Approximately 41% of 18- to 24-year-olds in the United States attend a college or university (
1). Serious psychological distress affects an estimated 17% or more of these students (hereafter referred to as college students) (
2,
3). Unfortunately, although college students often have access to campus mental health providers and insurance that covers services, only about one-third of college students with mental health problems receive treatment (
4,
5). For students who do not receive treatment, mental health problems are likely to persist (
6), resulting in lower academic achievement and graduation rates (
7,
8), higher substance misuse rates (
9–
11), greater social impairment (
12), and lower postgraduation workforce participation and income (
13–
16). As a consequence, there is a pressing need to reduce college students’ unmet need for treatment.
Our understanding of factors influencing use of mental health services by college students is evolving. In a 2009 convenience sample of 26 campuses, 22% of randomly selected students had received mental health treatment in the prior year, with lower treatment rates among men, students from racial-ethnic minority groups, younger students, and heterosexual students (
5). However, student characteristics, students’ mental health–related beliefs, the number of campus mental health providers, and campus size explained only a small portion of the two- to threefold variation in service use across campuses (
5). Further exploration of factors associated with students’ use of mental health services could facilitate the development and deployment of programs to increase treatment rates.
As part of California’s Mental Health Services Act (Proposition 63), California counties began working together in 2011 under the California Mental Health Services Authority (CalMHSA) to develop and implement a series of statewide prevention and early intervention initiatives, one of which was aimed at improving student mental health in the University of California (UC), California State University (CSU), and California community college (CCC) systems. As part of an evaluation of these efforts, CalMHSA and the UC, CSU, and CCC systems sought to better understand the prevalence and impact of mental disorders among students, the extent to which students accessed mental health services, the extent to which service use differed between campuses with (UC and CSU) and without (CCC) systemwide networks of campus mental health clinics, and students’ perceptions of their campuses’ environments with respect to mental health.
In this study, we analyzed data from a survey conducted at 39 California colleges and universities that was designed to provide a snapshot of student mental health issues and students’ use of campus and off-campus mental health services. In particular, the study evaluated factors associated with mental health service use, especially factors amenable to change, such as coping skills, campus environment, and the presence of a formal network of campus mental health clinics.
Methods
Undergraduate and graduate students and faculty and staff completed an online survey during spring and fall semesters of 2013. The UC chancellor’s office invited all ten UC campuses to participate; eight chose to participate. The CSU chancellor’s office invited all 23 CSU campuses to participate; nine chose to participate. The CCC president’s office invited all 30 CCC campuses receiving CalMHSA-supported grants and 30 randomly selected CCC campuses not receiving such grants to participate; 14 of the former and eight of the latter agreed to participate. The most common reasons for not participating were competing demands and insufficient staff and resources. Compared with participating campuses, nonparticipating campuses generally were smaller, had fewer students, and had higher percentages of Latino and African-American students. Staff representatives at participating campuses were responsible for contacting students and staff and faculty and were instructed to invite large numbers of students and staff and faculty to participate. Staff representatives at participating campuses used preexisting lists of students and faculty to distribute survey invitations and information. The RAND Institutional Review Board approved the study.
Respondents
A total of 33,943 students and 14,018 staff and faculty completed surveys, including 15,046 students and 9,566 staff from UC, 6,925 students and 2,835 staff from CSU, and 11,972 students and 1,617 staff from CCC.
Measures
Mental health service utilization.
Two questions assessed students’ use of mental health services while at their current campus. Respondents indicated whether they had ever used campus mental health services; students who responded no were asked whether they had used such services off campus. Students who responded yes to either question were categorized as having used mental health services.
Mental health–related academic impairment.
Items modified from the National College Health Assessment (NCHA) II 2010 spring survey assessed the extent to which six emotional issues or behavioral health problems (anxiety, stress, depression, eating disorders, alcohol use, or death of a friend or family member) affected students’ academic functioning within the prior 12 months (
17). Students were categorized as having had mental health–related academic impairment if they reported having dropped a course, received an incomplete, taken a leave of absence from school, or had a similar substantial academic disruption as a result of at least one of the problems.
Current serious psychological distress.
The Kessler Psychological Distress Scale (K6), a commonly used, reliable, and valid six-item Likert measure (
18,
19), assessed how frequently students experienced symptoms such as hopelessness and worthlessness during the prior 30 days. Current serious psychological distress was defined by a score of 13 or greater.
Coping.
A six-item Likert measure, modified from the California Healthy Kids Survey (
20), assessed the extent to which students used active coping strategies to deal with personal problems or stressors. Items included “I know where to go for help with a personal problem” and “I seek alternative solutions to a problem.” The scale had relatively high reliability (Cronbach’s α=.81), and students with a score greater than 2.5 (the average of the scale scores, which ranged from 1 to 4) were categorized as having active coping skills.
Campus mental health climate.
Campus mental health climate was assessed by students’ perceptions of whether or not their campus was supportive of mental health issues (α=.91) and staff and faculty perceptions of the adequacy of support services for students with mental health problems and of the campus resources available to staff and faculty for supporting students with mental health problems. The campus climate measures are described in more detail in
Table 1 (
21).
Demographic characteristics.
Students self-reported race-ethnicity, gender, age, undergraduate versus graduate status, course load (full-time versus part-time), and sexual orientation as lesbian, gay, bisexual, transgender, and questioning (LGBTQ). They also indicated whether they were the first in their family to attend college. Copies of the survey are available by request.
Campus characteristics.
Campuses were categorized by size (large [>20,000 students] or small [≤20,000 students]) and by system (UC or CSU, each with a systemwide network of campus mental health clinics, or CCC, in which each campus chooses whether mental health services are provided and what type to provide).
Location of the campus in a metropolitan community and median income information from the Area Health Resources Files were used to control for community characteristics likely associated with the availability of off-campus mental health resources.
Data Analysis
We sought to adjust for potential differences between student survey responders and each campus’s student body by using available administrative data on students’ gender, race-ethnicity, and course load (full-time versus part-time). We constructed response propensity weights by using a logistic regression of participation, equal to dividing one by the estimated probability of survey responses for each campus, assuming all students could participate. Using the weighted data, we conducted univariate and bivariate analyses to describe students’ mental health service use.
We performed logistic regressions examining the association between students’ use of mental health services and student characteristics, campus environment, and system. We controlled for community characteristics in which the campus was located and considered the hierarchical nature of our data (students within campuses and campuses within systems) by using an iteratively reweighted least-squares approach to produce more accurate estimates and standard errors (
22,
23). We performed separate logistic regressions for combined use of campus and off-campus mental health services and use of campus mental health services. Given the frequency and importance of the interactions of current serious psychological distress, academic impairment, and active coping skills, we present a model of their interactions. Preliminary analyses indicated that the results for the other variables were not substantively different than the results of the regression models without the interactions; as such, presenting the interactions allows us to examine how the combined presence of two or three of these overlapping factors influenced students’ service utilization.
Results
Students were primarily full-time (84%) undergraduates (82%). Sixty-four percent were female, 52% were age 21 or younger, 23% were ages 22 to 25, and 25% were age 26 or older. Current serious psychological distress was reported by 19% of students; 11% of students reported significant mental health–related academic impairment in the prior 12 months. Twenty percent of students reported use of campus or off-campus mental health services (hereafter referred to as “combined mental health services”) while in college, with 10% reporting use of campus services and 10% reporting use of off-campus services.
Table 2 provides additional information about student and campus characteristics and rates of use of mental health services.
Student Characteristics
In the multivariate logistic regression analyses, we found that women, graduate students, and LGBTQ students were significantly more likely than men, undergraduates, and non-LGBTQ students, respectively, to report both use of combined mental health services and campus mental health services (
Table 3). Older students were more likely than younger students to use mental health services. Asian and Latino students were less likely than white students to report use of combined mental health services and campus services. African-American students were less likely than white students to use campus mental health services. Full-time students were more likely than part-time students to use campus services.
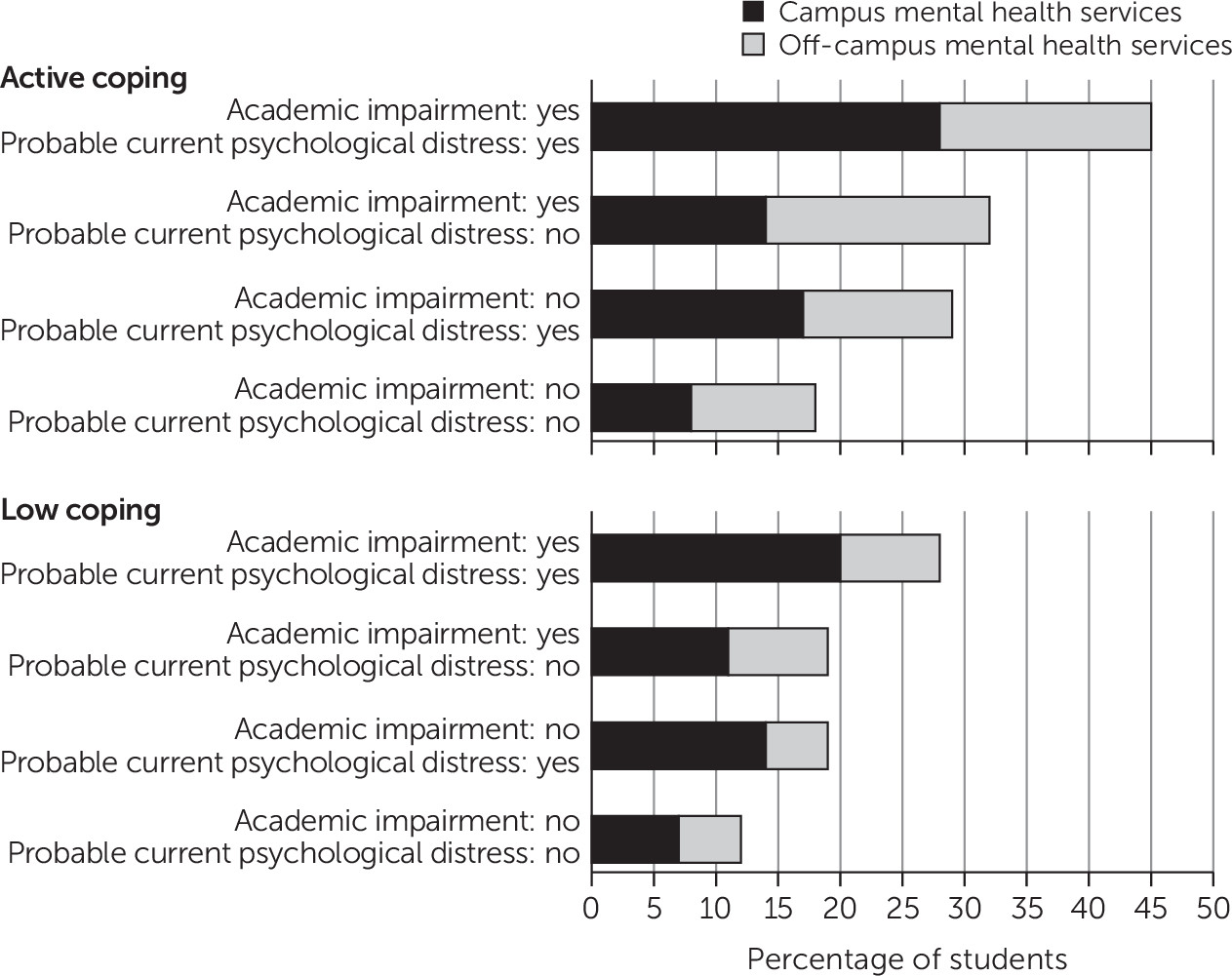
The highest rates of use of combined mental health services (45%) and campus mental health services (28%) were among students with active coping skills who reported both mental health–related academic impairment and current serious psychological distress (
Figure 1). Controlling for other factors, the analyses showed that these students were substantially more likely to use combined mental health services and campus services than students without past-year academic impairment, without active coping skills, or without current serious psychological distress (
Table 3). Active coping was consistently associated with mental health service use. Specifically, even with comparable levels of academic impairment and current psychological distress, students with active coping skills were more likely than students with low coping skills to have used combined mental health services and campus mental health services (
Figure 1 and
Table 3).
Campus Characteristics
Students who perceived their campus climate as supportive of mental health issues were more likely to report using combined mental health services and were substantially more likely to report use of campus mental health services (
Table 3). Similarly, students on campuses rated by faculty and staff as having adequate mental health support services were significantly more likely to report use of combined services and campus services. Students on campuses where faculty and staff reported having adequate resources to support students with mental health problems were also significantly more likely to use combined mental health services and were significantly more likely to use campus services.
Finally, whether a student was enrolled in the UC or CSU system, each of which has a systemwide network of campus mental health clinics, or the CCC system, which does not, was significantly associated with use of mental health services. Both UC and CSU students were significantly more likely to report use of combined mental health services and were substantially more likely to report use of campus mental health services compared with CCC students.
Discussion
This study was one of the largest assessments to date of factors influencing mental health service utilization among college students. Rates of self-reported current serious psychological distress (19%) were consistent with those reported by other studies in postsecondary educational settings (
24). More than 10% of college students in our survey indicated that mental health problems substantially affected their academic success. We are aware of no other multicampus study that has examined academic impairment associated with mental health problems.
One of this study’s major contributions is documenting the substantial influence of campus climate on students’ use of mental health services, both on and off campus. For example, if the culture of every California public college campus was supportive of mental wellness, use of services among students with current mental health symptoms or recent mental health–related academic impairment would be expected to rise by an average of 39%. Our findings underscore the importance of improving campus mental health climates and reducing the stigma related to seeking help for mental health problems (
25). To avoid the unintended consequence of decreasing a student’s willingness to seek mental health services, campuses should support individualized approaches for students with mental health problems, for example, by revisiting policies requiring some students receiving campus mental health services to take a leave of absence (
26,
27).
CalMHSA’s innovative and ambitious student mental health initiatives contained a range of prevention and early intervention activities designed to improve campus climates with respect to mental health. These activities consisted of disseminating information and training students, staff, and faculty through empirically supported approaches to recognizing and supporting individuals with mental health problems (
28,
29); conducting campus training sessions and social media campaigns to reduce stigma around mental health issues and to motivate students to help others (
30); conducting programming to enhance students’ skills in coping with stress and more quickly seeking support when needed; and developing policies, programs, and collaborative partnerships that facilitate access to effective resources and treatment for students. These activities complement more traditional approaches, such as screening for mental health problems (
31) and increasing the number and availability of mental health providers on campus (
32), by seeking to reach and support students with mental health problems sooner. Further evaluation is needed to understand the impact of these efforts.
We found substantial use of off-campus services, particularly among CCC students—possibly because community college students predominantly reside off campus and have easier access to off-campus services or because of the absence of a formal system of mental health services on CCC campuses. However, CCC students remained significantly less likely to receive mental health services compared with their UC and CSU peers. Our findings suggest that a formal system of campus services with sufficient providers to meet demand (
32) could potentially reduce unmet need for treatment. But even on campuses with mental health clinics, there was substantial off-campus service use, highlighting the importance of enhancing collaboration between higher education institutions and community mental health resources (
33).
Helping students deal with stress is another important objective—we found that students with active coping skills were consistently more likely to use mental health services compared with comparable students who did not possess such skills. Enhancing coping skills may be particularly beneficial for students on campuses without mental health services, given that obtaining services off campus may require additional initiative and effort. Because students with less active coping skills appear to be at greater risk of mental health problems (
34), programs to enhance coping skills, whether in person or online, may prevent the occurrence or exacerbation of mental health problems.
Prior studies have found that rates of mental health service utilization are higher among female (
2,
4,
35) and nonheterosexual (
4,
5,
36) young adults and lower among members of racial-ethnic minority groups (
2,
4,
5,
37). Our findings of similar disparities reinforce the importance of ensuring equitable access and encouraging utilization by all individuals. Reaching out to students from underserved racial-ethnic minority groups in culturally appropriate ways (
38), distributing best-practice toolkits (
38), and implementing culturally informed social-marketing campaigns (
39) are a few of the approaches available to administrators and others to address disparities in service use.
Our study had limitations. Not all campuses invited to participate did so. Our approach to surveying a convenience sample was similar to that of other large higher-education surveys (
40–
43), but given that each campus was responsible for inviting students and faculty and staff to participate, we have no information about the numbers or characteristics of nonrespondents. We sought to mitigate effects of selection bias by weighting our sample to represent each campus’s general student body, allowing us to adjust for selection bias associated with available demographic characteristics. The rates of mental health problems in the weighted sample were also comparable to rates in random sample studies of college students, providing some reassurance that respondents were unlikely to have higher rates of mental health problems than the general student body. Still, we had no way to assess response bias—it is possible that respondents were more likely than nonrespondents to seek services and to perceive their campus climate as supportive of mental health issues. Also, we do not know to what extent our findings represent nonparticipating campuses or other higher education institutions. Nor do we know how early CalMHSA activities on campuses might have influenced survey responses, although the majority of these activities occurred after the study period.
Our estimate of mental health–related academic impairment was likely conservative because we operationalized impairment on the basis of just six behavioral health issues (
17); thus we did not capture academic impairment related to other behavioral health issues, such as drug use or posttraumatic stress disorder. Our cross-sectional study design also prevented us from assessing causality. For example, coping strategies and perceptions of campus climate could influence service utilization, but the inverse could be true as well. Our assessment of recent mental health problems (past 30 days) covered a different time frame than our assessment of mental health service utilization (while at college), so we do not know the extent of students’ symptoms while they were receiving services. We underestimated off-campus service use, to the extent that individuals who used campus mental health services may have also used off-campus services. We also had no information on student’s socioeconomic status, which has been associated with asking for assistance among youths (
44) and may be an important unobserved predictor of coping.
Conclusions
Despite its limitations, our study broke new ground by incorporating academic impairment, coping skills, and student and faculty and staff perspectives on campus climates. This study revealed that at least half of students with mental health issues, especially those with active coping skills, sought services off campus—a finding that underscores for colleges and universities the importance of developing solid collaborative relationships with community-based organizations, such as county departments of mental health, that can help support students in times of need. Our findings also reinforce how important it is that postsecondary educators, practitioners, and staff ensure that students understand where and how to access services, that they believe that the campus environment where they work is supportive—not stigmatizing—of students with mental health issues and needs, and that they personally have resources at hand to respond to students in distress.
Acknowledgments
The California Mental Health Services Authority (CalMHSA) provided support for this study. The authors thank Elizabeth May, Ph.D., Erin-Elizabeth Johnson, M.A., Gina Boyd, M.L.I.S., and Hilary Peterson, B.A., of the RAND Corporation for research assistance and assistance with manuscript preparation; Ann Collentine, M.P.P.A., of CalMHSA; Taisha L. Caldwell, Ph.D., of the University of California; Ray Murillo and Ana Aguayo-Bryant of the California State University Office of the Chancellor; Betsy Sheldon of the California Community Colleges Chancellor’s Office; and Robert F. Saltz, Ph.D., and Richard P. McGaffigan of the Pacific Institute for Research and Evaluation. Without their tireless support and valuable input, this work would never have been done.