Mental and substance use disorders affect 56 million adults in the United States (
1). In recent years, less than half of individuals with mental disorders and one-tenth of those with substance use disorders received any treatment (
1). Inability to access affordable treatment is one reason for treatment underuse (
2). The uninsured rate has long been higher among individuals with mental and substance use disorders than the general public (
3,
4). Many uninsured individuals pay out of pocket or seek treatment from safety-net providers. Among the insured, restrictive insurance coverage and high cost-sharing have been barriers to receiving care (
5).
The Affordable Care Act (ACA) is designed to reduce uninsurance and barriers to care. Beginning in 2014, most adults faced a new requirement to buy insurance. In addition, the ACA allocated new funding to expand Medicaid to adults with incomes below 138% of the federal poverty level. In 2014, 25 states and the District of Columbia adopted ACA Medicaid expansion (31 states and the District of Columbia expanded by 2016) (
6). State marketplaces selling federally subsidized insurance were also implemented in 2014. Treatments for mental and substance use disorders are essential health benefits in marketplace plans (
7). ACA-related Medicaid and private insurance plans are also subject to the federal Mental Health Parity and Addiction Equity Act (MHPAEA), which mandates mental health treatment coverage comparable to medical-surgical treatments (
7).
In 2014, ACA provisions increased the insured rate by more than 5 percentage points in the adult population (
8,
9). Enrollment gains were especially large among low-income adults in Medicaid-expanding states (
8). Individuals with chronic illnesses (
10) and fair or poor health (
11) were also especially likely to gain insurance in 2014. ACA provisions increased overall service use and reduced out-of-pocket spending among the newly covered (
8,
12). Commentators have suggested that 2014 expansions—in tandem with the MHPAEA—could greatly expand access to treatment for people with mental and substance use disorders (
5,
7). The 2010 ACA provision allowing young adults to remain as dependents on parental insurance coverage increased the use of mental health care (
13) and improved financial protection (
14). However, impacts of 2014 ACA provisions on treatments for mental and substance use disorders are largely unknown. We examined changes in coverage and service use in a national sample of individuals with these disorders from 2011 to 2014.
Methods
Data
Cross-sectional data from the National Survey on Drug Use and Health (NSDUH) were analyzed. NSDUH annually interviews about 70,000 individuals and provides nationally representative estimates for the noninstitutionalized population. Respondents are interviewed in their homes with computer-assisted interviewing. Annual response rates varied from 58.3% to 64.7% during our study period (2011–2014) (
1).
The NSDUH identifies individuals likely to currently have mental illness by using a score derived from screening questions on mental health impairment, suicidality, and severe psychological distress. This composite measure has been validated against clinical assessments (c statistic=.745) (
15). Individuals are screened for current substance use disorders by applying
DSM-IV definitions of abuse or dependence.
Individuals were asked about their current insurance status in several major categories: private insurance, Medicaid or the Children’s Health Insurance Program, Medicare, and other insurance programs (including Department of Veterans Affairs benefits and TRICARE). Individuals not reporting any of these categories were asked in a follow-up question confirming whether they were uninsured.
Individuals were separately asked whether they received treatment for a mental or substance use disorder in the prior year. Individuals indicating prior-year mental health treatment were asked about visiting various inpatient or outpatient settings or receiving a prescription for a psychotropic medication and could indicate multiple types of treatment. Individuals indicating substance use disorder treatment were also asked about visiting inpatient and outpatient settings.
Payment source for mental and substance use disorder treatment was measured using various question formats. For mental health treatment, payment source was measured only for prior-year outpatient and inpatient services (not for psychotropic medications), and individuals could indicate only one source of payment that covered the majority of treatment received (individuals with both outpatient and inpatient service use could indicate different sources of payment). For substance use disorder treatment, individuals were asked to indicate all payment sources for treatment most recently received. We analyzed each payment source with a separate indicator.
The NSDUH also collects demographic measures, including sex, race-ethnicity, household income, highest educational attainment, and age. To protect confidentiality, variables such as income are reported in broad categories. To address missing data for some variables, NSDUH analysts apply imputation methods (
16). We used the imputation-revised measures to minimize nonresponse bias.
Statistical Analysis
To compare changes after the implementation of the 2014 provisions of the ACA, we divided the sample into two groups: 2011–2013 and 2014. We identified individuals with either probable mental illness or a substance use disorder, restricting the sample to adults ages 18–64 (persons ≥65 were excluded because most were Medicare eligible before implementation of the ACA).
For individuals with a mental disorder, with a substance use disorder, and with neither disorder, we calculated percentages with each type of insurance. We also calculated percentages of those using any treatment in the prior year and, conditional on receiving treatment, types of settings visited and source of payment for treatment. For substance use disorder treatment, we excluded treatment in self-help programs and jails, which are typically not paid for through insurance.
We examined changes overall and among adults with household income ≤200% of the federal poverty level (FPL). The ≤200% category includes all individuals eligible for Medicaid under the ACA provisions residing in states expanding Medicaid and two-thirds of individuals enrolled in the marketplaces (
17).
All estimates were adjusted for age, sex, race-ethnicity, residence in a metropolitan area, and self-reported general health. We applied survey weights to make estimates nationally representative, adjusting standard errors for complex sampling design. We calculated two-tailed t tests to compare differences in means for the two time periods and used p<.05 as the cutoff for statistical significance.
Sensitivity Analyses
We conducted several sensitivity analyses. First, we considered changes in the subgroup with both mental illness and substance use disorders. Second, to analyze changes among those more or less likely to be affected, we examined changes among individuals with income ≤100% of FPL (who would be most affected by Medicaid expansion) and individuals with income >200% of FPL (who might be less affected). Third, we excluded populations enrolled in Supplemental Security Income (SSI) because they were eligible for Medicaid prior to the ACA. Fourth, we excluded adults under age 26 who had already been substantially affected by the 2010 ACA dependent coverage provision. Fifth, we examined the subgroup of individuals interviewed in the NSDUH in the second half of 2014, because they had greater time to experience new coverage options, comparing them with individuals interviewed in the second halves of 2011, 2012, and 2013. Sixth, instead of modeling a discontinuity in 2014, we modeled time trends over the sample period using linear and quadratic coefficients to provide more insight into the evolving trends.
Results
Prevalence and Population Demographic Characteristics
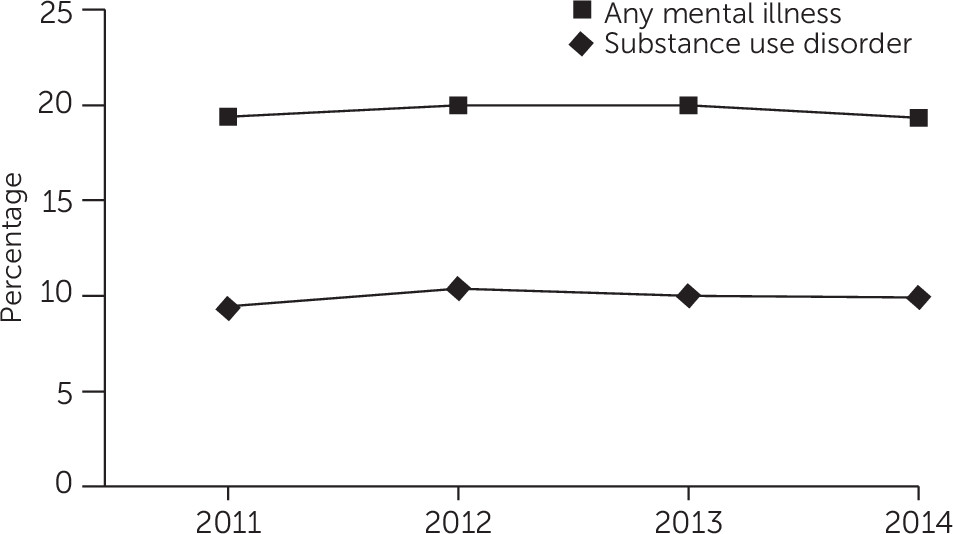
The prevalence of mental and substance use disorders remained relatively unchanged over the study period, at about 20% and 10%, respectively, of all nonelderly adults (
Figure 1).
Across the study period, 39.8% of individuals with mental illness were under age 35, compared with 57.7% of individuals with substance use disorders (
Table 1). Most of those with mental illness were women (61.2%) whereas women were the minority in the substance use disorder group (35.9%). Roughly two-thirds of both groups were non-Hispanic whites. More than half resided in large metropolitan areas. About one-quarter (22.5%) of individuals with mental illness were at or below 100% of FPL, compared with 20.9% of individuals with substance use disorders. An additional 21.7% of individuals with mental illness and 21.5% of individuals with substance use disorders had incomes between 101% and 200% of FPL. About one-quarter (23.5%) of individuals with mental illness self-rated their general health as fair or poor, compared with 14.4% of individuals with substance use disorders. In addition, 19.9% of individuals with mental illness had comorbid substance use disorders and 40.0% of individuals with substance use disorders had comorbid mental illness. Both groups had lower incomes and worse health status than individuals without mental or substance use disorders.
Insurance Coverage Trends
Among individuals with mental illness, the adjusted uninsured rate declined by 5.4 percentage points (p<.01 for difference), from 21.3% to 15.9% (
Table 2). Most of the reduction in the uninsured rate among those with mental illness was attributable to increases in Medicaid coverage, from 16.2% to 19.8%. No significant changes were noted in this group in the rate of private insurance or Medicare and other insurance.
Among individuals with substance use disorders, there was a 5.1-percentage point decline (p<.01) in the uninsured rate, from 25.9% to 20.8%. As with the population with mental illness, Medicaid enrollment accounted for most of the reduction, increasing from 11.6% to 16.0%. No significant changes were noted in private insurance or Medicare or other insurance.
For individuals without mental or substance use disorders, the uninsured rate declined by 4.3 percentage points (p<.01), from 18.6% to 14.3%. Medicaid enrollment increased from 9.1% to 10.9%, and private insurance coverage increased from 67.8% to 69.9% (p<.01 for both).
Changes in insurance coverage were substantially larger among individuals with incomes ≤200% of FPL. The uninsured rate for individuals with mental illness decreased by 10.1 percentage points (p<.01), from 33.2% to 23.1%. For substance use disorders, the uninsured rate decreased by 9.1 percentage points (p<.01), from 39.9% to 30.8%. The uninsured rate among low-income individuals without mental or substance use disorders decreased by 8.6 percentage points (p<.01), from 37.6% to 29.0%. For individuals with substance use disorders in the low-income group, Medicaid was the only type of coverage to significantly increase, but for individuals with mental illness, there were significant increases in Medicaid and private insurance.
Mental Health Treatment Use and Payment Sources
In 2011–2013, 43.0% of individuals with mental illness received any mental health treatment. The rate in 2014 was 45.1%, a 2.1-percentage point increase (p=.04) (
Table 3).
Among those in mental health treatment in 2011–2013, 86.5% of individuals reported receiving psychotropic medications, 57.2% received outpatient treatment, and 7.5% reported residential or inpatient treatment. No significant changes in treatment settings were noted between 2011–2013 and 2014.
A variety of payment sources were reported for outpatient and inpatient mental health treatment (as noted, each individual could report only one source for each, but some individuals used both outpatient and inpatient treatment). In 2011–2013, 14.9% reported Medicaid coverage and 34.1% reported private insurance. Any out-of-pocket payment was reported by 37.3%, and 20.6% reported paying entirely out of pocket. Finally, 36.5% reported other sources of payment. No significant changes in payment sources were noted between 2011–2013 and 2014. All patterns related to use of treatment, setting, and payment source were similar among individuals with mental illness with incomes ≤200% of FPL.
Substance Use Disorder Treatment Use and Payment Sources
In 2011–2013, 9.0% of individuals with substance use disorders received any treatment (excluding self-help programs); the rate was very similar in 2014—9.3%.
In 2011–2013, individuals in treatment used various treatment settings: 49.0% reported outpatient treatment programs, 37.6% reported residential treatment, 25.8% reported receiving treatment in a physician’s office, 40.9% reported receiving treatment in a hospital or emergency department, and 37.4% reported receiving treatment in a mental health clinic. No significant changes in treatment setting were noted between 2011–2013 and 2014.
In 2011–2013, Medicaid was reported as a source of payment for 19.6% of individuals receiving substance use disorder treatment. This increased by 7.4 percentage points (p=.05) to 27.0% in 2014. In 2011–2013, private insurance was reported as a source of payment by 37.2% of individuals. Any out-of-pocket payment was reported by 54.4%, and 22.3% reported paying for treatment entirely out of pocket. Other payment sources (for example, public assistance programs) were reported by 41.5%. No significant changes in payment by private insurance, out of pocket, or by other sources were noted between 2011–2013 and 2014. Treatment patterns were similar among individuals with incomes ≤200% of FPL. No significant changes were noted in use of treatment or in settings visited. There were suggestive but not statistically significant increases in private insurance as a reported source of payment for treatment.
Sensitivity Analyses
Similar to individuals with mental illness and individuals with substance use disorders, those who had co-occurring mental and substance use disorders did not experience any significant change in private insurance, but they did experience large increases in Medicaid enrollment and reduced rates of uninsurance. When viewed by alternative income levels, the decrease in the uninsured rate and increases in Medicaid for individuals in all groups with incomes ≤100% of FPL were larger than changes in the full sample but similar to the group with incomes ≤200% of FPL. Individuals with incomes >200% of FPL experienced much smaller coverage changes than the full sample, as expected because this population is not generally eligible for Medicaid. When SSI recipients and young adults were excluded, coverage changes were relatively similar to those for the full sample. Insurance coverage changes were larger for individuals interviewed in the second half of 2014 than for the full sample. In models with linear and quadratic time trends, we found that quadratic coefficients for insurance coverage were significant, consistent with an inflection point in the trend during the study period, rather than a gradual or consistent change in trend.
Discussion
Insurance coverage gains among individuals with mental and substance use disorders were on par with the population without disorders in 2014, the first year of implementation of the ACA Medicaid expansions and health insurance marketplaces. Medicaid accounted for the vast majority of new coverage among those with substance use disorders and those with mental illness. These populations are more likely than the general population to have low incomes (
18) and thus to be income eligible for expanded Medicaid. By contrast, private insurance significantly increased in only one group—individuals with mental illness who had incomes ≤200% of FPL. Although the ACA has provided new subsidized private insurance options and, in combination with MHPAEA, has reduced discriminatory coverage practice for individuals with mental and substance use disorders, awareness of these options may be limited among high-need populations, and cost may remain a salient barrier.
Mental health treatment use increased by 2.1 percentage points. This is consistent with increased service use among individuals with severe psychiatric distress observed in the National Health Interview Survey (
19). This reduction may be attributable to a reduction in cost-related barriers to care, the most frequently reported reason individuals who need treatment do not receive care (
1). However, even after gaining insurance, many individuals contend with deductibles and copayments that can continue to reduce service utilization.
We did not find any changes in use of substance use disorder treatment. Health insurance reduces the cost of substance use disorder treatment; Medicaid significantly increased as a source of payment among those who used treatment, indicating some financial relief for safety-net providers and self-paying patients. Other barriers not related to cost remain, such as a lack of perceived need for services (
1), limited supply of treatment providers (
20,
21), and stigma (
22,
23). These may require intervention beyond insurance expansion.
Findings add context to current efforts to increase coverage and improve access to care for people with mental and substance use disorders. Campaigns to enroll the uninsured could highlight the availability of specialty services in insurance plans (
24). However, private insurers may be reluctant to increase enrollment of these populations because such individuals account for greater average health care spending (
25). Traditional tools for addressing this spending risk, such as risk adjustment (included in the marketplaces), can mitigate this risk (
26), but additional strategies may be required to account for the excess spending associated with these conditions. Once an individual is enrolled, there is a need to increase treatment receipt. This could include improved screening for possible disorders and linkage to treatment resources in primary or specialty care. For example, care coordination programs have been effective in linking general medical care with specialty mental health and substance use disorder treatment (
27,
28). Ensuring that Medicaid and private insurance plans include provider networks with available specialists to provide these services is essential.
Several limitations should be considered. We did not have access to state-level identifiers and thus could not determine whether changes in coverage and access differed in states that implemented Medicaid expansion in 2014 (California, Connecticut, the District of Columbia, and Minnesota were early expanders—before 2014—under the ACA) versus nonexpanding states. Second, NSDUH does not separately identify ACA enrollment due to the marketplace, just as it does not separately identify individuals enrolled through nongroup plans from employer-sponsored insurance. Third, NSDUH is not well designed to capture out-of-pocket spending related to copayments and deductibles. Out-of-pocket payment is recorded only for mental health care when it is the majority source of payment, and it is recorded only as one of several sources of payment for substance use disorder treatment; the amount is not recorded. Fourth, although NSDUH provides a large national sample, sample sizes were limited to detect effects for smaller subgroups. Self-reported measures may be subject to social desirability biases. The use of computer-assisted interviewing has been found to minimize bias, however.
Conclusions
In 2014, the first year of ACA Medicaid expansions and marketplaces, insurance coverage improved among individuals with mental and substance use disorders. Low rates of treatment utilization persisted, however, especially among individuals with substance use disorders. Care coordination programs within insurance plans and health systems can encourage treatment receipt among newly enrolled individuals.