Management of pediatric mental disorders is an important public health concern because mental and behavioral disorders can affect physical, emotional, and social development throughout the lifespan (
1–
4). Approximately 20% of youths in the United States experience at least one mental health condition during their lifetime, and 10% of youths with emotional disturbance may face functional impairments (
3). Compared with privately insured youths, youths treated in the public sector are at higher risk of serious emotional or behavioral disorders (
5,
6) and thus are more likely to receive mental health services (
7).
Over the past several decades, mental health care utilization has increased rapidly among youths diagnosed as having a psychiatric disorder (
8–
10). However, these services are often fragmented and disconnected (
1,
7,
11–
13) and thus result in inefficient care and higher costs (
14). In the past 20 years, the wraparound practice model has emerged as one of the more promising approaches for strengthening the system of care for youths with mental disorders. This practice model uses a team-based, child-centered planning process to maintain youths in community settings. The model with 10 specific core values aims to strengthen the planning process and facilitate links between agencies and health care professionals (
15). Implementation of this practice model could vary across communities (
16,
17). In Maryland, wraparound services have been implemented as part of a care management entity, a nonprofit organization that coordinates a care planning team, delivers individualized health services for youths and their families, and facilitates community-based and home-based supportive services. Introduced in the state through the 2009 Children's Health Insurance Program Reauthorization Act demonstration grant, the wraparound practice model was implemented within a care management entity infrastructure that targeted Medicaid-enrolled youths with serious mental health needs (
18).
Extensive evidence has shown the wraparound practice model can improve psychiatric symptoms, school performance, and juvenile justice involvement. This further translates to medical cost savings from reduction in inpatient care and sustainability of health services (
19–
23). For example, a recent study of the impact of a wraparound practice that uses a care management entity model found that youths enrolled in the program were more likely to use outpatient clinic services compared with youths enrolled in the usual source of care (
24), suggesting that wraparound services could facilitate access to community-based care.
Studies demonstrate that wraparound services delivered by a care management entity may improve outcomes for youths with severe emotional or behavioral disorders. However, most investigations focused on the period during which youths were receiving coordinated care services, and—to our knowledge—none have examined outcomes following discharge from care (
22,
25–
28). Care coordination for youths with complex mental health needs is expected not only to affect outcomes in the short-term but also to have a long-term impact on use of community-based services. The expectation is that participants will not need inpatient or emergency care services after they exit from the care management entity program. In this regard, knowledge of outcomes after youths exit such programs carries important implications for long-term program investment.
This is a novel study that leveraged a quasi-experimental design to examine the impact of the care management entity model on use of acute psychiatric services one year after discharge from the care management entity’s services. Care coordination was provided on a first-come, first-served basis because of financial constraints and workforce capacity. We hypothesized that youths served in the care management entity model would have fewer emergency department (ED) visits and hospitalizations after discharge compared with a group of youths with severe mental or behavioral conditions who did not receive services from a care management entity.
Methods
Study Design
This was a retrospective cohort study that used a pre-post design to examine the impact of the care management entity model on clinical outcomes among youths with severe mental or behavioral conditions. The study cohort comprised youths served by the care management entity and a comparison group of youths with similar demographic characteristics and psychiatric diagnoses at baseline (i.e., prior to entry into the care management entity).
Study Participants
The care management entity cohort was selected from youths served in a care management entity model anytime from December 2009 through December 2013. The study inclusion criteria were age 20 years or younger at the time of enrollment in the care management entity, continuous Medicaid eligibility for at least 365 days prior to enrollment, involvement in care management entity services for at least 30 days, and continuous Medicaid eligibility for at least 365 days after discharge from the care management entity. In the care management entity administrative data, approximately 20% of participants who met the age criterion for the study (N=121) had missing discharge information. Rather than restrict the sample to participants with complete data, we performed multiple imputation to impute the length of stay in care management entity services, which allowed us to estimate the missing discharge dates (
29–
31). [Detailed data imputation steps are described in an
online supplement to this article.]
The comparison cohort was selected from the Medicaid-enrolled youths who resembled youths enrolled in the care management entity but who themselves were not enrolled in coordinated care services. The selection for the comparison group was based on a hierarchy of severe mental disorders (i.e., schizophrenia, bipolar disorder, and major depressive disorder) and on a hierarchy of foster care, disability, and low-income Medicaid eligibility. This process ensured that the comparison sample properly reflected the distribution of the care management entity cohort.
To create a comparable service period for the two groups, each member of the comparison group was assigned the enrollment and discharge date of a randomly selected member of the care management entity cohort. The use of random assignment with replacement avoids imbalances between the distribution of youths enrolled in the care management entity and the comparison group during the window of time allotted for observation (
32). Once the enrollment date and the respective discharge date were assigned, similar inclusion criteria were applied to the comparison cohort: ages 20 years or younger at the enrollment date, continuous Medicaid eligibility for at least 365 days prior to date of enrollment and continuous Medicaid eligibility for at least 365 days after the index date, defined as the date of care management entity discharge.
[An illustration of the overall procedure for cohort selection is available in the online supplement.]
Data Sources
The data comprised care management entity administrative records linked with Medicaid claims for youths enrolled in the entity’s services from December 2009 through December 2013. The youths’ age, gender, race, and enrollment information, such as dates of enrollment in and discharge from the care management entity and the agency subsidizing care coordination services (for example, public child welfare, juvenile justice, and public mental health services), were derived from the administrative records of the care management entity.
Medicaid claims included three separate files: Medicaid enrollment, pharmacy, and medical service claims. Medicaid enrollment claims provided information on the Medicaid eligibility category (e.g., foster care). Medicaid pharmacy claims were used to identify psychotropic medications dispensed in outpatient settings. Medical service claims included claim type (general medical or mental health), service type (inpatient, outpatient, physician, special services, or home health), ED visit, and diagnosis for each claim. Diagnoses were recorded according to the ICD-9, and clinical procedures were recorded by Current Procedural Terminology codes.
Outcome Measures
The two study outcomes, identified from Medicaid medical service claims, were psychiatric-related ED visits and hospitalizations. The outcomes were measured one year after discharge or the index date. Each outcome measure was operationalized as a dichotomous variable of any use and as a count variable of the number of visits for each of the psychiatric services.
Covariates
Demographic characteristics.
Age, gender, race, and Medicaid eligibility category at the time of discharge from the care management entity were obtained from Medicaid enrollment files. Race was classified as African American, white, and other (Asian, Native American, and Pacific Islander). Medicaid eligibility category was classified as Supplemental Security Income (SSI), Temporary Assistance for Needy Families (TANF), foster care or adoption, and all others (e.g., home- and community-based services waivers, families with incomes up to 138% of federal poverty level, enrollment in Maryland children’s health program, and long-term care).
Psychiatric diagnosis.
Psychiatric diagnoses were obtained from Medicaid medical (inpatient and outpatient) service claims one year prior to the discharge or index date. We used the ICD-9 diagnostic codes to determine the presence of schizophrenia, bipolar disorder, attention-deficit hyperactivity disorder (ADHD), anxiety, depression, conduct disorder, impulse control disorder, and oppositional defiant disorder.
Psychotropic medication.
Psychotropic medication use one year prior to the discharge or index date was obtained from Medicaid pharmacy claims. Medications within the following psychotropic therapeutic classes were included: antipsychotics, medications for ADHD (e.g., stimulants and atomoxetine), antidepressants, lithium, and mood-stabilizing anticonvulsants (e.g., carbamazepine, valproic acid, and lamotrigine). Concomitant antipsychotic use was defined as an overlap of two or more antipsychotic agents for more than 30 days. The 30-day period was used to avoid classifying all simultaneous use of more than one antipsychotic as concomitant use, for example, cross-tapering from one antipsychotic to another.
Inverse probability treatment weighting.
Inverse probability treatment weighting is commonly used to minimize confounding in observational studies of clinical interventions. First, the propensity score was estimated from a multivariable logistic regression model by using baseline demographic and clinical characteristics from one year prior to the index date. Covariates used in the prediction model were described in the prior section. Asymmetrical trimming of the propensity scores was restricted to the fifth and 95th percentiles on the basis of the propensity score distribution for the youths enrolled in the care management entity and the comparison group, respectively (
33). We did not include the outcome measures (i.e., psychiatric-related ED visits and hospitalizations) in the model because of the high correlation between the outcomes and psychiatric diagnoses and use of psychiatric medications.
The next step was to use the propensity score to calculate the inverse probability treatment weighting for individual youths (
34). The cohorts were adjusted by using this weighting process, and the adjusted cohorts were used in all analyses.
Statistical Analysis
Differences in characteristics between the youths enrolled in the care management entity and the comparison group were examined by using chi-square tests for categorical variables and t tests for continuous variables. Two models were applied to investigate the association between enrollment in care management entity services and psychiatric-related ED visits and hospitalizations after discharge (
35). In model 1, generalized linear models were used to compare the likelihood of change of using services between the youths enrolled in a care management entity versus the comparison group. The models were fit via generalized estimating equations and were employed with a logit link. Model 1 also adjusted for demographic and clinical profiles one year prior to the index date. The difference-in-difference (DID) estimator was used to test whether the care management entity program had influence on the change of psychiatry-related ED visits and hospitalizations.
In model 2, we examined the association between participation in the care management entity and number of psychiatric services among youths with at least one service visit. Furthermore, we specified a zero-inflated negative binomial distribution in the regression model because the number of visits was considered to be overdispersed (
36–
38). A negative binomial distribution is commonly used to address the overdispersion issue.
Data are presented as odds ratios (ORs) in model 1 and as incidence rate ratios (IRRs) in model 2 in order to report the association between care coordination by a care management entity and the clinical outcomes. Analyses were performed with SAS, version 9.3. All p values were two-sided, and values of <.05 were considered statistically significant. The study was approved by the University of Maryland Institutional Review Board. Tabulated data of less than or equal to 10 for any given cell were not reported, in accordance with the data use agreement and HIPAA.
Results
After the cohorts were adjusted with treatment weighting, a total of 488 youths in the care management entity program and 1,893 youths in the comparison group were included in the analyses. In general, almost three-quarters (72.6%) of youths were ages 13 and older, and over half were male (60.8%), were African American (63.1%), and were enrolled in either the SSI or the TANF Medicaid eligibility category (64.0%). By nature of the adjustment with inverse probability treatment weighting, most of the characteristics were balanced between the two groups (
Table 1).
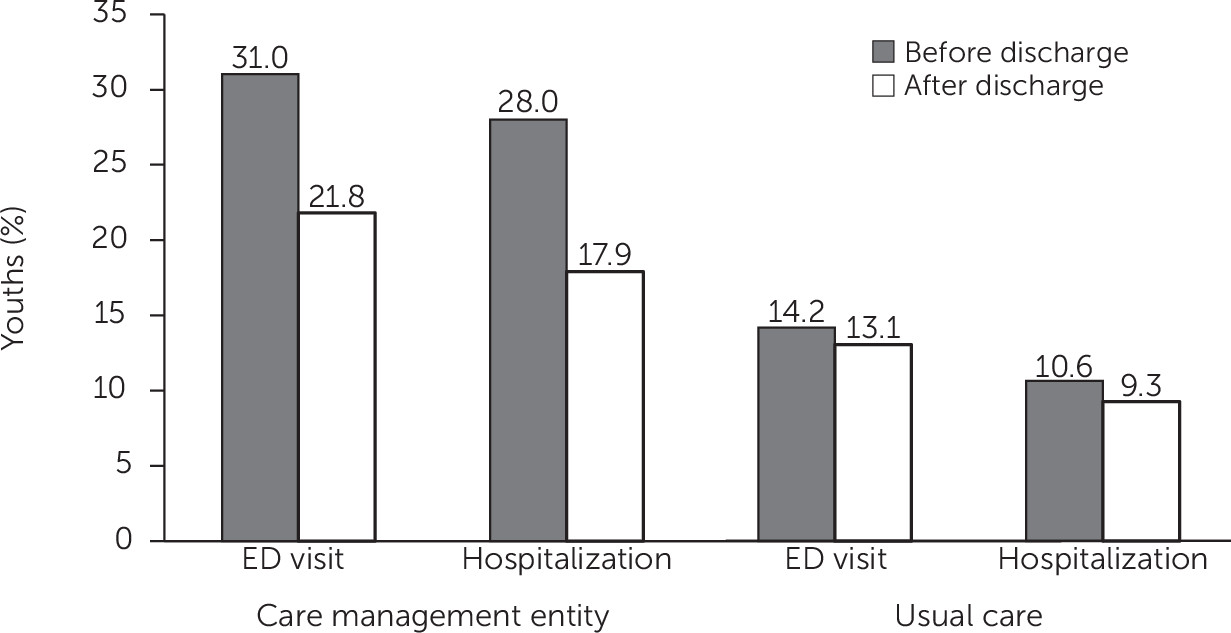
Of the 488 youths in the care management entity program, 31.0% had at least one psychiatry-related ED visit and 28.0% had at least one hospitalization in the year prior to discharge (
Figure 1). Among youths in the care management entity program, there was a reduction in the use of psychiatric services in the year after discharge compared with the year before discharge, a difference of –9.2% for ED visits and –10.1% for hospitalizations. For the comparison group, by contrast, the differences in use of psychiatric services before and after discharge were negligible, a difference of –1.1% for ED visits and –1.4% for hospitalizations. The unadjusted mean±SD number of ED visits by youths in the care management entity program decreased from .73±1.47 before discharge to .46±1.34 after discharge. The number of hospitalizations among CME youths fell from .76±2.68 to .52±2.21. For the comparison group, no difference was observed before and after discharge in ED visits (from .26±.88 to 23±.83) or hospitalizations (from 20.±88 to .20±1.31).
Because some baseline characteristics remained unbalanced, a covariate adjustment was used in model 1 and 2.
Table 2 presents the ORs and 95% confidence intervals (CIs) from model 1.The DID estimators indicated that the likelihood of having any psychiatry-related ED visit (OR=.65) or hospitalization (OR=.60) after discharge (versus before) was significantly lower among youths in the care management entity than in the comparison group.
The IRRs in
Table 3 were derived from the youths who received at least one visit for each psychiatric service in the year after discharge and were adjusted for demographic and clinical characteristics. Almost all baseline characteristics remained balanced in the reduced population [see
online supplement]. The results showed that there was no significant association between enrollment in the care management entity and the number of ED visits or hospitalizations. However the Medicaid eligibility category at discharge was found to be a strong predictor of the number of psychiatric services for the two study outcomes. For example, youths in the foster care system experienced fewer hospitalizations compared with youths in the TANF program (IRR=.78).
Discussion
To our knowledge, this is the first study of Medicaid administrative claims to analyze use of psychiatric services among youths after they were discharged from a coordinated care model to a usual source of care in the community. Our findings suggest that the coordinated care model was associated with a lower likelihood of the use of any psychiatric ED visits and hospitalizations within a year after youths were discharged from the program. However, for those who received psychiatric services, no differences were observed between the two groups with respect to the number of ED visits or hospitalizations.
There are several explanations for the nonsignificant effect of the coordinated care model on the number of ED visits or hospitalizations among users of psychiatric services. First, the small sample size, especially for youths who had at least one ED visit postdischarge, could affect statistical power to detect a difference. Second, youths who had any psychiatric ED visit or hospitalization might have more complicated mental health situations than youths who did not use any of these services, and thus the effects of the care management entity model might differ depending on the severity of the mental health condition. Third, it is possible that other factors had a stronger association with the use of these psychiatric services and thus offset the effect of the care management entity model. In this study, we observed that Medicaid eligibility category at discharge was significantly associated with the number of psychiatric hospitalizations, even after the analyses controlled for other covariates, which aligns with prior research that used the National Medical Care Utilization and Expenditure Survey (
39).
The study results are relevant to state agencies and administrators for future program implementation, for a number of reasons. Most important, our findings demonstrate that the care management entity model was associated with sustained reductions in use of acute psychiatric services—participants in the program had greater reductions in use of psychiatric services following discharge compared with youths who did not receive services from a care management entity. From an administrative perspective, acute psychiatric services not only incur greater costs to the public mental health system but also are indicative of mental health crises and instability. Second, the study found that youths in the child welfare system, such as foster care and SSI, had fewer hospitalizations compared with youths receiving TANF. It is possible that these findings were influenced by the role played by the youths’ case workers, which may complement the role of the care coordinators from the care management entity.
Third, youths who were in the care management entity model for at least one year had higher utilization of psychiatric services compared with the comparison group (data not shown). Prior research has similarly found that receipt of wraparound services was associated with a higher likelihood of an inpatient admission or ED visit as well as a higher number of outpatient clinic visits while youths were in care. The wraparound practice might facilitate mental health care access; however, further research is needed to confirm this hypothesis. Finally, the delivery of wraparound services within the care management entity model highlights the importance of collaboration across multiple agencies. Data linkage between Medicaid claims and the care management entity’s administrative records, and possibly linkage to other service systems, would enrich the data for assessing youths’ outcomes.
The study had limitations that should be considered. First, information on fidelity to the wraparound practice model was not available when the analyses were conducted. Another study conducted interviews with youths, families, and collaboration team members to measure the fidelity of the wraparound model. Using the National Wraparound Initiative definition, the study found that the practice model achieved overall fidelity to the wraparound model, although some subscales indicated a need for increasing natural support, community-based services, and commitment to outcome-based practice (
40). However, all providers in the state were trained by the same technical assistance center, so there was consistency in workforce training to deliver the wraparound practice. Second, regression to the mean (RTM) may explain the changes in the study outcomes. To mitigate RTM effects, a study design and analytic procedures that resemble randomization are highly recommended in the analytic stage for observational studies (
41). In this study, both the natural, quasi-experimental design and inverse probability treatment weighting were used to approximate the randomization process, which minimized bias introduced by the RTM. Finally, the study findings were based on one year of postdischarge data. A longer observation period is needed to study the long-term benefits of this care model.
Conclusions
A care management entity with wraparound services is a promising care delivery model for youths with severe mental or behavioral disorders and may inform state policies and practices. As states implement coordinated care models to serve youths with severe needs for mental health services, additional efforts are needed to assess the comparative effectiveness of these programs for the larger community of youths with special mental health care needs. Among youths who met selection criteria for this study, the mean duration of enrollment in the care management entity was 315±207 days. The most common reason for discharge was successful completion, indicating that the youths’ functioning levels had increased and thus the youths had resumed their use of standard care in the community (
42).
Acknowledgments
The authors acknowledge the data/analytic contribution of Hilltop Institute, University of Maryland, Baltimore County, and support from the Institute for Innovation and Implementation, University of Maryland.