The prevalence of chronic general medical conditions among people with serious mental illness is high (
1–
3), and these conditions are important contributors to premature mortality in this population (
4). However, fragmented care—a legacy of the historical separation between the specialty mental health and general health systems—poses a barrier to care, which may lead to poorer overall health outcomes (
5). For people with mild to moderate mental illnesses, integrating mental health care into primary care clinics has proven to be an effective strategy, resulting in greater likelihood of timely detection and high-quality treatment of mental health conditions (
6).
However, people with serious mental illness tend to access treatment services through the specialty mental health sector and typically receive poor-quality primary care in the general medical sector (
7). For these reasons, experts have proposed integrating care by providing general medical care services in specialty mental health clinics (
8). Although this strategy has been tested in community mental health centers through a Substance Abuse and Mental Health Services Administration (SAMHSA) grant program (
9) and in the Department of Veterans Affairs (
10), little is known regarding its implementation on a large scale across specialty mental health clinics in a public mental health care system.
This article presents the results of an analysis of a state policy designed to promote integration of general medical care services into specialty mental health clinics throughout the New York State mental health system. Beginning in 2010, the New York State Office of Mental Health (OMH) gave licensed specialty mental health clinics the opportunity to expand their scope of practice to include two types of general medical services, health monitoring (HM) and health physicals (HP). HM services are defined in OMH guidance to clinics as continued measuring of specific health indicators associated with increased risk of general medical illness and early death. The indicators that are measured and billed as HM can include (but are not limited to) blood pressure, body mass index, substance use, physical activity level, and smoking cessation. HP services are defined as general medical evaluations, which include age- and gender-appropriate history, physical examination, and ordering of laboratory and diagnostic procedures. Either service can be provided by a physician, nurse practitioner, or other clinician acting within his or her scope of practice. After enrolling in the program, clinics can be reimbursed by Medicaid, and no prior approval is required for reimbursement.
Clinic enrollment in the program is a critical first step toward delivering integrated care on a sustainable basis. This analysis examined clinic enrollment in the HM/HP program, focusing on two research questions: What is the overall uptake and reach of the program across the New York State mental health system? What characteristics are associated with clinics that enroll in the HM/HP program? Answers to these questions provide insight into the potential for this initiative to improve health for patients with severe mental illness and chronic general medical conditions in a large and complex care delivery system.
Methods
Data
Data on licensed mental health clinics in New York State were drawn from administrative databases maintained by the OMH, including the OMH Provider Database, and from the Medicaid data warehouse. Data on the treated populations were drawn from the 2013 Patient Characteristics Survey (PCS), a comprehensive census of patients treated in mental health programs in New York State over a one-week period (
11). Data from the PCS were available for 492 of the 500 (98%) licensed mental health clinics in the state. Institutional review board approval of study procedures was obtained from the RAND Human Subjects Protection Committee.
Enrollment in HM/HP
Clinic enrollment status was determined as of March 2015 from the OMH Provider Database. Although clinics were able to enroll separately for HM or HP, in practice clinics enrolled for HM only, for both HM and HP, or for neither. Of the 114 clinics that enrolled for HP, only three did not enroll for HM. For this reason clinics were classified as either no HM/HP (N=209), HM only (N=177), or HP with or without HM (N=114).
Clinic Characteristics
Clinic type.
The analysis distinguished three types of mental health clinics. State-operated clinics are owned and operated by New York State and were required to enroll in the HM/HP program. Freestanding clinics are independent entities, unaffiliated with a hospital or larger health care system, although they may be part of a state human services agency. Hospital-affiliated clinics have a formal association with a hospital. They are frequently owned and managed by a parent organization that offers a diverse range of general and behavioral health care services.
Region.
Clinics were classified by address as being in New York City, another urban area, or a nonurban area. Urban and nonurban areas were defined by using Rural-Urban Commuting Area (RUCA) codes (RUCA ≤4 versus RUCA >4) (
12).
Clinic size.
Clinics were classified into quartiles on the basis of the size of their patient caseload. Results are reported for comparisons of the first (<100 patients per week) and fourth (>265 patients per week) quartiles. The caseloads for the middle two quartiles ranged between 100 and 265 patients per week.
Proportion of Medicaid patients.
Clinics were classified into quartiles on the basis of the proportion of their caseload enrolled in Medicaid. Results are reported for the first (<64.3%) and fourth (>86.5%) quartiles, compared with the middle two quartiles (between 64.3% and 86.5%)
Age group served.
The patient population was identified via the OMH Provider Database licensing data to indicate whether the clinic was licensed to serve children, adults, or both.
Percent nonwhite.
Clinics were classified into quartiles on the basis of the proportion of their caseload with nonwhite race-ethnicity. Results are reported for the first (<19.4%) and fourth (>73.8%) quartiles, compared with the middle two quartiles (between 19.4% and 73.8%).
Prior billing for general medical care.
Clinics were classified according to whether any programs associated with their provider agency submitted Medicaid claims for either health monitoring or health physicals in the six months prior to the clinic’s enrollment in the HM/HP program.
Clinic auspice.
Clinics were classified as public if they were owned and operated by the state or a county government; otherwise they were classified as private.
Analysis
The proportion of clinics enrolling in the HM/HP program was calculated for all clinics and for each type. The coverage of the target population was calculated by using data on clinic caseload. We examined predictors of enrollment by using chi-square tests and logistic regression models, with statistical adjustment for multiple clinic characteristics. Standard errors of logistic regression coefficients were adjusted for the clustering of multiple clinics within the same agency. Logistic regression results were calculated with Stata, version 9.4, and reported as odds ratios with 95% confidence intervals.
Results
Clinic Characteristics
As of March 31, 2015, a total of 500 operating mental health clinics were licensed by the New York State OMH, (
Table 1). Three hundred (60%) were freestanding, 135 (27%) were hospital affiliated, and 65 (13%) were state operated. A total of 243 clinics (49%) were located in New York City, including 80 hospital-affiliated clinics (59% of the 500 clinics). Of 65 state-operated clinics, 45 (69%) were located outside New York City.
Hospital-affiliated clinics had higher caseloads than state-operated clinics. Medicaid patients (including those dually enrolled in Medicaid and Medicare) accounted for a majority of patients in all three types of clinic. State-operated clinics served the highest proportion of Medicaid patients: 57 of these clinics (out of 65) treated a share of Medicaid patients equal to or exceeding 64% of all patients. Most freestanding clinics (86%) were private, and 81% of the hospital-affiliated clinics were private. All state-operated clinics are by definition government owned. Finally, 93% of the hospital-affiliated clinics had submitted claims for a health monitoring or health physical visit in the six months prior to enrollment in the HM/HP program, indicating preexisting capacity for providing care for general medical conditions. For freestanding and state-operated clinics, the numbers were substantially lower: 10% and 3%, respectively.
HM/HP Enrollment by Clinic Type
As
Table 2 shows, 58% of all clinics were enrolled in the HM/HP program. As expected, the state-operated clinics had the highest percentage of enrollment—59 of 65 (91%)—with roughly equal participation in HM and HP. Fifty-four percent of freestanding clinics and 53% of hospital-affiliated clinics were enrolled.
Reach of HM/HP Among Medicaid Enrollees
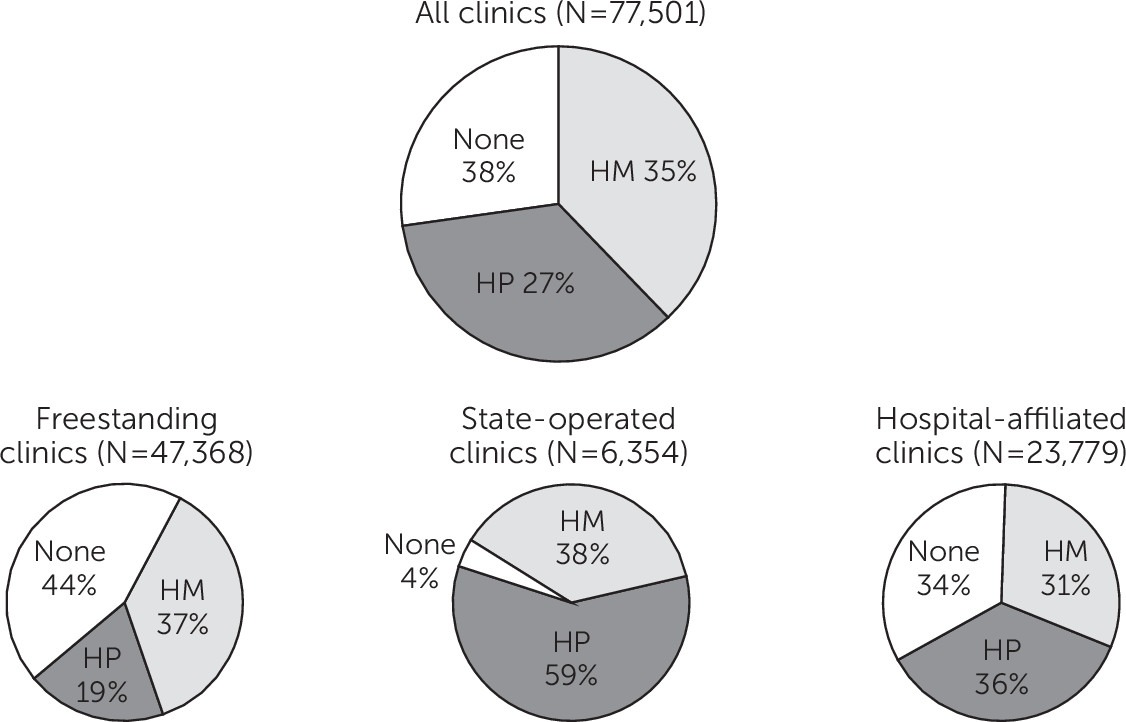
The extent to which the Medicaid population treated in mental health clinics can be reached by the HM/HP program is shown in
Figure 1. Of the total population of 77,501 Medicaid enrollees served by OMH-licensed clinics in a given week, 35% were seen in clinics enrolled for HM and 27% were seen in clinics enrolled for HP. State-operated clinics had the highest levels of coverage, where all but 4% of individuals received services from a clinic in the HM (38%) or HP (59%) program. Most patients in both freestanding (56%) and hospital-affiliated (67%) clinics were served in clinics enrolled in the health services program.
Predictors of Clinic Enrollment
Relationships between clinic characteristics and pattern of enrollment in the HM/HP program (no enrollment, enrollment in HM only, or enrollment in HP with or without HM) are shown in
Table 3. The characteristics that predicted enrollment are different for each type of clinic. Among the freestanding clinics, six characteristics predicted a higher likelihood of enrollment: a nonurban area (χ
2=11.2, df=4, p=.024), a larger patient caseload (χ
2=12.8, df=4, p=.012), an adult treatment population (χ
2=14.9, df=4, p=.005), a higher proportion of white patients (χ
2=13.8, df=4, p=.03), public status (χ
2=13.8, df=2, p=.001), and prior experience billing for primary care services (χ
2=14.8, df=2, p=.001). However, among hospital-affiliated clinics, only clinic size was associated with enrollment, with larger clinics more likely to enroll than smaller clinics (χ
2=12.8, df=4, p=.012). The six (9%) state-operated clinics that did not enroll were smaller and had a lower proportion of Medicaid patients, but these differences were not statistically significant.
Table 4 shows adjusted associations between clinic characteristics and enrollment in HM or HP with or without HM, relative to not enrolling in either program, for hospital-affiliated and freestanding clinics. State-operated clinics were excluded because of the lack of variation in enrollment associated with mandated participation. Two consistent predictors of enrollment in the health services programs were noted: clinic caseload size, with larger caseloads predicting enrollment, compared with medium-sized caseloads; and the agency’s prior experience with billing for primary care services. The clinics with the smallest caseloads did not differ from those with medium-sized caseloads. Compared with clinics that did not enroll in either program, clinics that enrolled only for HM were significantly less likely to be pediatric clinics than mixed adult-pediatric clinics and significantly more likely to be public (county operated) than private. Compared with clinics that did not enroll in either program, those that enrolled for HP were less likely to have caseloads with low proportions of Medicaid patients and less likely to be hospital affiliated than freestanding after the analysis adjusted for prior billing of primary care services by the provider agency and other clinic characteristics.
Discussion
Adults with serious mental illness often go without care for their chronic general medical conditions despite the fact that medical conditions account for the majority of excess mortality in this population (
1,
2). Providing general medical care in specialty behavioral health care settings can improve integration and quality of care, as experience in the Department of Veterans Affairs (
10), a highly integrated health system, and in SAMHSA's Primary and Behavioral Health Care Integration Program, where general medical services are supported through grant funding, has demonstrated (
9,
13). More recently, an optional health home program under the Affordable Care Act that seeks to “integrate physical and behavioral health and long-term services and supports for high-need, high-cost Medicaid populations” has led several states to develop specialty care–based integrated programs for enrollees with serious mental illness (
14). However, the potential for this model to be implemented in a sustainable way across a state’s entire mental health system remains to be demonstrated.
New York State’s HM/HP program offers an opportunity to observe how a large mental health system, with 500 clinics that serve more than 75,000 patients in a typical week, responds to a relatively simple policy innovation: allowing mental health clinics to bill Medicaid for basic general medical care procedures. Understanding how this policy affects the mental health system can inform future efforts to improve health care and health outcomes among adults with serious mental illness. Enrollment by clinics in the HM/HP program is the first step toward successful expansion of access by using this modality of integrated care.
In total, 58% of the clinics, which together served 62% of all Medicaid-enrolled patients with serious mental illness statewide, enrolled in one or both of the HM/HP program options. Rates of enrollment varied across the three main types of clinics in the system. Enrollment by state-operated clinics was nearly universal. However, these clinics are exceptional because the state can require them to participate; in the past, the state has required them to measure indicators of general medical health (
15). The freestanding and hospital-affiliated clinics enrolled at very similar rates—54% and 53%, respectively—although among the clinics that enrolled, the hospital-affiliated clinics were more likely than the freestanding clinics to enroll for the HP license, which provides a higher level of general medical services.
When the analysis adjusted for other clinic characteristics, hospital-affiliated clinics were less likely than freestanding clinics to enroll in one of the integrated care programs. This finding was a surprise, given that hospital-affiliated clinics appear to have built-in advantages for providing general medical care: easier access than freestanding clinics to clinicians qualified to provide general medical services, as well as an incentive to identify patients with general medical needs because those patients can be referred internally for follow-up care. The hospital-affiliated clinics may not have perceived as strong a need as the freestanding clinics to develop a new specialty care–based service for their patients.
Prior billing for HM/HP services by the agency of which the clinic was a part was a strong predictor of enrollment, particularly of enrollment for HP. A large majority of hospital-affiliated clinics had prior billing for these services, reflecting the fact that many hospitals also provide primary care services. In contrast, a minority of freestanding clinics had prior billing, reflecting a much lower level of experience with primary care services in the agencies to which they belonged. This finding suggests that clinics that provided better access to general medical services before the program were best able to take advantage of it. This may also suggest that the policy is more likely to benefit consumers who already have greater access to general medical care services than those facing difficulties obtaining care.
The effect of the policy on the quality of care for general medical conditions and the health status of consumers is an area for future study. However, the findings highlight an important potential limitation of the approach. Although systemwide effects are possible, they may be limited by the lack of resources in a given community to develop services de novo. Additional policy efforts may be needed to engage clinics that lack experience with primary care services or affiliations with general medical providers.
Other predictors of enrollment provide additional hints about the incentives affecting clinic decisions. First, large clinics were more likely than medium-sized clinics to enroll in the HM and HP programs. A possible explanation is that smaller clinics anticipated a challenge in maintaining a sufficient flow of patients to cover the cost of hiring a clinician through reimbursement. Effect size was larger for HP services, where services are less frequent (for example, provision of annual physical exams) and more costly (a physician or nurse practitioner is required). Second, publicly owned county clinics were more likely to enroll than private clinics. This finding may reflect the ability of public clinics to share the costs of providing services, such as hiring of new staff, with other government agencies or care providers. These findings suggest that additional strategic investments could extend the impact of the policy into other sectors of the mental health system.
Conclusions
Results of this study suggest that the policy implemented by the New York State OMH to promote mental health–based general medical care was successful in covering a large portion of the target population: individuals with serious mental illness who are treated in specialty mental health clinics. However, the results also suggest gaps in the system. Different policy strategies are likely to be needed to extend access to general medical services to the types of clinics in the public mental health system that were least likely to enroll—specifically, smaller, nonpublic clinics with no prior experience delivering general medical care services. In addition, further studies of the impact of the HM/HP policy on utilization, quality of care, costs, patient experiences with care, and health outcomes are needed to arrive at a fuller evaluation. Future studies of this and related policies can build a knowledge base for guiding evidence-based policy in integrated delivery systems for this population with complex medical needs.