West Virginia faces chronic funding challenges, limited resources, and overwhelming health care disparities that have worsened during the present opioid epidemic and that affect determinants of health. The West Virginia Children’s Access Network (WVCAN), a project sponsored by a grant from the Health Resources and Service Administration (HRSA), is an example of a way to address such disparities for children with mental health needs in schools. This project aimed to provide school-based psychiatry services in West Virginia’s rural areas by child psychiatrists and psychologists trained in telepsychiatry. The Appalachian population is challenged by poverty, provider shortage, and geographical isolation (
1). Because of stigmatization, lack of psychiatric literacy, and adequate access to psychiatric specialists, rural patients’ mental health is exceptionally vulnerable and often relegated to primary care. In these communities, there is insufficient coordination of care with psychiatrists (
2). Most notably, there is a profound treatment gap among the 14% to 20% of children and adolescents who display or verbalize evidence of a psychiatric disorder. Of those identified, 70% never receive treatment (
3).
According to HRSA, West Virginia has 372 health professional shortage areas, 90 of which are mental health specific [see
online supplement] (
4). Access to affordable health care coverage was made available with the Affordable Care Act, in which the number of uninsured West Virginia children decreased by 44%. Roughly 11,000 children remain uninsured and largely without care. An assessment of transportation-related health care barriers in McDowell County revealed that 55% of residents traveled longer than 60 minutes to care, 29% could not drive themselves to care, 42% missed medical appointments because of a lack of transportation, and 70% reported that road conditions prevented transportation to care (
5). Because of this confluence of tremendous need and insufficient capacity, creative solutions are needed to ensure availability of psychiatric services locally.
While evaluating behavioral health needs in Appalachian schools, staff and students identified many areas of need, including diffusing and treating anger, bullying, truancy, family abuse and violence, self-harm, and substance abuse (
6). In 2013 and 2014, approximately 14,000 West Virginia adolescents ages 12 to 17 (11% of all adolescents) had at least one major depressive episode within the past year. Additionally, in each year from 2010 to 2014, 5,000 adolescents ages 12–17 (45% of all adolescents with major depressive episode) received treatment for their depression in the past year (
7). Often, minors do not receive sufficient services to support them in their homes, schools, or communities. Because of this scarcity, children with mental illness are at risk of unnecessary segregation or institutionalization. A letter to the governor from the Department of Justice dated June 1, 2015, states that West Virginia fails to provide services to children with significant mental health conditions in settings appropriate to their needs (
8). Implementation and dissemination of an evidence-based telehealth model for integrating mental health services into school-based clinics are likely solutions.
Implications for School Health
In Appalachia, school-based health clinics (SBHCs) are a key point of access to health care for West Virginia’s youths (
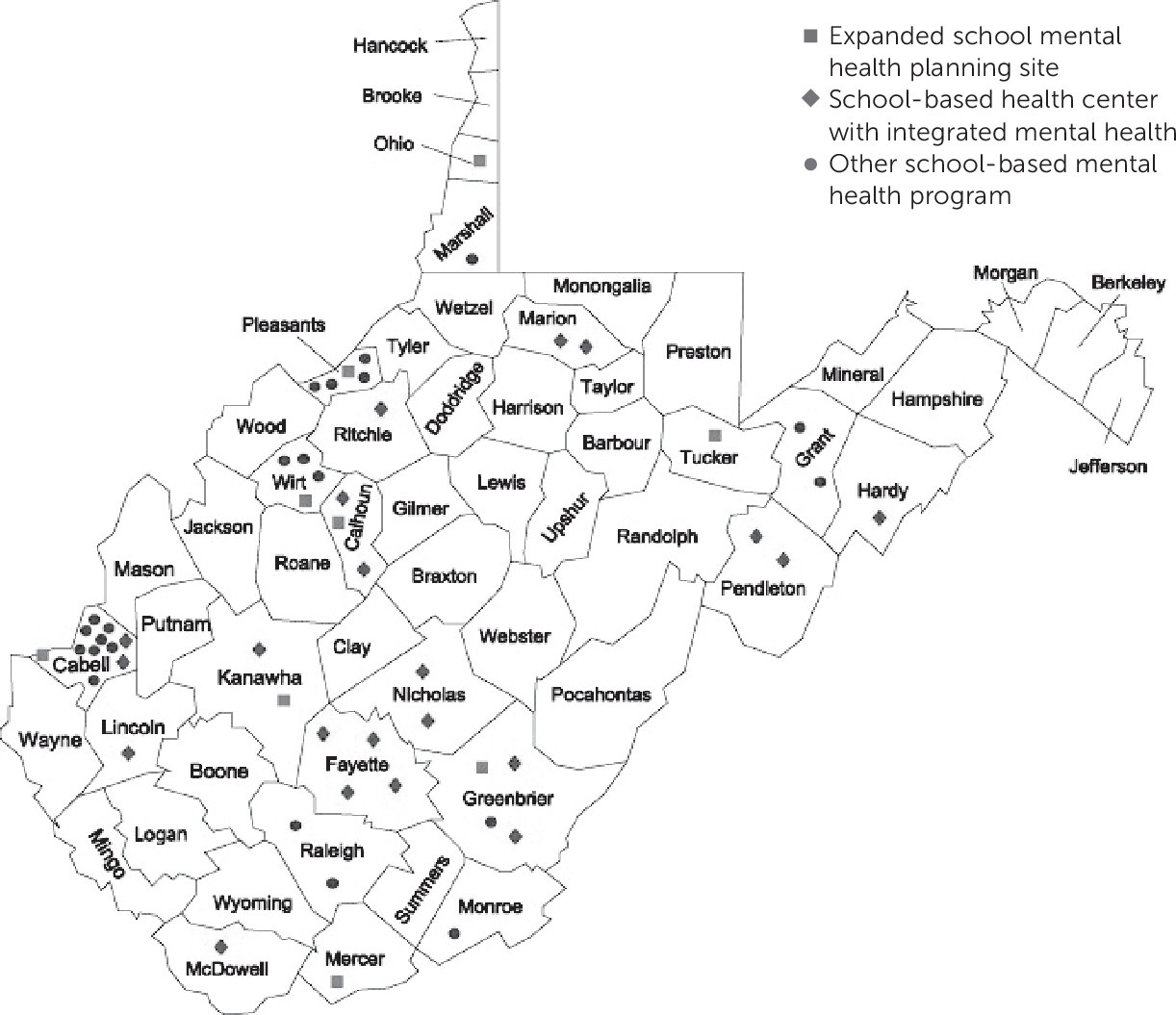
9). SBHCs are health clinic sites sponsored and managed by community health centers. SBHCs are housed within a school site and provide a range of services, such as preventive and immediate care, behavioral health services, health education, and sometimes dental care. Most SBHC services are provided during the school day. West Virginia’s SBHCs have been providing easily accessible and cost-effective care to school-age children for over 18 years. As of fall 2015, school-based health services were available to a school-aged population of over 76,000 children in 36 counties (
Figure 1). West Virginia has the most SBHCs per capita in the United States. SBHCs are well accepted by local communities and have ongoing partnerships with county school systems. The American Academy of Pediatrics supports the use of SBHCs, citing the proven benefits and great potential. West Virginia’s Expanded School Mental Health Initiative is a jointly sponsored effort of the West Virginia Department of Education and the West Virginia Department of Health and Human Resources that aims to build on core services typically provided by schools. Although these initiatives have the potential to identify the problem areas and intervene early, schools are often overwhelmed by the lack of resources to meet their needs.
By using telepsychiatry, SBHCs can become natural collaborators for telehealth access. When mental health services are available in the SBHC, evidence has shown the ability to reduce mental health care disparities (
10). Many practice models are identified in the telehealth service line for mental health treatment, but the model in which psychiatrists provide consultative care to primary care providers has been recommended as the approach with the most robust evidence for improving patient care (
3). Other practice models include direct care, teacher conferences, and education for teachers, school nurses, parents, the student body, and the community at large. These models may be implemented singularly or in combination to provide a holistic, collaborative approach.
Implementation Strategy of WVCAN
The strategy discussed here, which is currently used in the WVCAN project, allows for implementation of a multidisciplinary telehealth model into three SBHCs in West Virginia (Barbour, Pocahontas, and McDowell counties). Our primary outcomes were increasing youth access to psychiatric care and reducing wait times. Secondary outcomes focused on satisfaction and sustainability. We hypothesized that WVCAN would increase access to psychiatric services for youths who were unable to access these services through other means and reduce the wait times for their first appointments. Finally, we expected teachers, parents, and youths to report their impressions of WVCAN services.
Before operationalizing services, the necessary steps to ensure success included identifying sites, assessing clinical and technical needs, identifying funding opportunities, and being aware of state- and payer-dependent telemedicine regulations. Identification of an on-site “champion” was vital to ensure systematized implementation. Frequent on-site visits to train, evaluate, and assist staff occurred initially and decreased as network sites gained competency and efficiency in the screening and referral process. Informational flyers detailing available services were disseminated periodically to local referral sources and the school community to facilitate communication. In an attempt to maximize mental health provider services, all SBHCs opted to combine the use of comanaged direct care and consultation and stabilization models. This included the use of a child and adolescent psychiatrist who assists patients with diagnostic clarity and stabilization followed by a transition back to the SBHC primary provider. Case consultations were offered for acute crises or established patients. The SBHC staff included a case manager (CM) and, at times, a nurse. The HRSA grant supported the telehealth equipment and the services of a part-time child psychiatrist, who spent 4 hours per week at each site. Patient areas at SBHC were carefully selected to maintain appropriate privacy for the clinical encounter. School personnel, therapists, parents, or primary care physicians could refer any enrolled student who had not been able to access outpatient child psychiatric care for any reason to WVCAN.
When CMs identified children in need, they described the program to the parents and then obtained consent for WVCAN to contact them. Obtaining consent for minors to receive mental health services in an SBHC can be challenging because of a lack of guardian availability. However, at the time of the evaluation, the child psychiatrist obtained both assent from the youth while on video and verbal consent from the guardian by telephone. The child psychiatrist conducted a comprehensive diagnostic evaluation of the minor who attended the initial intake via telemedicine. The treatment options were discussed with both the child and the guardian. A follow-up appointment was scheduled within 4 to 6 weeks to determine if progress had been made. For most children, a form of psychotherapy was recommended even when medications were prescribed, and the CMs often made the therapy referrals (with parental consent) and ensured initial contact with the therapist. Psychological services (group therapy via telehealth supervision) were implemented for the student body on topics including anger management, assertiveness, and coping skills. On review of completed appointments at one year (September 2016 to August 2017), the following findings are highlighted. The primary referral sources were largely initiated by the local therapists, CMs, parents, teachers, and school counselors. Lack of access to local specialists and long wait times were cited as the most common referral reasons. A total of 98 appointments were provided, of which 65 were kept, for a no-show rate of 17%. Two hospitalizations were reported among the served youth. The full impact of this project will be discussed when all data are available.
Barriers, Challenges, and Sustainability
The lack of appropriate service reimbursement has been one of the largest challenges in sustaining rural telehealth programs. Despite the evidence base and favorable policy environment, telehealth claims for mental health are a small proportion of total claims, and average reimbursements for these claims are substantially lower than are those for comparable nontelehealth services (
11). Currently, 48 states and the District of Columbia provide Medicaid reimbursement for some forms of interactive telemedicine services; however, the degree of reimbursement varies widely. Specific to West Virginia, live video reimbursement is offered for authorized providers at distant sites; however, no reimbursement is offered for asynchronous evaluations or electronic communications, such as e-mail, phone, or fax interactions. Prescribing medications online is allowable when a “valid patient–practitioner relationship” has been established through telemedicine in a manner approved by the appropriate board (
12). Given the variability between payers, a component of the WVCAN programmatic success has included periodic review of claims submitted by network sites and paid by the project team to ensure consistent reimbursement. Network site involvement in free CME opportunities at the hub site was established via telemedicine to bolster collaboration, support, and sustainability. A novel educational opportunity for group supervision, in which the psychologist supervised an on-site therapist via telehealth, was established.
Maintaining a team that includes multiple personnel working distances from, yet connected with the local community, is important to mitigate cultural and distance barriers. CMs provided ongoing support for WVCAN by making appropriate referrals, connecting providers with families and school personnel, serving as liaisons and advocates for both the youths and the providers, and providing ongoing data about service impact. Finally, it has been imperative to conduct periodic self-assessments to examine strengths and weaknesses of the program as well as to seek out supervision from fellow telehealth and SBHC colleagues.
Discussion
Telehealth is an efficacious and cost-effective model to screen and provide specialty services to children in rural areas while also increasing compliance. First, given that psychiatric care is indicated for many youths with serious emotional and behavior problems, it is imperative for the school community to find ways to partner with psychiatric providers. Telehealth behavioral services are instrumental in addressing the access-to-care limitations of mountainous rural and underserved areas. There is a growing evidence base that such interventions are as effective as in-person evaluation and treatment for a variety of presenting problems and treatment modalities. This model can also elicit more self-initiated and confidential care, employ increased prevention strategies, use adolescent-focused care, and reduce the overall cost of care (
13). WVCAN provides an exemplar of a school–telepsychiatry partnership that brings the services to the setting where youths are most accessible. By virtually eliminating wait time for service, WVCAN directly disrupts the known cycle of underuse of psychiatric care experienced by youths who fall through the cracks as they wait for service.