Mental disorders are prevalent and impactful in military (
1–
4) and civilian (
5,
6) settings. However, military and civilian research shows that only a fraction of persons with mental disorders seek care (
3,
7–
9). Stigma—a multifaceted phenomenon that involves stereotypes, prejudice, and discrimination (
10)—has been identified as a prominent barrier to mental health care for both military personnel (
11–
13) and civilians (
14,
15). Qualitative studies point to a greater burden of stigma in military organizations, with the military’s focus on toughness and self-reliance as a driving factor (
16,
17).
Another driving factor is that in many nations, military personnel seek care through the military, and clinicians must report significant health-related duty restrictions to the military employer (
18). This might increase the possibility that those in the workplace will become aware of a mental disorder, which opens an additional opportunity for stigma experiences. In addition, because of the stringent health and fitness standards in the military, many of those who develop a mental disorder are found unfit for continued service (
19), which may lead to a potentially undesired premature medical discharge from service (
20). Such a discharge may have important social impacts (such as loss of identity) and economic consequences (such as loss of income and benefits) (
18). Indeed, concerns about negative career or workplace impacts of care seeking are commonly identified barriers to care in the military (
18,
21). Thus military personnel may be more likely to experience stigma, and such stigma may have a disproportionate impact.
Recent research, however, casts some doubt on the centrality of stigma as a barrier to care for military personnel. For example, the prevalence of stigma concerns has declined significantly over the past decade (
22,
23), and most recent military research suggests no association between stigma concerns and care-seeking propensity (
14,
21,
24). There is also emerging evidence of significantly greater mental health care seeking among military personnel compared with civilians, even after adjustment for differences in need (
25), a finding that has been attributed to the investments in military mental health care over the past decade (
25,
26). If these investments have managed to either dramatically decrease stigma or neutralize its effects on care seeking, analogous reinforcements in the civilian mental health system might yield corresponding benefits. These recent findings on stigma and care seeking in the military thus call into question the assertion that military personnel have a disproportionate burden and impact of stigma.
There is, however, little quantitative evidence along these lines, and the lack of highly comparable survey data is the primary impediment (
18). One study from the United Kingdom compared attitudes toward mental illness between military personnel and the general population (
27). Results suggest that these populations are similar overall in terms of attitudes, and the few differences found showed no clear pattern. Specifically, whereas the general population had more positive attitudes toward job rights for those with a mental illness, military personnel had more positive attitudes regarding the causes of mental illness. Importantly, however, the study did not account for differences in the need for mental health care. Also, because these investigators measured only attitudes, the degree to which stigma was actually experienced, along with the impact of such experiences, is not clear (
27).
This study addressed these limitations by using data from two related population-based mental health surveys to examine the prevalence and impact of perceived mental illness–related stigma among Canadian Armed Forces (CAF) personnel and a comparable sample of Canadian civilians.
Methods
Data Sources and Setting
Data were from the 2013 Canadian Forces Mental Health Survey (CFMHS) (
28) and the 2012 Canadian Community Health Survey–Mental Health (CCHS-MH) (
29). Both surveys employed a sampling framework resulting in representative samples of CAF personnel and the Canadian general population, respectively.
The CFMHS was a stratified random sample of all serving CAF Regular Force personnel as well as reservists who were deployed in support of the mission in Afghanistan, although only the Regular Force population was included in the study reported here (N=6,696; overall response rate of 80%) (
28). The CCHS-MH used a cluster sampling approach (N=25,113; overall response rate of 70%) targeting the population of noninstitutionalized individuals ages 15 and older living in private dwellings in Canada’s ten provinces, excluding full-time members of the CAF and persons living on reserves and other Aboriginal settlements (
29). Participants in both surveys were recruited via a telephone call from Statistics Canada interviewers. For both surveys, the primary reasons for nonresponse were noncontact and refusal to participate. Interviews were conducted face to face with 100% of military personnel and 87% of civilians, with additional civilian interviews conducted via telephone. Data for both surveys were collected by using a computer-assisted interview, and the wording of all overlapping content across surveys was identical (
28,
29).
We followed procedures from a recent military-civilian comparison (
30) to restrict the civilian sample in order to approximate the military population. Our restricted civilian sample (N=8,394) excluded those who were not full-time employed, not ages 17 to 60, had recently immigrated (such persons would not have been eligible for CAF service), and had reported any chronic conditions that would typically preclude military service (for example, heart disease or severe obesity). This restricted sample was used for all analyses.
Mental Health Care Seeking
All respondents were asked, “Have you ever received treatment for an emotional or mental health problem?” and whether this was during the past 12 months.
Perceived Stigma and Impacts of Stigma
Respondents who reported mental health care seeking in the past 12 months completed the Mental Health Experiences Scale (
15), which assesses the experience and impacts of stigma. Respondents were first asked the following question regarding perceived stigma: “During the past 12 months, did you feel that anyone held negative opinions about you or treated you unfairly because of your past or current emotional or mental health problem?”
Respondents who endorsed perceived stigma also rated how much these perceptions of negative opinions or unfair treatment affected them over the past 12 months in each of six domains: family relationships, romantic life, work or school life, financial situation, housing situation, and health care for physical health problems. Each question was rated on a scale of 0, not affected, to 10, severely affected. These scores were then summed into an overall impact score. Possible overall scores ranged from 0 to 60, with higher scores indicating greater impact of stigma. For this study, we considered those who did not report perceived stigma to have no impact of stigma. In our analyses, we examined the mean overall impact score and mean score in each impact domain.
Sociodemographic Characteristics
Sociodemographic variables included sex, age category (<25, 25–34, 35–44, and >44), race (white versus nonwhite), marital status (single, married or common law, and separated or divorced), household income category (<$50,000, $50,000–$99,999, $100,000–$149,999 and ≥$150,000), and highest educational attainment (less than secondary, secondary only or some postsecondary, and postsecondary completion). These groupings were chosen on the basis of the survey content, the distribution of respondents, sample size in each of the subgroups in the two populations, and conceptual considerations.
Need-Related Characteristics
We used several measures common to both surveys to adjust for differences in the need for mental health care in the two populations.
Mental disorders.
The World Health Organization Composite International Diagnostic Interview (WHO-CIDI) (
31) was used to assess the presence of the following past-year mental disorders on the basis of
DSM-IV criteria: major depressive episode, generalized anxiety disorder, and alcohol use disorder (that is, alcohol abuse or alcohol dependence).
Suicidal ideation.
Suicidal ideation was assessed by asking respondents whether they had “seriously thought about committing suicide or taking [their] own life” in the past 12 months.
Psychological distress.
The Kessler Psychological Distress Scale (
32) was used to assess overall levels of psychological distress experienced during the past 30 days. The ten items were rated on a 5-point scale and summed to create a total distress score. Possible scores range from 0 to 40, with higher scores indicating higher levels of distress. For this study, we trichotomized distress scores on the basis of cutoffs reported in Australian population research (
33): low, 0–5; moderate, 6–19; and high, 20–40.
Statistical Analyses
SAS version 9.3 and Stata version 13.1 were used for data analysis. We used modified Poisson regression to examine the effect of population (military versus civilian) on the likelihood of mental health care seeking and perceiving stigma, and we used linear regression to examine the effect of population on the level of stigma impact (overall and in each domain). For all analyses, we examined the effect of population in an unadjusted model, followed by a model controlling for sociodemographic characteristics (partially adjusted model) and a model controlling for sociodemographic characteristics as well as variables related to the need for care (fully adjusted model).
Listwise deletion was used for missing data in all regression models, which resulted in the exclusion of cases representing between .5% and 4.7% of the population. The CFMHS and CCHS-MH include survey weights provided by Statistics Canada that ensure representativeness of the samples and account for nonresponse. Variance estimates for all analyses were calculated with bootstrap methods using 500 replicate weights provided by Statistics Canada (
28).
Ethical Aspects
The relevant policy and review committees within Statistics Canada reviewed and approved all aspects of data collection (including ethical aspects) and all conditions of data access and use. Participation in the surveys was voluntary, and participants provided informed consent.
Results
As shown in
Table 1, there were important disparities in terms of sociodemographic characteristics between military personnel and civilians. The military sample had a higher proportion of males (86.1%), compared with the overall (49.3%) and restricted (57.9%) civilian samples. Military personnel were younger, with only 21.4% ages 45 and older, compared with 51.5% and 38.8% in the overall and restricted civilian samples, respectively. The military sample had a much smaller proportion of nonwhite persons: military, 9.9%; overall civilian, 20.4%; and restricted civilian, 22.1%. Large differences were apparent in the income distribution across populations. Only 6.6% of military personnel earned less than $50,000, compared with 35.2% and 19.8% in the overall and restricted civilian samples, respectively. Finally, the military sample had a lower proportion with less than a secondary school education (military, 4.1%; overall civilian, 18.1%; and restricted civilian, 8.1%) and a higher proportion with only a secondary education or some postsecondary school (military, 34.6%; overall civilian, 22.9%; and restricted civilian, 21.5%).
Table 1 also shows a number of differences in the prevalence of factors related to the need for mental health care among military personnel and civilians. A greater proportion of military personnel had a major depressive episode (military, 8.0%; overall civilian, 4.7%; and restricted civilian, 3.5%), generalized anxiety disorder (military, 4.7%%; overall civilian, 2.6%; and restricted civilian, 1.7%), suicidal ideation (military, 4.3%; overall civilian, 3.3%; and restricted civilian, 2.3%), as well as moderate or high psychological distress (military, 45.3%; overall civilian, 35.2%; and restricted civilian, 32.0%).
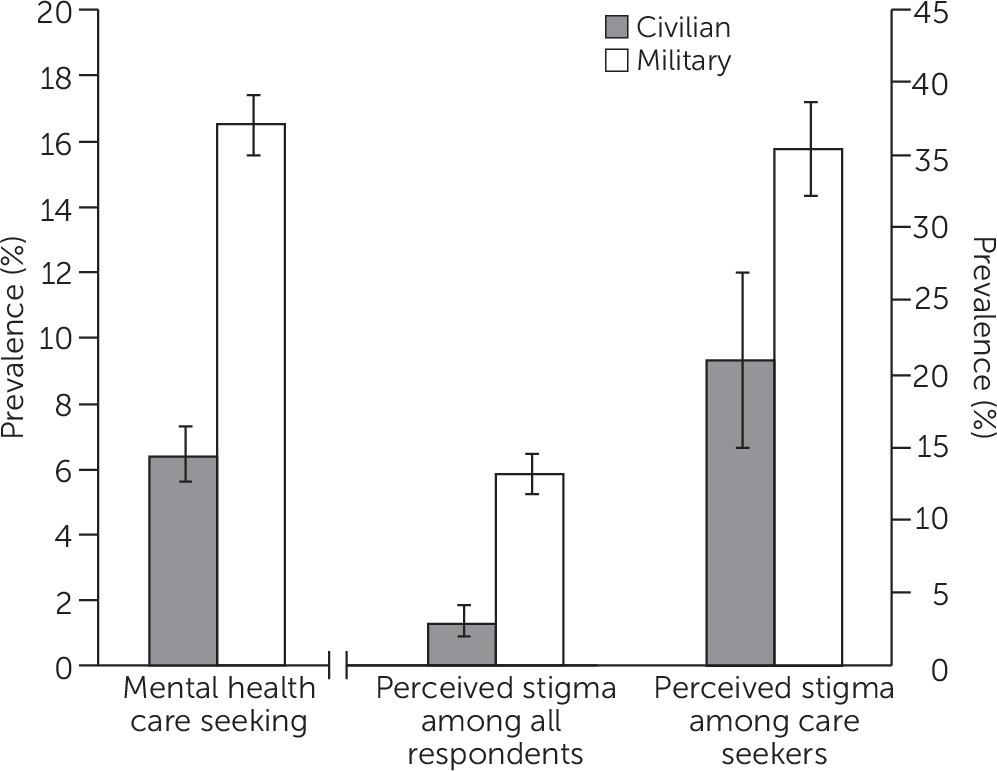
Mental health care seeking in the past 12 months was reported by 1,075 military personnel and by 631 civilians. Unadjusted prevalences for mental health care seeking and perceived stigma are shown in
Figure 1, and unadjusted mean scores for the impact of stigma are shown in
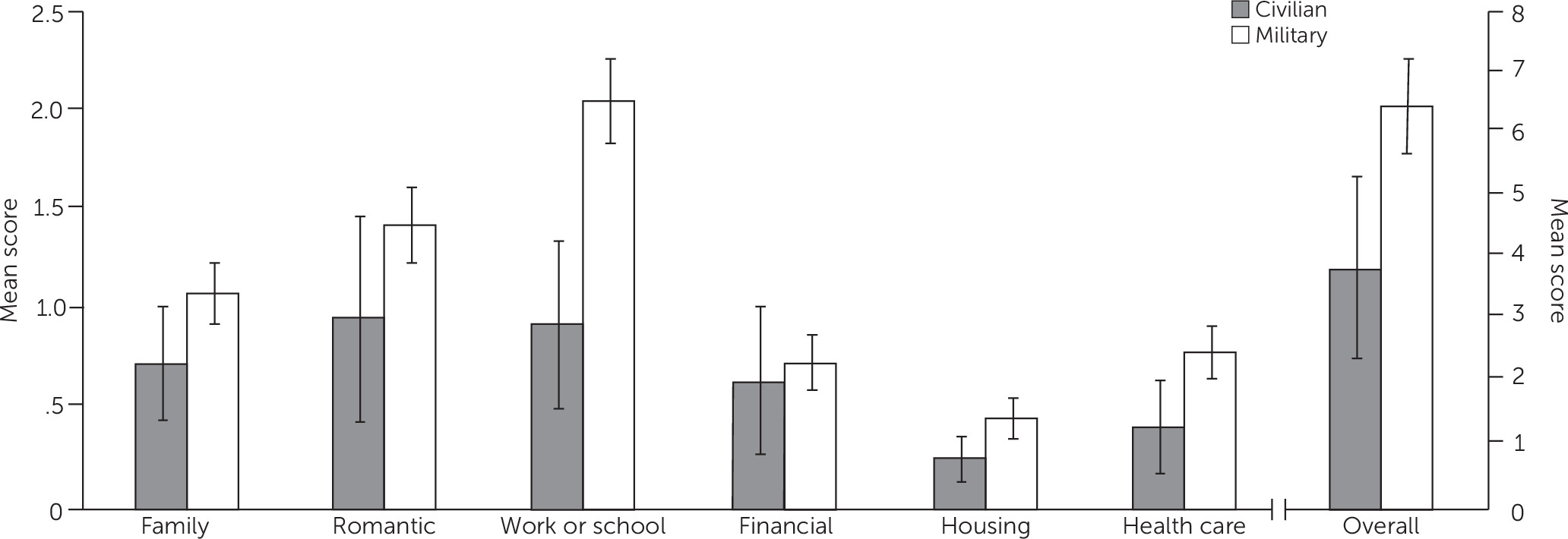
Figure 2. Unadjusted and adjusted results from regression analyses are presented in
Table 2 (care seeking and perceived stigma) and
Table 3 (impact of stigma). Military personnel were significantly more likely than civilians to report care seeking in the past year (16.4% versus 6.4%), even after the analysis controlled for sociodemographic characteristics and need for care (adjusted prevalence ratio [PR]=1.86). Military personnel were also significantly more likely than civilians to perceive mental health stigma in the past year (35.4% versus 21.0%), even after the analysis controlled for sociodemographic characteristics and need for care (PR=1.70).
Military personnel also reported a higher overall impact of stigma than did civilians (mean score of 6.42 versus 3.80), even after the analysis controlled for sociodemographic characteristics and need for care (p=.040) (
Figure 2). Examination of the relative impact of stigma in each domain showed that the greater overall impact reported by military personnel was particularly pronounced for work or school life (mean score of 2.03 for military personnel versus .91 for civilians) (
Figure 2). Again, this difference was significant after the analysis adjusted for sociodemographic characteristics and need for care (p<.001).
Discussion and Conclusions
Using highly comparable, recent survey data for Canadian military personnel and civilians, we found that perceived stigma related to mental illness was significantly more prevalent among military personnel compared with civilians, even after adjustment for differences in sociodemographic characteristics and need for care. Stigma had a significantly greater impact on military personnel, particularly in the domain of work or school life. Finally, we confirmed recent findings suggesting greater use of mental health services among military personnel compared with civilians, even after adjustment for the greater need for care in the military population.
Our findings are not consistent with those of Forbes and colleagues (
27), who did not find dramatic or consistent differences in stigmatizing attitudes toward mental illness between military personnel and their civilian counterparts in the United Kingdom. Although this divergence may be attributable to differences in the prevalence of stigma across military forces in Canada and the United Kingdom, the available data point to, if anything, greater stigma in United Kingdom military personnel compared with Canadian military personnel (
34). A more likely explanation may involve differences in measurement of the underlying attitudes. Indeed, our study examined perceived experiences of stigma among those who had sought mental health treatment, rather than attitudes toward mental illness in the whole population. Forbes and colleagues (
27) were able to adjust only for age and sex, whereas we adjusted for a broader range of confounders known to be strongly associated with perceived stigma and to differ in prevalence in military and civilian populations, notably the presence of mental disorders (
30).
Taken together, our findings are in line with a recent review of military research indicating that among the most commonly endorsed concerns about seeking treatment for a mental health problem were “my unit leadership might treat me differently,” “members of my unit might have less confidence in me,” and “it would harm my career” (
21), all of which may be reasonable concerns for military personnel. Our results are also consistent with qualitative findings of a study in which military personnel articulated an occupation-specific burden of mental illness–related stigma and its prominence as a barrier to care (
35). In addition, a greater care-seeking propensity among military personnel makes sense conceptually in light of the greater access to care in the military mental health care system (
25).
Strengths and Limitations
This study had a number of strengths. For instance, we used data from two recent, contemporaneous, population-based surveys with high response rates, highly comparable methods, and identical survey items. Also, we employed robust methodological procedures, including sample restriction to create a sample of Canadian civilians that was more comparable to the military population as well as adjustments for key sociodemographic characteristics and variables related to the need for mental health care.
Several limitations must also be acknowledged. First, the stigma items were asked only of individuals who reported accessing mental health services in the past year. That is, individuals with mental health problems who did not seek treatment but who may nevertheless have experienced stigma were not reflected in the analysis. The population burden of perceived stigma may therefore have been systematically underestimated in both populations. However, individuals may avoid seeking treatment in order to avoid being stigmatized (label avoidance) (
36), which may mean that those who do not seek care are actually less likely to report stigma and which may suggest that we, in fact, overestimated the proportion of individuals who perceived stigma. Second, the two surveys did not measure all of the same mental disorders, and thus we were able to include only three past-year disorders in our adjustments. Importantly, the WHO-CIDI posttraumatic stress disorder (PTSD) module was not included in the civilian survey; this disorder likely plays a large role in stigma experiences in the military (
18,
35). We did, however, adjust for additional markers of need for care (for example, psychological distress) to compensate for the non-inclusion of the PTSD module for civilians. Given that the prevalence of some disorders is greater among military personnel than among comparable civilians (
30), our approach likely undercontrolled for this excess prevalence. However, the essence of our findings remained unchanged after we additionally controlled for a self-reported diagnosis of PTSD as a chronic health condition and for perceived unmet need for care. Third, the amount of variance explained by models predicting the impact of stigma was relatively low, and we acknowledge the possibility of residual confounding in these analyses. Fourth, we could assess only perceived stigma experiences, and we had no knowledge of the factual circumstances behind those perceptions. Finally, our findings may not generalize to other nations and their military forces.
Implications
In this study, we found a much greater perceived burden of stigma in the military, a population that proved to be more likely to seek care. This apparent discrepancy suggests that the relationship between stigma and care seeking may differ between military personnel and civilians. It is possible that in military samples, factors other than stigma attenuate any negative effect of stigma on care seeking (
37). For example, CAF mental health literacy efforts that enhance recognition of the need for mental health care (
25) might have more than counterbalanced any negative effect of greater stigma. Indeed, recognition of need is one of the pillars of the CAF’s program, and there is strong evidence from 2002 CAF data that failure to recognize need was a leading barrier to care (
7). Our findings thus point to the potential power of interventions other than the direct destigmatization efforts that have been the focus of recent efforts to neutralize the effects of stigma on care seeking in military and other populations.
A second and less encouraging hypothesis is that in the military, stigma is a consequence of care seeking, not an antecedent. Mental health literacy and destigmatization efforts may have led not only to improved attitudes toward mental illness (
22,
38) but also to greater care seeking (
37), and those seeking care may be much more likely to perceive stigma after seeking care. This coheres with our findings on the disproportionate impact of stigma experiences in the military, especially in the workplace. If stigma and its impacts are indeed more often a consequence than an antecedent of care seeking in the CAF, then there could be opportunities to intervene and minimize negative consequences. If the underlying experiences reflect unfair application of medical standards, or if unfair treatment occurs in other domains (for example, promotion), there might also be opportunities to obtain more favorable results—in military organizations and in other workplaces.