Borderline personality disorder (BPD) is among the most frequently encountered yet undertreated conditions in clinical mental health settings (
1–
3). BPD may have a profoundly negative impact on the psychosocial and occupational functioning of persons with the disorder (
2,
4) and may severely burden family members and health systems (
5,
6). Despite the disorder’s substantial public health impact, empirically supported therapies for BPD are not widely available in publicly funded treatment settings. Mental health services in these settings typically focus on short-term intervention or case management (
7), which are not likely to produce recovery among persons with BPD. The experiences of persons seeking care for BPD are often unrecognized, and standard services may not reflect treatment preferences of persons with BPD (
7,
8). However, understanding the experiences of persons seeking care for BPD is important for developing targeted services and connecting consumers with appropriate resources (
1).
Prior studies have examined service needs related to BPD and barriers in obtaining appropriate services; however, few studies have qualitatively examined service needs from the perspective of those seeking care. For instance, Strike and colleagues (
9) explored the circumstances of health service use among suicidal men with BPD and found that prior negative experiences with health care providers frequently contributed to avoidance of health care settings and to “fragmented pathways” to care. Other research has examined perceived lack of supportive services for caregivers and family members of persons with BPD (
6). Dunne and Rogers (
6) interviewed caregivers for persons with BPD, and they found that the caregivers felt both dissatisfaction with their involvement in care planning and uncertainty about what supportive services were available.
Although these findings highlight the difficulties of obtaining appropriate care and services for BPD, the resource landscape for BPD is not understood completely. Few studies, for instance, have either evaluated on a national scale the circumstances or preferences of persons seeking information about BPD services (“BPD care seekers”) or incorporated perspectives from consumers, caregivers, and family members. Such knowledge is important for describing service limitations and for allowing a marginalized population to articulate issues and concerns. Using qualitative analysis of data from a national sample of BPD care seekers, we aimed to build on the knowledge base for BPD services by characterizing the experiences of consumers, caregivers, and family members seeking BPD resources.
Methods
Sample
Data were obtained by study investigators retrospectively from the Borderline Personality Disorder Resource Center (BPDRC) at New York Presbyterian Hospital, an online center created to connect persons affected by BPD with treatment and support (
www.bpdresourcecenter.org). Established in 2008, the BPDRC disseminates educational materials and connects individuals to region-specific resources, such as treatment centers, physicians, and supportive services. The BPDRC Web site provides general BPD information, whereas individuals seeking referrals, specific information, or other resources may contact the BPDRC staff by e-mail or phone. During service requests to the BPDRC, licensed clinical social workers conduct brief unstructured interviews regarding service needs and experiences, and they record the interview content in the form of written narratives, or transcripts. E-mails were also transcribed and analyzed; however, the vast majority of records were phone call requests. Resources and referrals are provided on the basis of individual callers’ needs and preferences.
Participants who contacted the BPDRC with service requests by telephone or e-mail between January 2008 and December 2015 were eligible. We excluded from analysis the transcripts of participants who identified themselves as a minor (age <18), who were non-English speaking, or who were referred to services outside of the United States. This study was approved by the Weill Cornell Medical College Institutional Review Board.
Analysis
Descriptive statistics describing frequency of requested service types, the distribution of requests by state, and the caller’s relationship to a BPD patient were generated. If information was available, requests were categorized by demographic information, such as age, gender, and race; however, demographic information was not systematically collected.
To assess the themes identified within caller records, we conducted a conventional qualitative content analysis (
10) of a randomly selected subset of 500 transcripts, including calls spanning the duration of the request database (2008–2015). Analysis and coding were conducted in stages, guided by principles of grounded theory (
11). First, study investigators reviewed the selected transcripts, performed exploratory analyses, and independently identified major themes. Second, a review of literature concerning health service utilization and treatment for BPD was conducted and was used as a reference to consider the preliminary themes contained in the transcripts. Third, study investigators developed analytic codes for each theme, making iterative adjustments on the basis of the data and service literature, and applied them to the transcripts. Similar concepts and codes were diagrammed, consolidated, and grouped by central themes. Call record excerpts were selected to illustrate overarching concepts. Coding, analyses, and literature review were performed by using NVivo qualitative analysis software (
12).
Results
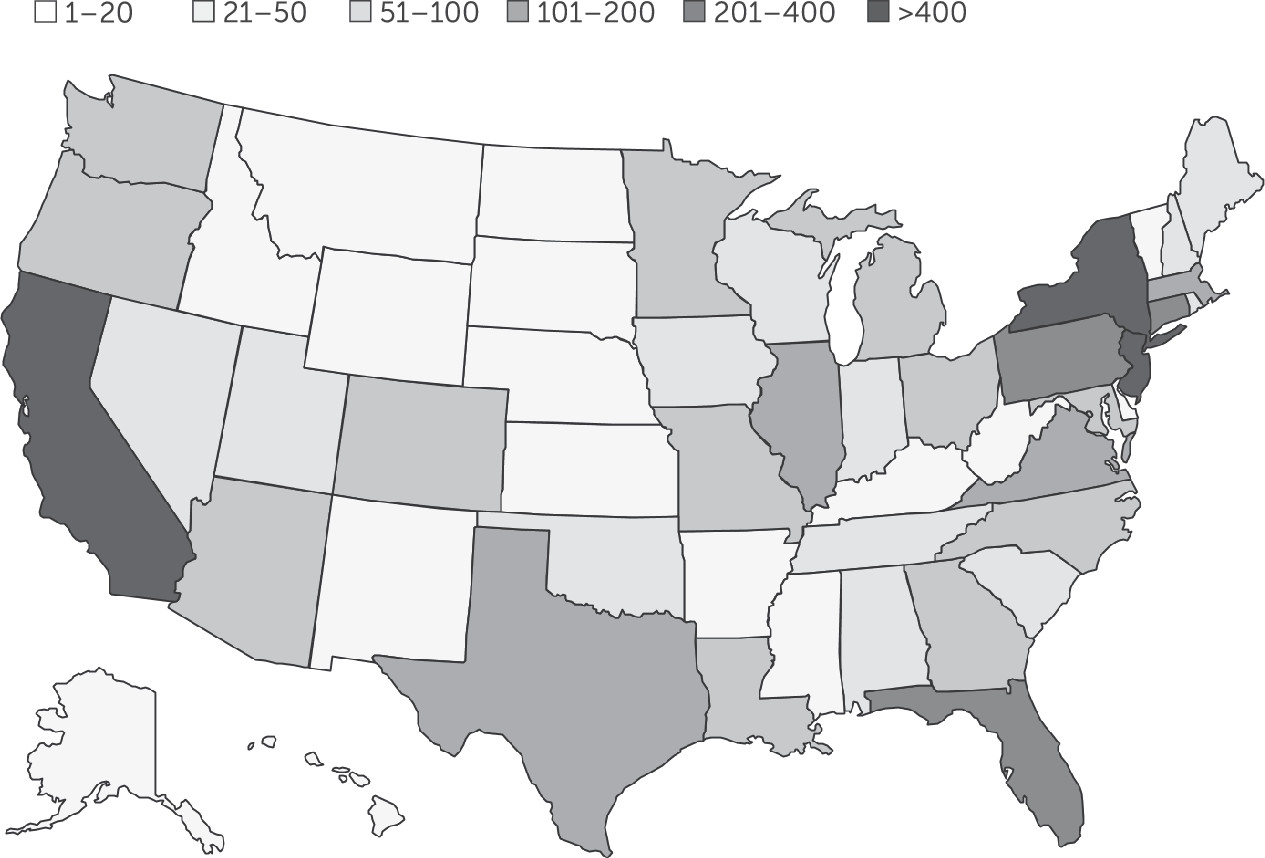
The BPDRC database of service requests contained eligible transcripts for 6,253 callers (approximately 800 per year), distributed across all states (
Figure 1). Most inquiries (N=3,039, 49%) were made by family or friends of persons diagnosed as having BPD, whereas 40% (N=2,514) were made by individuals with BPD. Approximately 9% (N=563) of contacts were by health professionals seeking referrals for individuals with BPD or seeking information regarding BPD symptoms. Approximately 10% (N=603) of calls concerned services for adolescents.
Requested Services
Among the randomly selected call records, 256 were for outpatient or intensive outpatient care, making it the most frequently requested and recommended service (
Table 1). Dialectical behavioral therapy (DBT) resources were requested by a majority of callers seeking outpatient services for BPD (N=172, 67%), followed by requests for general cognitive-behavioral therapy (N=54, 21%) and transference-focused therapy (TFP) (N=4, .02%). Few callers seeking outpatient services for BPD requested pharmacotherapy (N=3, .01%) or referrals for prescribing physicians (N=2, .01%), and only two (.01%) requested referrals to psychiatrists who could prescribe medications for BPD.
Mental Health Literacy and Marginalization
Two notable and related themes were poor mental health literacy with respect to BPD and marginalization and stigmatization of individuals with BPD. Informational materials were the most frequently requested resources besides requests for outpatient referrals. Several callers requested basic epidemiologic statistics regarding BPD prevalence. Similarly, both patients and providers requested resources to learn about the symptoms and features of BPD, to identify BPD, and to distinguish BPD from other mental disorders. For example, one transcript reported that a caller wanted information about accommodating an employee with BPD, stating that “she has an employee with BPD [symptoms] who is very difficult. [She] wanted articles on how to prevent divisiveness when such an individual is on staff.”
Many callers reported apprehension about receiving a BPD diagnosis because of potentially negative attitudes of others. For example, one caller reported that “she fears she has symptoms of BPD and depression but has avoided seeking diagnosis. . . . She is concerned about anyone knowing that she has BPD due to stigma.” To some callers, the issue of stigmatization was reflected in the orientation of mental health providers toward BPD. One transcript described a caller with BPD who was also a mental health provider. “She is doing research on stigma concerning BPD among mental health professionals,” according to the transcript. “She has been diagnosed with BPD . . . and was turned away by many clinicians.” Transcripts from other callers noted the isolation created by stigmatizing attitudes: “She has had BPD her entire life and said that the stigma has kept her isolated and ostracized. Her local hospital has asked her not to return.”
Family and Caregiver Resources
A majority of contacts to the BPDRC were made by family members or friends (N=271) on behalf of individuals with BPD. The primary service needs identified most by friends or family members after outpatient services were supportive services (N=77, 28%) and resources to facilitate conversation with someone who might have BPD (N=61, 23%). In particular, the transcripts reflected a desire for increased communication between mental health providers and family members and for more integration of family members into care plans. For instance, one transcript noted, “A family of [a son with BPD] in his early twenties asked [for] help in learning how to communicate and interact with their son. He is seeing a therapist, but the parents feel they lack skills needed to positively impact/assist their son.”
Family members frequently requested supportive resources to help them cope with or understand BPD. Family Connections, a 12-week course that provides education, skills training, and support for people in a relationship with someone who has BPD (
13), was the most commonly referenced resource for those seeking family-oriented services. Other frequently requested family-based resources included Treatment and Research Advocacy for Borderline Personality Disorder (
14) and the National Education Alliance for Borderline Personality Disorder (
15).
Insurance and Finances
One theme closely tied to requests for family services was concern about insurance coverage and finances. Approximately 12% (N=60) of callers reported concerns about treatment costs or the affordability of their level of desired care. Financial concerns were especially prevalent among callers seeking inpatient services or services for family members. For example, the transcript for one caller stated, “Her 16-year-old son has BPD and she cannot afford $20,000 per month for residential treatment. She wanted to find less costly alternatives that would provide structured, intensive treatment.” A secondary and related theme concerned a divide between desired care and the care covered by public insurance. For example, the transcript of one caller reported that “her 17-year-old daughter is on Medicaid, was diagnosed with BPD at age 14, and has been hospitalized repeatedly for parasuicidal behavior. [She] cannot afford private pay.”
Medical and Psychiatric Comorbidity
Caller records reflected the difficulties of individuals with BPD in coping with comorbid psychiatric and general medical disorders and their desire to find services to accommodate more complex pathologies. Among individuals with BPD, 10% (N=19) of callers reported substance abuse problems or an additional psychiatric diagnosis. A typical example highlights the negative impact of BPD on coping and interference with treatment for comorbid psychiatric disorders: “[Caller] has a 19-year-old son in a drug rehab in Florida who will be [discharged] shortly. He has BPD, bipolar disorder, and substance abuse. They want a longer-term residential center that can handle all of these.” Another example illustrates how general medical conditions may complicate treatment: “[The caller’s] niece has BPD and severe substance abuse plus diabetes and asthma. [She] has overdosed many times and had inpatient rehab plus two detox stays with no effect.”
Crisis Services
A final theme was need for acute mental health services for patients and families in crisis. Requests included services for families undergoing stress because of an individual with BPD, services for individuals demonstrating suicidal behaviors, or resources for individuals experiencing general distress. For example, the transcript for one caller reported that “her daughter, 17, fits criteria for BPD and that she is noncompliant and will not go to treatment. She has fits of rage, [she] cuts herself, and police have been called a few times to take her to the ER.” Likewise, the impact of periods of crisis on families was reflected by a caller who stated that he “has a 41-year-old daughter with BPD whom he has supported for three years. [Insurance] is not helping and family is falling apart due to stress.”
Discussion
The BPDRC database provided a wide-ranging account of resource preferences, barriers to care, and general experiences of BPD care seekers in the United States. Primary themes included types of requested services, mental health literacy and marginalization, family resources, financial concerns, comorbidity, and crisis services. Overall, these findings underscore challenges in obtaining appropriate care for BPD and opportunities for improving the coverage and scope of current resources.
Requested Services
The predominance of psychotherapy in resource requests is consistent with current research and practice guidelines regarding therapy for BPD (
16–
18). Indeed, the form of psychotherapy requested most, DBT, is among the most widely validated therapeutic methods for treatment of BPD (
2,
19) and is effective at achieving remission of some troubling features of the disorder, such as self-injury, suicidality, and hospital use (
2,
20). Other forms of psychotherapy, such as TFP, mentalization-based therapy, and schema-focused therapy, have also been shown to be effective at treating BPD compared with nonpsychotherapeutic treatments (
21,
22).
In contrast, few callers requested resources or referrals for medications, a result that is consistent with current knowledge regarding pharmacotherapy for BPD (
23). Although research suggests that antidepressants and antipsychotic medications may be used successfully to treat certain aspects of BPD, there is limited evidence with which to make conclusions regarding the overall efficacy of pharmacotherapy for BPD (
23). The infrequency of requests for pharmacological resources suggests that the callers had at least general awareness of current practices.
Information and Mental Health Literacy
The predominance of requests for informational materials highlights a lack of knowledge about BPD among both consumers and providers. Mental health literacy, referring to “knowledge and beliefs about mental disorders which aid their recognition, management or prevention” (
24), is an especially important goal, given that BPD is among the most underrecognized mental disorders (
25,
26). Inadequate knowledge regarding BPD may lead to inappropriate treatment seeking, poor implementation of treatment plans, and misallocation of mental health resources (
7,
25,
27). These outcomes often result in diminished patient confidence in service providers and reduced likelihood of seeking treatment (
9).
Lack of knowledge about BPD also creates barriers to appropriate treatment by contributing to marginalization and stigmatization of persons with the disorder (
1,
7,
8). Among health professionals, knowledge about BPD informs attitudes and beliefs about the causes of the disorder, influencing rates of diagnosis and recommended therapies (
1,
25). Yet BPD is still seen by many as an untreatable disorder (
7,
28), leading providers to avoid the diagnosis altogether (
29). Ensuing poor treatment responses reinforce providers’ negative perceptions of BPD, further limiting understanding of the disorder (
7,
28). Given the callers’ reports of negative experiences in terms of being rejected from treatment or being referred to ineffective treatment, efforts to increase mental health literacy are warranted to reduce stigmatization of BPD and reduce inappropriate treatment seeking. Moreover, training of providers in the recognition of personality disorders and the need for long-term supportive services may likewise help reduce unnecessary service utilization.
Family and Caregiver Resources
Although treatment programs and research acknowledge the important role of family caregivers in the treatment and management of BPD, supportive services for caregivers are rarely available (
30). BPDRC callers frequently expressed unfamiliarity both with the disorder and with available family resources. Likewise, consistent with prior studies (
6,
30), family members reported dissatisfaction with their involvement in treatment and communication with providers. Further clinical and systematic efforts are needed to improve understanding of BPD among family members, to build family members’ awareness of available supportive services, and to encourage integration of families into therapy. As an initial step, connecting family caregivers with existing available resources is especially important, given that caregivers for persons with BPD may experience significant self-neglect and strain on their personal health and well-being (
6).
Insurance and Finances
As reported by callers, individuals with BPD frequently accrue high health care costs, in part because of difficulties in locating appropriate services, inaccessibility of treatment, and poor insurance coverage (
1,
5). Management of BPD frequently requires long-term treatment and support, yet many health care insurers are reluctant to reimburse for long-term therapeutic sessions (
31). Insurance coverage is often more favorable toward treatment of conditions such as major depressive disorder and bipolar disorder, which are viewed as more urgently debilitating and treatable within a limited time frame (
1,
31). Given these difficulties, therapists have considerable incentive to bill for short-term treatment (
31).
In addition, compared with research for other mental disorders, BPD research has received far less funding from the National Institutes of Health (
1). The lack of research imperative likely contributes to the lack of services and coverage for BPD treatment. Unreliable findings regarding treatment efficacy and prognosis may, in turn, be used as justification for limited reimbursement for long-term BPD services (
31). As reflected in caller transcripts, one potential consequence of inadequate research and insurance support is less coverage for more intensive treatment, residential care, and services for those most in need.
General Medical and Psychiatric Comorbidity
General medical and psychiatric comorbidities were among the concerns expressed most commonly by the BPDRC callers. Research suggests that BPD is frequently associated with concomitant mood and anxiety disorders, substance abuse, self-injury, suicidal behaviors, and general medical illnesses (
2,
32–
34). Psychiatric comorbidity is an especially important consideration in relation to treatment outcomes. A number of independent, large-scale longitudinal studies have shown that comorbid personality disorders, particularly BPD, not only adversely affect treatment outcomes of major depressive disorder (
35,
36) but also lead to lower rates of remission and increased relapse rates (
37–
39). In addition, the negative effects of BPD on treatment for depression seem to be unidirectional (
38–
41). For instance, Gunderson and others (
38) found that improvements in major depressive disorder were not followed by improvements in BPD, whereas improvements in BPD were often followed by improvements in major depressive disorder. Similar findings were reported with regard to the relationship between BPD and bipolar disorder (
42) and anxiety disorders (
43). These findings underscore the importance of comprehensive approaches to address BPD and comorbid disorders.
Crisis Intervention
The consequences of not caring for individuals in crisis are potentially costly to health care systems and potentially lethal to patients. Given that BPD is characterized by emotional and interpersonal instability, individuals with BPD often experience crises that add to the difficulty of coping with anxiety, depression, and psychotic symptoms (
44,
45). During crisis periods, individuals with BPD are at particularly elevated risk of self-injury and suicide (
46), necessitating acute mental health services (
44,
45); however, few interventions specifically address acute crisis periods. A review by Borschmann and colleagues (
44) found only two ongoing randomized crisis intervention trials for individuals with BPD; the authors concluded that there was insufficient evidence to assess efficacy of crisis intervention for persons with BPD (
44). As revealed by the BPDRC callers, there is significant demand for effective crisis interventions, and it may be inadequately addressed by current resources.
Although this study provided important observations from the perspective of BPD care seekers, it also had limitations. First, despite being nationally based, the BPDRC caller database is a convenience sample lacking systematic collection of demographic information and, therefore, may not be representative of more general views or experiences. Future studies with more rigorous sampling methods and a focus on specific demographic groups may provide a more thorough understanding of current issues and trends in BPD services. Similarly, caller transcripts were based on unstructured interviews, which may not reveal all salient themes. Future research should explore in more detail the themes represented in this study and the factors and services related to successful management of BPD.
Conclusions
This study provided a broad overview of the experiences and preferences of BPD care seekers and highlights important focal areas for improving BPD services. Consistent with prior studies, BPD care seekers identified family services, crisis intervention, and mental health literacy as areas in which available resources could be improved or expanded. Similarly, BPD care seekers identified stigmatization, financial concerns, and comorbid disorders as potential barriers to finding and obtaining appropriate services and treatment. These insights offer targets for future efforts to improve BPD services and outcomes.