The rising prevalence of autism spectrum disorder (ASD), which increased from 1 in 150 children in 2004 to 1 in 59 children in 2014, also has increased the use of services to treat ASD (
1,
2). Although patients with mild ASD may rely on treatments that improve social and communicative ability, patients with more severe ASD often require individual support with intensive behavioral interventions and psychotropic medications (
3). For acute episodes with aggressive or self-injurious behaviors, which are common among some children and young adults with ASD, these services may not suffice. As a result, psychiatric hospitalizations occur more frequently among this population—approximately 10% of youths with ASD experience a psychiatric hospitalization before age 21, and the average length of stay is longer for youths with ASD compared with other psychiatric conditions (
4). Although these hospitalizations often are warranted, they remove children and young adults from their homes, disrupt ongoing treatments, and may indicate a failure of home and community-based care (
5,
6).
Similar to psychiatric hospitalizations, emergency department (ED) visits occur more frequently for youths with ASD. One study reported that 30% of children with ASD had at least one ED visit in the prior 12 months compared with 17% of children without ASD (
7), and a second study found a nine-fold increase in the likelihood of a psychiatric ED visit among children with ASD compared with children without ASD (
8). A third study concluded that ED visits among individuals with ASD are increasing over time in some age groups—for example, the share of young adults ages 15 to 21 with ASD experiencing an ED visit increased from <5% to approximately 30% between 2005 and 2013 (
9). These findings are of concern, because ED staff may not have adequate training to provide high-quality care to patients with psychiatric conditions such as ASD; in acute episodes marked by agitation, the lack of training can place both providers and patients at risk (
10,
11).
If psychiatric hospitalizations and ED visits result, at least in part, from inadequate access to home and community-based care, then increasing the utilization of outpatient services for ASD may reduce the likelihood of these events if those services deter the negative symptomatology that can result in hospitalizations. A substitution effect between outpatient and inpatient services has been identified in the treatment of psychiatric disorders in general (
12), psychosis (
13), depression (
14), bipolar disorder (
15), and substance use disorder (
16). Whether a substitution effect exists in the treatment of ASD is less clear. One study using Medicaid claims data found no association between outpatient services and likelihood of psychiatric hospitalizations among children with ASD but found that an increase in spending on respite care reduced the likelihood of an inpatient stay (
17). More recently, another study using commercial claims data reported that outpatient service utilization increased directly before an ED visit among children with ASD (
18). However, the authors focused only on outpatient services used within 30 days of the ED visit and did not control for measures of earlier spending.
To better understand the relationship between psychiatric hospitalizations, ED visits, and home and community-based care in the treatment of ASD, this study used commercial insurance claims data from >100,000 children and young adults with ASD to examine whether the utilization of ASD-specific outpatient services, including occupational, physical, and speech therapies and other behavioral interventions, would reduce the likelihood of psychiatric hospitalizations and ED visits.
Methods
Data Sources and Sample
This retrospective data study was exempted from review by the University of Pennsylvania’s Institutional Review Board. The primary data source was the Health Care Cost Institute, which collects inpatient, outpatient, and pharmacy claims from Aetna, Humana, and UnitedHealth. The study period covered January 1, 2008, through December 31, 2012. The study sample consisted of individuals from birth through age 21 years diagnosed with ASD. For this study, diagnosis of ASD was defined as having at least two claims on different days containing an ICD-9-CM diagnosis code of 299.XX during the study period.
Our sample included data only from children and young adults whose behavioral health claims were included in the data (i.e., the behavioral services were not carved out). Individuals whose claims were in the top 0.1% of the spending distribution were excluded to eliminate a small number of outliers with extreme levels of spending; we did not exclude the bottom 0.1% because the distribution was only skewed toward high spenders. Continuous enrollment in an insurance plan during the entire study period was not required. For patients with multiple periods of enrollment, the earliest period of enrollment was used.
Measures
We had two outcome variables: a binary indicator of a hospitalization in a given week and a binary indicator of an ED visit in a given week. Only hospitalizations and ED visits with an associated psychiatric diagnosis code (ICD-9-CM 290.XX through 319.XX) were included. The explanatory variable of interest was spending on any outpatient services with an associated diagnosis code of 299.XX, which indicated an ASD-specific service. These services included occupational and physical therapies, speech therapy, diagnostic assessment, case management, mental health/social skills/behavior modification, a personal care or home health aide, and family therapy. Spending was calculated as the sum of payments made by the insured (i.e., coinsurance, copayments, and deductibles) and by the insurer.
A primary analytic challenge of this study was to determine how to select the time periods in which to measure service utilization. We hypothesized that ASD-specific outpatient services immediately preceding a psychiatric hospitalization or ED visit may have been related to an acute crisis rather than to the type of services these individuals typically received, and that more distant measures of spending were more likely to capture treatment as usual. Therefore, three measures were constructed for each child: the first consisted of spending in the 2 weeks prior to the week of a psychiatric hospitalization or ED visit, the second measure consisted of spending in the 3 to 6 weeks prior to the week of one of these events, and the third measure consisted of spending in the 7 to 14 weeks prior to the week of one of these events. To create these measures, individuals needed to have had a period of continuous enrollment that was at least 14 weeks long. Similar measures were constructed to assess use of outpatient services without a specific ASD diagnosis, thus enabling us to control for other health care utilization. In all analyses, spending was measured in thousands of dollars.
We controlled for psychotropic medication use with five variables that indicated whether a patient had a prescription filled for an antidepressant, antipsychotic, anxiolytic, mood stabilizer, or stimulant medication during the week prior to the psychiatric hospitalization or ED visit. Both new and refilled prescriptions were included. Psychotropic medications were not collapsed into one category as were outpatient services because of the substantial variation in prices of drugs and drug classes, which made it more difficult to capture use and spending.
Covariates included age at baseline, gender, type of insurance (point of service, preferred provider organization, health maintenance organization, exclusive provider organization, indemnity/other, or high deductible), state fixed effects, and a quadratic weekly time trend.
Statistical Analysis
Survival analyses were used to identify the impact of ASD-specific outpatient service spending over time. Specifically, we estimated maximum-likelihood discrete-time survival models with complementary log-log links, where the events of interest were a hospitalization or an ED visit with an associated psychiatric diagnostic code in a given week. For children and young adults with repeat hospitalizations, only the first hospitalization was used. This approach is similar to that used for discrete logistic regression analyses but allows for the estimation of coefficients to be invariant to the length of the time interval (
19). The unit of analysis was the patient-week. Standard errors were robust. Estimated coefficients were manually converted to hazard ratios (HRs) for interpretation.
Given the number of potential approaches, we performed sensitivity analyses using alternative spending measures as well as other statistical models, including Cox regression analyses. We also performed additional analyses to determine whether the effect of spending on ASD-specific outpatient services differed for youths who had higher levels of spending and whether the effect changed when we controlled for the consistency over time of services received.
Results
The final sample included 104,381 children and young adults with ASD across all 50 states. Approximately 9% of the study sample had at least one psychiatric hospitalization between 2008 and 2012; there was a higher incidence of ED visits, with 14% of the study sample experiencing at least one ED visit with an associated psychiatric code (
Table 1). The mean±SD age at baseline was 8.5±4.6, and the sample was more than 80% male. The most common insurance type was point of service (64.9%), followed by preferred provider organizations (13.9%), health maintenance organizations (13.6%), and exclusive provider organizations (7.3%); only 12% of the children were enrolled in a high-deductible health plan. On average, weekly spending on ASD-specific outpatient services was $36 compared with $53 for non-ASD outpatient services.
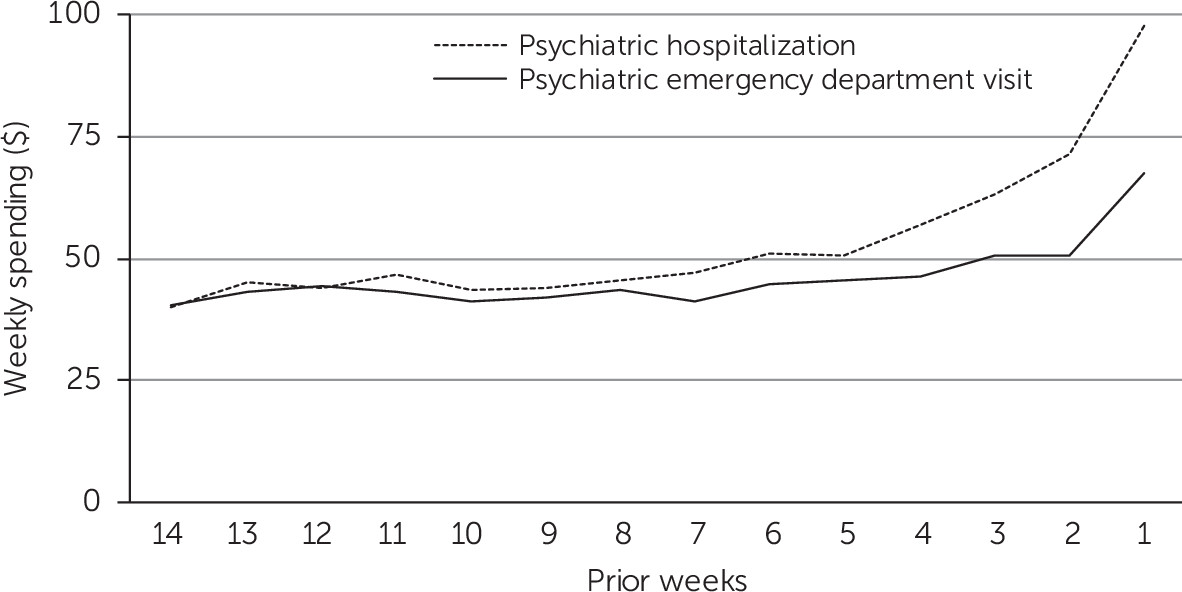
First, we plotted the trajectory of average weekly spending on ASD-specific outpatient services leading up to a psychiatric hospitalization or ED visit among all children and young adults who experienced either event to determine the appropriate construction of spending measures. Spending was relatively constant until 5 to 6 weeks before an event, when it increased moderately and then spiked during the 2 weeks prior to the event (
Figure 1).
Next, we performed complementary log-log regression analyses and found a positive association between the likelihood of psychiatric hospitalizations and greater spending on ASD-specific outpatient services in the 2 weeks prior (HR=1.12; p<0.001) to the hospitalization, as well as in the 3 to 6 weeks prior (HR=1.06; p<0.001) to the hospitalization (
Table 2). Conversely, greater spending on ASD-specific outpatient services in the 7 to 14 weeks prior to the psychiatric hospitalization was associated with a lower incidence of psychiatric hospitalization (HR=0.98; p=0.011).
As with psychiatric hospitalizations, greater spending on ASD-specific outpatient services in the 2 weeks prior (HR=1.08; p<0.001) and 3–6 weeks prior (HR=1.03; p=0.033) to a psychiatric ED visit was positively associated with the likelihood of the event, but there was no association between the likelihood of a psychiatric ED visit and spending on ASD-specific outpatient services in the 7 to 14 weeks prior (HR=1.00; p=0.631) to the ED visit.
Greater non–ASD-specific spending in all time periods was positively associated with both psychiatric hospitalizations and ED visits. With the exception of stimulants, having a prescription for a psychotropic medication was positively associated with incidence of both kinds of events.
In our analyses of the monthly spending measures for each patient, findings were qualitatively similar (see Appendix A in the online supplement). Results were robust as analyzed with other statistical approaches as well, including Cox regression analyses (see Appendix B in the online supplement). We also performed subanalyses based on quintiles of average spending in the 7- to 14-week period, which is the measure most likely to capture treatment as usual (see Appendix C in the online supplement). In the highest-spending quintile, the 7- to 14-week measure had a larger impact on the likelihood of psychiatric hospitalizations compared with the full sample (HR=0.95; p<0.001). In the lowest-spending quintile, spending in the 7–14 weeks prior to an event had an even larger effect (HR=0.08; p=0.008). Notably, there was a negative and significant effect of spending during the 7 to 14 weeks prior to an event on ED visits in the highest-spending quintile (HR=0.95; p<0.001). Finally, we examined the consistency of the home and community-based care children received (see Appendix D in the online supplement). While it is difficult to measure consistency in claims, we created a binary variable that indicated whether the patient received ASD-specific outpatient services in each of the 7 to 14 weeks prior to the psychiatric hospitalization or ED visit. The consistency variable was negatively associated with psychiatric hospitalizations (HR=0.70, p=0.007) but not with ED visits (HR=1.01, p=0.830).
Discussion
The utilization of home and community-based care may lower the risk of psychiatric hospitalizations and ED visits for children and young adults with ASD, but there has been little evidence to support this hypothesis. In part, this is because most studies focus on more proximate service utilization (e.g., 30 days surrounding an event) and therefore do not allow for differential effects of less recent utilization. Our study addressed this gap by constructing spending measures for periods closer to and further from a given psychiatric hospitalization or ED visit.
Results showed that less recent spending on ASD-specific outpatient services—specifically, spending during the 7 to 14 weeks prior to an event in a given week—reduced the likelihood of a psychiatric hospitalization in that week. Spending on service utilization in the weeks closer to the psychiatric hospitalization did not decrease the risk, which suggests that these services were associated with increased symptomatology and therefore were delivered too late to prevent the hospitalization. On average, there was no evidence that spending on ASD-specific outpatient services reduced the likelihood of a psychiatric ED visit.
These results highlight a potential benefit of home and community-based care, especially when those services are not contingent on the manifestation of aggressive or self-injurious behaviors that may lead to psychiatric hospitalizations. The observed effect was small—each additional $1,000 in spending during the 8-week period ($125 per week during the 7–14 weeks before an event) was associated with a 2% reduction in the risk of a psychiatric hospitalization. For comparison, that is more than twice the average conditional spending on ASD-specific outpatient services over an 8-week period ($881, SD: $2,179). However, it is far less than the average conditional spending on psychiatric hospitalizations in a single week ($4,323, SD: $4,066).
While the effect is modest, the main finding may be attenuated because there was no available measure of patients’ clinical or functional severity in the data. Estimating any inverse association between spending on outpatient services and psychiatric hospitalizations without this information illustrates the robustness of this result. One might expect these findings to differ based on severity of illness or prior utilization of services, a result which our sensitivity analyses suggest. One might also expect these findings to differ based on the consistency of services received; in other sensitivity analyses, we found a larger protective effect when services were delivered every week. These additional results suggest that there are different mechanisms through which ASD-specific outpatient services can decrease the risk of psychiatric hospitalizations for children and young adults with ASD.
Our findings diverge from previous work by Mandell and colleagues (
17), who found that respite care, but not outpatient care, reduced the likelihood of psychiatric hospitalizations for children with ASD. No information on respite care was available for the present study, and this kind of care is rarely covered by commercial insurance (
20). The difference in results could stem, at least in part, from higher reimbursement rates and a wider network of providers in commercial insurance than in Medicaid, which may translate into commercially insured patients accessing care more easily than patients with Medicaid (
21,
22). The results also could be driven by differences in quality, but little research has directly compared the quality of services delivered to individuals with ASD across different types of insurance.
Even if these services reduce the likelihood of adverse events, it may be difficult for some individuals with ASD to access home and community-based care—more than half of caregivers have reported difficulty accessing services, with one in five lacking a usual source of care (
23). One reason for this difficulty is a shortage of trained providers (
24), some of whom have raised concerns about the lack of training opportunities in evidence-based practices to treat patients who have ASD (
25). Addressing these barriers could improve the overall value of health care by reducing the use of costlier and more restrictive services, such as psychiatric hospitalizations. Other hurdles that families face, such as uncertainty about which treatments are covered by insurance, may mean that only those families that can effectively navigate health care delivery are able to utilize consistent, high-quality home and community-based care for ASD (
26).
Several limitations of this study should be noted. First, ASD diagnoses were not verified through clinical review, although the approach we used (i.e., determining a diagnosis on the basis of two ASD claims on separate days) has been shown to have high positive predictive value (
27). Second, we do not have any information on school-based or other services not paid for by insurance and thus may have underestimated the amount of care a child received, which would have biased our findings if children and young adults with ASD experiencing psychiatric hospitalizations or ED visits used these services at a different rate than those not experiencing such events. Third, we did not control for the quality of care, which can have an impact on the effectiveness of the services utilized. Fourth, spending measures were selected based on the trajectories of ASD-specific outpatient spending as demonstrated in
Figure 1, but they may not be the most appropriate measures of service utilization. Fifth, our measures of psychotropic prescription drugs filled only covered the week prior to a psychiatric hospitalization or ED visit and cannot be used to distinguish acute versus chronic medication use.
Finally, our results have not demonstrated that a $1,000 increase in spending on ASD-specific outpatient services during the course of 8 weeks is necessary for every child with ASD—instead, they suggest that more utilization of home and community-based care can confer protective benefits to children and young adults with ASD who are at risk of hospitalization. Of note, other benefits associated with reduced risk of psychiatric hospitalization via increased outpatient service utilization were not included in our analyses.
Conclusions
Despite these limitations, our findings have important implications. The financial burden associated with ASD is extensive, and psychiatric hospitalizations remain the most expensive type of service for youths with ASD (
28,
29). Policies such as ASD insurance mandates and mental health parity laws may increase spending on outpatient services by insurers initially (
30,
31), but our results suggest that some of the financial burden could be reduced in the long term, because children with ASD who received more home and community-based care had a lower risk of experiencing psychiatric hospitalizations. A better understanding of the mechanisms by which psychiatric hospitalizations occur in children and young adults with ASD may further reduce the likelihood of these adverse events.