Mental health problems are the leading contributor to the global burden of disability, representing 29% of the total years lived with disability worldwide (
1). The relevance of these problems has been established in high-, middle-, and low-income countries (
2). In recent years, strategies to organize mental health care have become oriented toward ambulatory mental health care (
3). The World Health Organization actively supports the community model of mental health care (CMMHC) as the best way to organize mental health care (
4,
5). Even though there are examples of successful implementation of CMMHC in countries with various levels of income (
6–
9), including Latin America (
10), implementation as a national strategy is lacking in most low- and middle-income countries (
5).
Evaluations have provided some evidence of the effectiveness of various aspects of CMMHC (
3,
11–
14). However, evidence is lacking about the impact of CMMHC as a whole. This lack is even more notable in middle- and low-income countries, where evidence is needed to inform mental health policies. One frequently studied outcome in these evaluations is reduction in the rate of hospitalizations (
15). However, use of this outcome may not be appropriate in resource-poor contexts, where availability of beds and day hospital care are limited (
16). In these cases, improvements in quality of care or remission and recovery of patients with mental health problems may not be reflected in variations in hospitalization rates. Furthermore, other barriers, such as higher or lower thresholds of referral, may influence hospitalization rates, affecting the utility of this variable as an outcome indicator.
In settings with limited availability of psychiatric beds, the rate of psychiatric emergency visits may more accurately represent the impact of interventions (
17,
18). In addition to documenting actual psychiatric emergencies, the rate of psychiatric emergency visits reflects unresolved demand that has not been addressed in ambulatory care. For example, changes in the rate of psychiatric emergency visits have been observed as a result of changes in the structure of and available resources in the mental health system (
19).
During this study (2006–2011), Chile was classified as an upper-middle-income country; however, the public mental health care sector continues to deal with problems comparable to those in middle-income countries (
20). The mental health system in Chile is largely public and free of charge to users; most services are provided at the primary care level, from which patients can be referred to secondary care if needed. Patients can access emergency services without referral. The national program for mental health, which was enacted in 2001, proposes the progressive implementation of CMMHC (
21). However, various levels of implementation exist across the country, and formal evaluations of the impact of CMMHC have not been conducted.
The purpose of our study was to compare the use of psychiatric emergency services in two geographic areas with higher and lower implementation of CMMHC over a six-year follow-up. Because a high rate of psychiatric emergency visits can be viewed as an indicator of a failure to provide adequate and effective mental health care (
22), we hypothesized that more complete implementation of CMMHC would result in lower use of psychiatric emergency services.
Methods
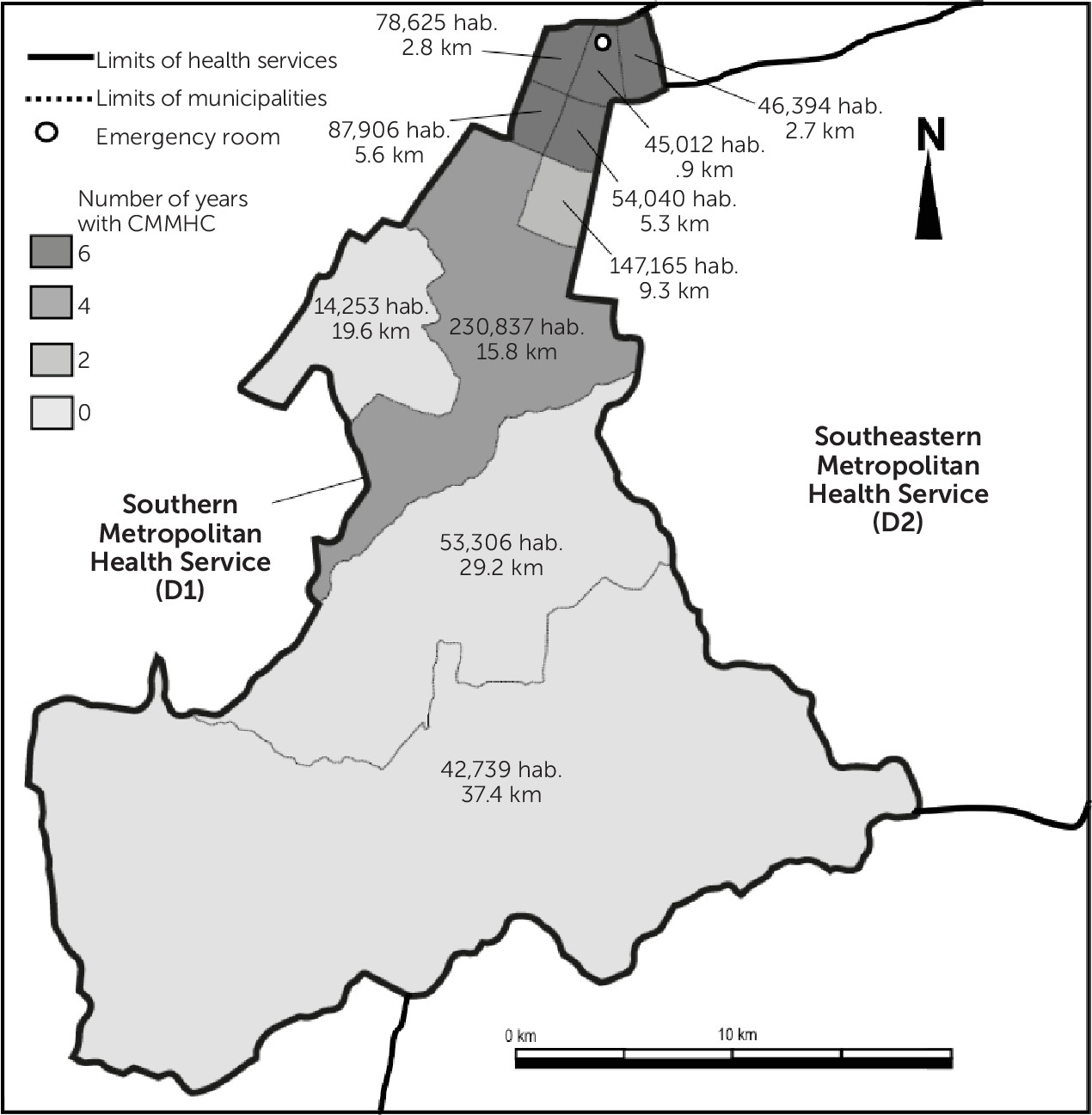
Two comparable geographic and health care administrative districts were compared: the Southern Metropolitan Health Service (district 1 [D1]), which has implemented CMMHC progressively and systematically, and the Southeastern Metropolitan Health Service (D2), which has mostly traditional psychiatric and mental health services based on psychiatric hospitalization and outpatient care adjacent to the hospital. Both districts are large, urban, low- to middle-income sectors located in Southern Metropolitan Santiago, delivering health care to a total of approximately one million inhabitants. Municipalities in D1 are in different stages of development of CMMHC. Each municipality has its own network of primary health care. However, across both territories, only a single emergency room in a general hospital, located in D1, offers specialized psychiatric care. Using data from 2006 to 2011, we compared the number of psychiatric emergency visits in the two health care districts. In addition, we compared D1 municipalities by degree of CMMHC implementation. One municipality was excluded because it has a different administrative government. Overall, ten D1 municipalities were studied.
Sources of Data
Information on psychiatric emergency visits was obtained from routinely collected data from the emergency room. Diagnostic information according to the
ICD-10 was provided by treating clinicians, and other patient information was provided by administrative personnel. The identity and address of the patient were verified by using the patient’s national ID card and previous health records. Data on population size of the districts and municipalities during the study were obtained from the National Public Health Insurance database (
23).
Figure 1 presents information on the population sizes of municipalities in D1. [Tables with demographic data for D1 municipalities are included in an
online supplement to this article.] Distance from a central point in each municipality to the emergency room was measured in linear kilometers by using Google Earth software and included in the analyses.
Definition of Psychiatric Emergency Visit
A psychiatric emergency visit was defined as a visit to any hospital emergency room in the two districts that required a psychiatric evaluation. Visits that were not made for a psychiatric reason were included as long as the visit involved a psychiatric evaluation, and visits that were made for a psychiatric reason were included, even if the final diagnosis was not of a psychiatric disorder. In a sensitivity analysis, a second definition of psychiatric emergency visits was used: only those in which the final diagnosis was F00–F99, according to ICD-10. The results of the first analysis are reported as primary results. In the Chilean context, most visits to the emergency room are initiated by users themselves, who come to the emergency room directly and are not referred by professionals. The patients are attended by residents in psychiatry, who make the diagnosis with the support of attending psychiatrists.
Implementation of CMMHC
CMMHC has been conceptualized in Chile in ways consistent with definitions provided by various authors. Characteristics of the model include delivery of health services that are based on the needs of a local population (public health perspective), are geographically accessible and acceptable (including services that accommodate patient preferences for outpatient care), are based on the objectives and strengths of persons with mental health issues, consider and promote use of a wide and diverse network of community resources and services that have appropriate capabilities, are evidence based, and are focused on recovery and active participation (including participation of persons in decisions related to management of their own mental health problems) (
24,
25).
Implementation of CMMHC in D1 began in 2005. D1 is recognized at the national level for having the only health service that has an explicit community focus in teaching mental health professionals (
26). It has implemented a psychiatric team that provides regular consultancy to the health centers. The health service has assigned responsibility for psychiatric care territorially in each municipality to specific teams in secondary care and has worked to improve continuity of care from the hospital to outpatient care, with the same teams attending to the patient in both settings. In D1, implementation of CMMHC has varied between the ten municipalities. In D2, mental health services are traditionally organized, and most specialized services are provided in the outpatient department of the psychiatric hospital. In D2, development of community-based services, such as psychiatric consultations, is limited. However, we have no reason to assume that the two districts had a significantly different patient profile.
To compare the ten D1 municipalities by degree of CMMHC implementation, they were categorized dichotomously, for each year of study, into those that had “implemented” or “partially implemented” CMMHC. Three key informants, each with more than ten years of service in the health district, classified the degree of implementation on the basis of a shared understanding of the concept of CMMHC. The aspects assessed were whether the responsibility of providing specialized outpatient care was territorially organized, whether a community mental health team provided consultancy services, and whether there was continuity of care from hospital care to outpatient services. There was 78% overall agreement among the three informants, and disagreements were settled by consensus. Most of the disagreements were related to defining which year community teams were incorporated in the respective district.
All ten D1 municipalities had nonspecialized primary care teams that performed screening, diagnosis, and initial treatment (including medication and counseling) of common mental disorders. Most municipalities had access to specialist consultancy for case management, which varied by year of the study. Some municipalities had specialized multiprofessional community mental health services. Psychiatric units for short-stay inpatient care with a limited number of beds, as well as day hospital units, were available. None of the D1 municipalities had early intervention teams, although some had access to services similar to those offered by assertive community treatment teams. In some municipalities, community residential care instead of long-stay inpatient care was available.
Statistical Analysis
Rate and incidence rate ratio (iRR) of psychiatric emergency visits—referring to the ratio of the rates of such visits between the two districts—were calculated by population for both health districts and for each year studied. The rate of psychiatric emergency visits for each district and for each municipality was studied by using quasi-Poisson regression models. In addition, analysis of psychiatric emergency visits between districts and among municipalities was modeled by using a random effect for intercept in order to account for dependency among repeated measures. In this case, a Poisson regression model was allowed by software for the multilevel analysis used (Imer4 for R, version 3.1.1). By using the exponent of regression coefficients, iRRs between municipalities with different levels of development of CMMHC were obtained. To test the hypothesis that municipalities with adequate development (classified as “implemented”) showed a faster decrease in the rate of psychiatric emergency visits, an interaction term between year and “implemented” or “partially implemented” CMMHC was explored. Univariate and multivariate models were conducted, and distance to the emergency room was included as a possible confounding variable.
Two sensitivity analyses were performed. One compared results by using both definitions of psychiatric emergency visits described above. The second analysis used the number of patients rather than the number of visits as the outcome. The number of patients was determined by reviewing all visits for each year according individual’s national identification number. The results of these analyses were robust, and neither the change in definition of visits nor the change in the outcome affected main results.
Results
Total number of psychiatric emergency visits across both districts varied from 4,379 in 2006 to 3,615 in 2011. As a proportion of all emergency visits, the proportion of psychiatric emergency visits did not change significantly from 2006 to 2011: 2.8% of total visits (95% confidence interval [CI]=2.6–3.0).
Figure 1 presents information on the geographical distribution of the ten D1 municipalities, distances to the emergency room in kilometers by municipality, population assigned to each team, and years of implementation of CMMHC.
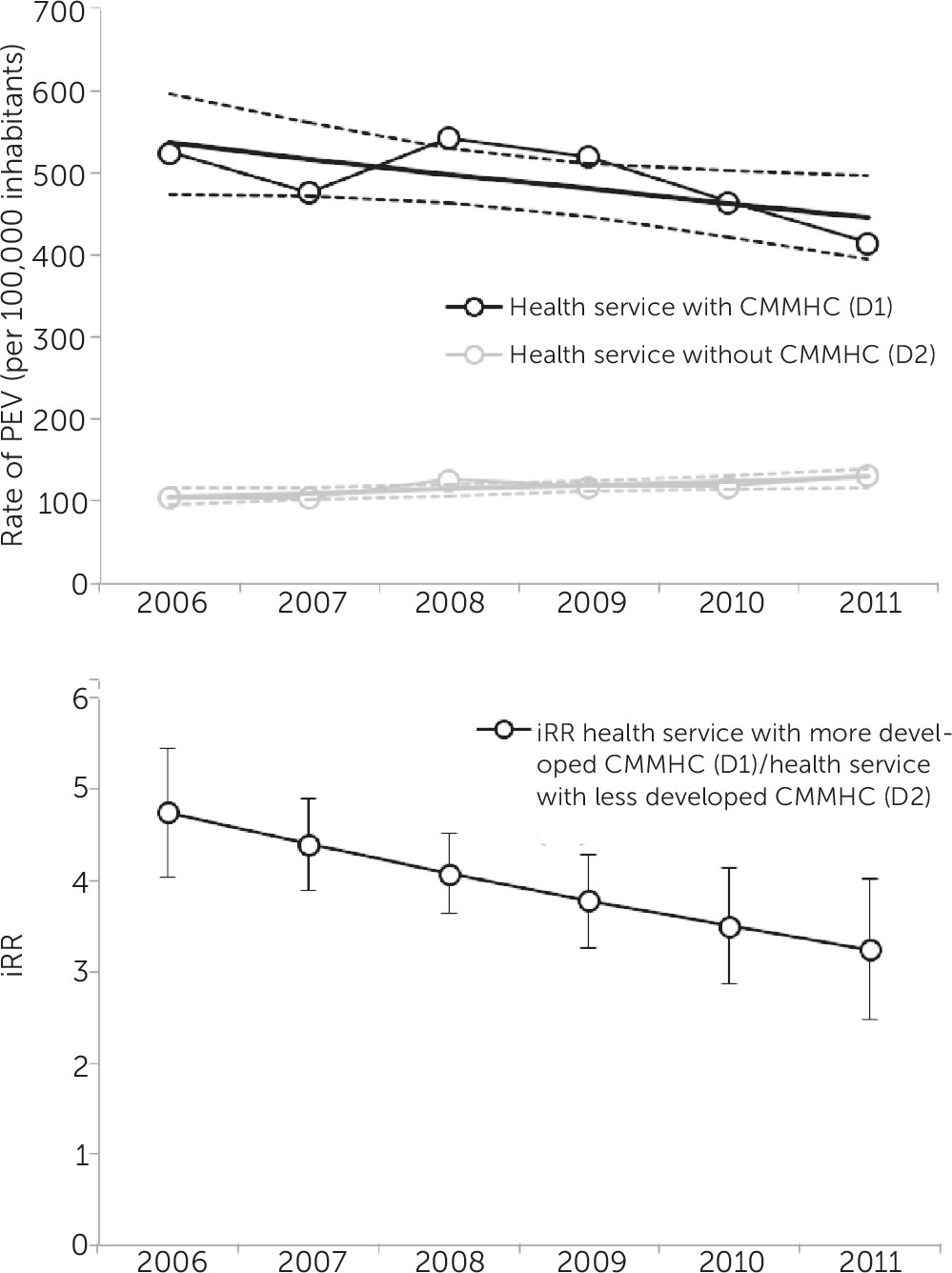
Figure 2 shows the rate of psychiatric emergency visits per 100,000 inhabitants for both districts and the nonadjusted iRRs between both districts. D1 had higher rates of psychiatric emergency visits than D2 during the entire observation period, although a declining tendency was noted, from 541 psychiatric emergency visits in 2006 to 414 in 2011. For D2, the rate increased from 104 in 2006 to 130 in 2011. As the bottom panel in
Figure 2 shows, the nonadjusted iRR between the two districts showed a declining tendency, from 4.7 [CI=4.1–5.5] in 2006 to 3.2 [CI=2.6–4.1] in 2011. This finding indicates that the rate of psychiatric emergency visits in D1 was 3.2 times higher than in D2.
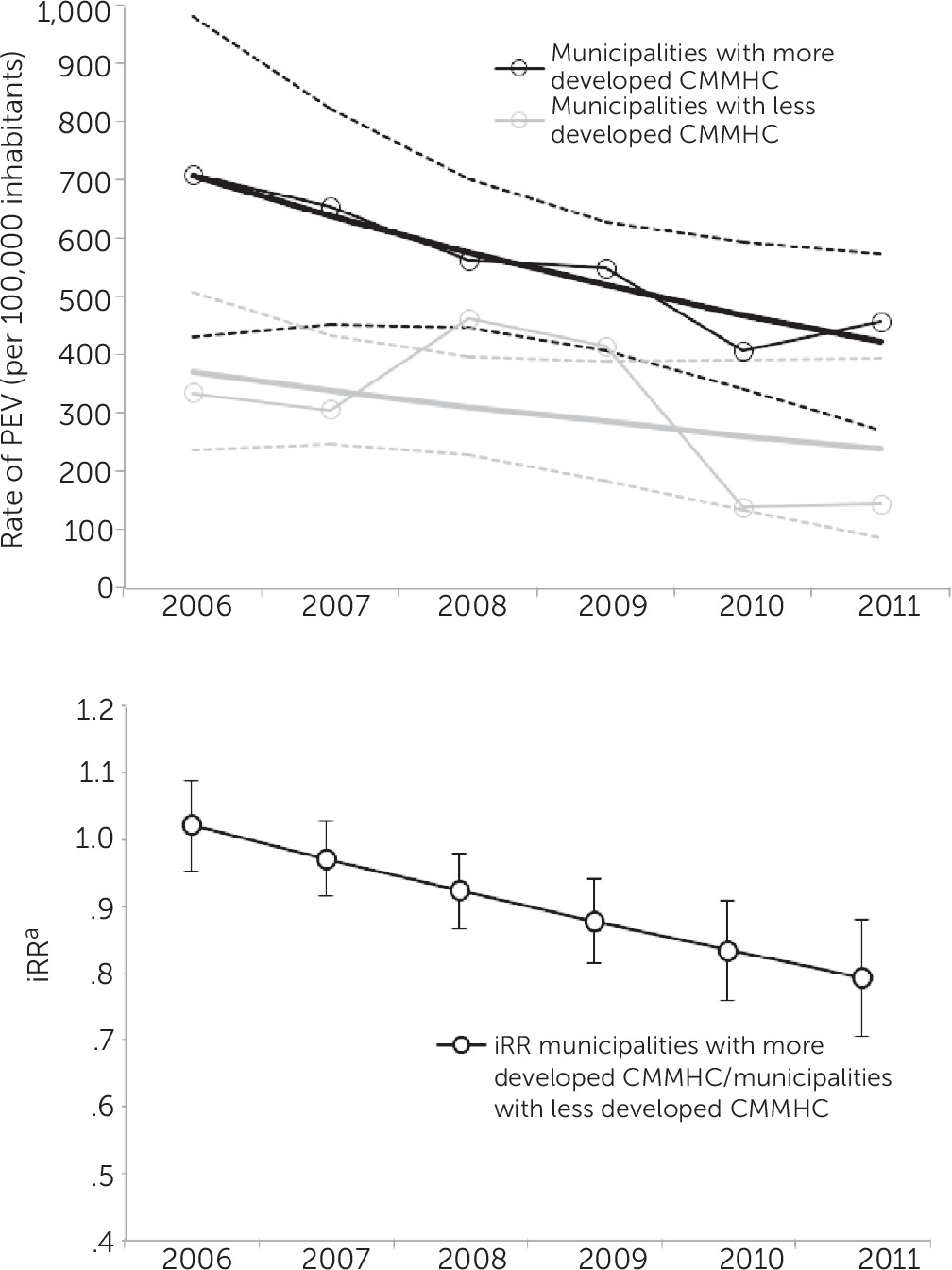
Figure 3 shows the comparison of D1 municipalities and the iRRs adjusted by distance to the emergency room for municipalities with implemented versus partially implemented CMMHC. The rate of psychiatric emergency visits per 100,000 inhabitants was higher in municipalities with more fully implemented CMMHC. The rates were reduced in municipalities with more fully implemented CMMHC and partially implemented CMMHC, but the reduction was smaller in those with partially implemented CMMHC.
Table 1 presents estimated iRRs from the regression analysis comparing the D1 municipalities with different degrees of CMMHC implementation. In the univariate analysis with random effects, psychiatric emergency visits decreased 5% annually across D1. Implemented CMMHC was associated with a lower rate of psychiatric emergency visits (17% lower than the rate in municipalities with partially implemented CMMHC). For every additional kilometer of distance to the emergency room, the rate decreased 5%. The random-effects model took structural factors into account, which is why these results differ from those presented in
Figure 3.
In the adjusted model in
Table 1, the iRRs for the year and distance variables remained almost identical to those in the random-effects model. However, the presence of implemented CMMHC was no longer significant, whereas the interaction between CMMHC and year was significant (p<.01). This finding indicates that the “protective effect” of CMMHC increased over time. In 2006, no differences in rates of psychiatric emergency visits were found between districts with implemented and partially implemented CMMHC, whereas in 2011, the rate in municipalities with implemented CMMHC was 21% lower than in municipalities with partially implemented CMMHC. [The crude data used to create figures and models are presented in a table in the
online supplement.] The results of the sensitivity analyses did not change our main findings (results available on request).
Discussion
The findings of this ecological study from metropolitan Santiago show that the implementation of CMMHC was associated with a progressive reduction in psychiatric emergency visits, at both the district and municipality levels. Our findings are important because we analyzed the implementation of the CMMHC model as a whole, rather than only some of its components.
It is noteworthy that the district and the municipalities with greater development of CMMHC had higher rates of psychiatric emergency visits. However, this could be explained by structural elements, such as the shorter distance to the psychiatric emergency service for the municipalities in D1 compared with D2. Indeed, when the analysis controlled for distance, the association was reversed: implementation of CMMHC was associated with a lower rate of psychiatric emergency visits, and the association appeared to strengthen over time.
The reduction in emergency visits observed in areas in which CMMHC was implemented may be related to various aspects of the model. For example, more frequent follow-up of patients may result in more timely detection of worsening mental health status, allowing for elective instead of emergency interventions (
27). Patients’ closer relationship with the psychiatric team can also provide them with a sense of security, allowing patients to contact the team during working hours instead of resorting to emergency care (
28). Finally, better access to consultancy services at the primary care level has been shown to reduce the number of psychiatric hospitalizations by improving the capacity of the primary care clinicians to treating psychiatric patients (
29).
Comparison With Other Studies
Thornicroft and Tansella (
3) discussed the components of mental health care delivery in a systematic review, and they concluded that the components of CMMHC guarantee the balanced development of both community-based outpatient services and hospital-based services. Another systematic review addressed this issue by focusing on community mental health care interventions in low- and middle-income countries and concluded that, as in high-income countries, community mental health services are associated with better outcomes and lower costs (
30). Similarly, a recent systematic review found that aspects of improved community care are associated with reduced readmission rates (
31). None of the studies included, however, addressed the impact of implementation of CMMHC as a whole; they addressed only some of the model’s components.
As noted above, the most frequently used outcomes in the literature are rate of hospitalization and rehospitalization, whereas psychiatric emergency visits have been less studied. The little evidence that exists is heterogeneous: some studies have found a reduction in psychiatric emergency visits associated with implementation of community-based health care (
32,
33), and others, including systematic reviews, have found no difference (
34,
35). One Dutch study, the setting of which was similar to ours, found an increase in the rate of psychiatric emergency visits after the network of community mental health care was strengthened by the addition of psychiatric nurses (
36).
The impact of structural changes in mental health care on the rate of psychiatric emergency visits has been studied in California, where increased availability of funds in the public mental health system through the Mental Health Services Act reduced the rate of voluntary psychiatric emergency visits in the short term; however, this effect was not sustained (
19). In particular, patients in the full-service partnership model, which incorporates many CMMHC elements, had a reduced likelihood of resorting to psychiatric emergency services (
22). In the same vein, a reduction in the availability of mental health services has been shown to be associated with in an increase in psychiatric emergency visits (
37).
It should be noted that these studies have been conducted in specific settings and with specific populations—for example, among patients with severe psychiatric disorders or among homeless persons. Because our study included general psychiatric patients, comparability with other studies is limited. Moreover, the studies described above were conducted in high-income countries, where undoubtedly conditions are different from those in Chile, not only in terms of level of access to and quality of health care but also in education level and other characteristics of the population.
Limitations
Some limitations of our study should be taken into account when interpreting the findings. The study was ecological, and the analyses were not at the individual level but at the aggregate level (municipality and district). Even though data for 30,000 individual psychiatric emergency visits over six years were analyzed, the visits were grouped and analyzed as larger units for methodological reasons. This limited our ability to control for confounding factors and to draw conclusions at the individual level. One such factor may be disorder severity or the presence of certain diagnoses, such as personality disorders (
38,
39). However, we have no reason to assume that these factors would differ between the districts and municipalities. Second, the degree of CMMHC implementation was assessed dichotomously based on expert opinion, because there were no validated instruments available to assess CMMHC implementation.
Finally, even though distance to the emergency room was taken into consideration, other factors influencing physical access, such as opening times or cost and type of transport, were not included in the analyses.
Conclusions
The results show that CMMHC implementation was associated with a reduced rate of psychiatric emergency visits in metropolitan Santiago. The study demonstrated that implementation of this model can reduce psychiatric emergency visits, which are burdensome to both system users and providers. Future studies should investigate the impact of the model on different mental health outcomes, at both the ecological and individual levels.