDs by persons with mental illness are warranted after the ACA is fully implemented.
A few limitations of the study should be noted. The sampling of NHIS excludes people in institutional care, such as hospitals, jails, and nursing homes, and allows for some flexibility in sampling respondents from the same household. Because people with serious mental illness are more likely to be institutionalized and have even greater needs for health care (
29) compared with the general population, this study is likely to have underestimated the prevalence of SPD and the differences in health care utilization by SPD status. The clinical diagnosis of mental illness that corresponds to SPD is unclear, although the K6 items used to identify SPD appear to primarily assess symptoms of depression and anxiety. Mental illnesses differ in duration, symptoms, and health consequences. Different patterns of health care utilization by diagnosis of mental illness have been reported (
20). Using a global mental health indicator does not allow the examination of differences in health care utilization and barriers to care across mental illness diagnoses.
Moreover, self-report measures of health care utilization are subject to recall errors and bias. The reasons for and nature of care utilization were not assessed. It is unclear whether these visits were associated with psychiatric issues or for general medical conditions only. It is not uncommon for primary care physicians to deliver mental health care (
30). Similarly, considerable emergency room visits are related to psychiatric conditions (
31). In addition, the thresholds used to define health care utilization (four or more office visits and two or more ED visits) are arbitrary. For ED utilization, in particular, our intention was to capture potentially avoidable ED visits by choosing a threshold of two or more visits while also considering the inconsistencies of response categories to questions about ED visits in the NHIS across survey years. However, because of a lack of detailed information for each visit, it was not possible to determine the nature of ED visits.