Factors Associated With Receipt of Cognitive-Behavioral Therapy or Prolonged Exposure Therapy Among Individuals With PTSD
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Methods
Procedure
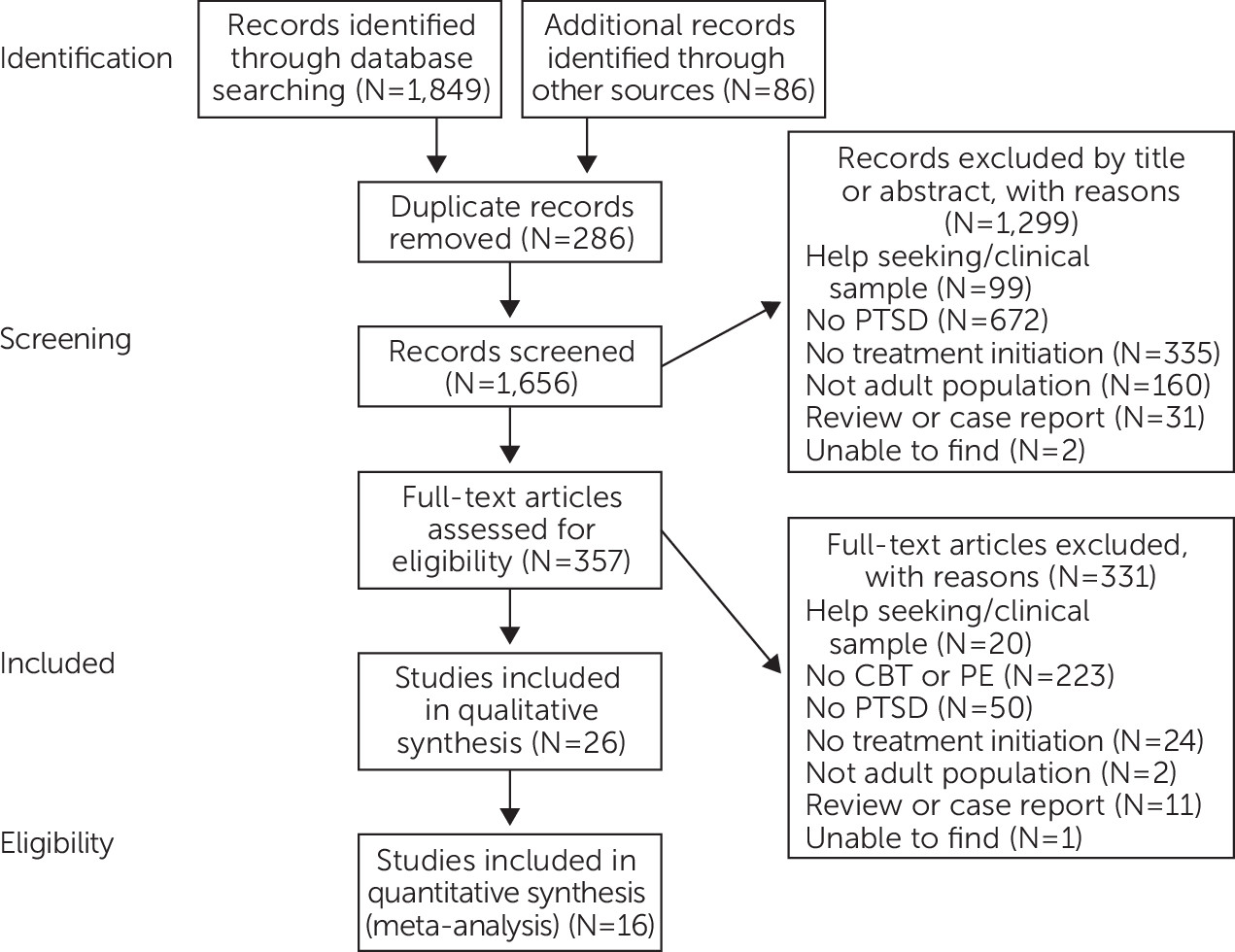
Data Analysis
Results
Quality of Studies
Participants
| Study | N | Sample | Dates | Design | Treatment | Outcomes |
|---|---|---|---|---|---|---|
| Baker et al., 2015 (23) | 156 | Veterans with PTSD | 2008–2012 | Retrospective chart review | PE, CBT | Initiation, completion of PE and CBT |
| Chen et al., 2013 (44) | 200 | Treatment-seeking civilians with chronic PTSD | 2012–2013 | Cross-sectional survey | PE | Preference for PE versus SSRIs |
| DeViva et al., 2017 (24) | 182 | Veterans with PTSD | 2012–2015 | RCT, retrospective chart review | CPT, PE | Initiation, education group |
| Feeny et al., 2009 (45) | 74 | Women recruited through ads for PTSD treatment | 2008–2009 | Cross-sectional survey | PE | Preference for SSRIs versus PE |
| Grubbs et al., 2015 (25) | 133 | Rural veterans with PTSD | 2013–2015 | Retrospective chart review | CPT | Initiation, engagement with CPT |
| Harned et al., 2013 (46) | 46 | Women with PTSD and BPD | 2012–2013 | Cross-sectional survey | PE | Preference for DBT or DBT + PE |
| Hundt et al., 2018 (26) | 201 | Veterans with PTSD | 2015–2016 | Retrospective chart review | PE, CPT | Initiation with PE/CPT |
| Hundt et al., 2018 (27) | 24 | Veterans with PTSD who declined PE and CPT | 2015–2016 | Qualitative | PE, CPT | Initiation with PE/CPT |
| Iversen et al., 2010 (43) | 821 | U.K. Iraq war military | 2003 | Cross-sectional survey | CBT, medications | Initiation, engagement with CBT, medications |
| Kehle-Forbes et al., 2014 (42) | 58 | National Guard veterans | 2013 | Qualitative | PE, SSRIs | Preference for PE versus SSRIs |
| Kehle-Forbes et al., 2016 (28) | 427 | Veterans with PTSD | 2010–2012 | Retrospective chart review | CPT, PE | Initiated PE and CPT, dropped out of PE and CPT |
| Keller & Tuerk, 2016 (29) | 324 | Veterans with PTSD | 2015 | Cross-sectional survey | PE, CBT | PE and CBT noninitiation |
| Lamp et al., 2014 (30) | 476 | Veterans with PTSD | 2013 | Retrospective chart review | PE, CPT | PE and CPT interest and initiation |
| Lu et al., 2016 (31) | 63 | Veterans with PTSD | 2008 | Content analysis | PE, CBT | Receipt of PE and CBT |
| Maguen et al., 2018 (32) | 2,960 | Veterans with PTSD | 2001–2015 | Retrospective chart review, content analysis | PE, CPT | Receipt of PE and CPT, N of sessions |
| Mott et al., 2014 (33) | 796 | Veterans with PTSD | 2008–2012 | Retrospective chart review, content analysis | PE, CBT | Initiation and completion of PE and CBT |
| Rosen et al., 2017 (34) | 61,128 | Veteran patients of clinicians trained in PE | 2015–2016 | Longitudinal survey | PE | Reach and maintenance of PE |
| Shalev et al., 2012 (47) | 397 | ER trauma patients in Jerusalem | 2003–2007 | Cross-sectional survey | CBT, PE | Initiation, preference for PE versus SSRIs |
| Shiner et al., 2013 (35) | 1,924 | Veterans with PTSD | 2009–2010 | Retrospective chart review, content analysis | PE, CBT | Use of PE and CBT |
| Shiner et al., 2018 (36) | 13,473 | Veterans with PTSD | 2014–2016 | Retrospective chart review | PE, CPT | Use of EBP templates |
| Sripada et al., 2018 (37) | 270,277 | Veterans with PTSD | 2015–2016 | Retrospective chart review | PE, CPT | Use of EBP templates |
| Sripada et al., 2018 (38) | 273,694 | Veterans with PTSD | 2015–2016 | Retrospective chart review | PE, CPT | Use of EBP templates |
| Stecker et al., 2013 (41) | 143 | Veterans with PTSD | 2009–2012 | Cross-sectional, qualitative | CBT | CBT noninitiation |
| Tuerk et al., 2013 (39) | 60 | Veterans with PTSD | 2007–2009 | Retrospective chart review | PE | Completed minimum PE sessions |
| Watts et al., 2014 (40) | 1,924 | Veterans with PTSD | 2009–2010 | Retrospective chart review | PE, CBT | N of veterans who received PE and CBT |
| Zayfert et al., 2005 (48) | 115 | Civilian patients of an anxiety clinic | 2002–2004 | Cohort, longitudinal | CBT | Initiation and completion of CBT |
Initiation of TC-CBT Treatments
| Participants | |||||
|---|---|---|---|---|---|
| Study | Setting | Male (%) | Average age | Diagnosis of PTSD (%) | Utilization of TC-CBT (%) |
| Baker et al., 2015 (23) | VA PTSD clinic | 90.4 | 46.7 | 100.0 | 58.0 |
| Chen et al., 2013 (44) | PTSD treatment study | 25.0 | 37.4 | 100.0 | 61.0 |
| Deviva et al., 2017 (24) | VA PTSD clinic | 93.0 | 48.5 | 100.0 | 34.0 |
| Feeny et al., 2009 (45) | Convenience | 0 | 31.8 | 100.0 | 82.0 |
| Grubbs et al., 2015 (25) | VA clinic | 88.7 | 51.9 | 100.0 | 55.0 |
| Harned et al., 2013 (46) | behavioral therapy clinic | 0 | 34.0 | 100.0 | 67.0 |
| Hundt et al., 2018 (26) | VA PTSD clinic | 79.3 | 43.7 | 100.0 | 42.0 |
| Hundt et al., 2018 (27)a | VA PTSD clinic | 79.0 | 44.6 | 100.0 | 0 |
| Iverson et al., 2010 (43) | VHA | 90.0 | 34.0 | 79.7 | 7.3 |
| Kehle-Forbes et al., 2014 (42) | Military | 98.3 | 35.4 | 100.0 | 53.0 |
| Kehle-Forbes et al., 2016 (28) | VA PTSD clinic | 84.1 | 46.4 | 100.0 | 82.0 |
| Keller and Tuerk, 2016 (29) | VA PTSD clinic | 77.0 | 42.9 | 100.0 | 43.2 |
| Lamp et al., 2014 (30) | VA PTSD clinic | 93.9 | 48.6 | 100.0 | 43.7 |
| Lu et al., 2016 (31) | VA PTSD clinic | 89.0 | 35.3 | 100.0 | 13.0 |
| Maguen et al, 2018 (32) | VHA | 90.0 | 35.5 | 100.0 | 20.1 |
| Mott et al., 2014 (33) | VA PTSD clinic | 90.0 | 46.6 | 87.9 | 11.0 |
| Rosen et al., 2017 (34) | VHA clinicians | 12.0 | |||
| Shalev et al., 2012 (47) | ER in Jerusalem | 54.0 | 38.0 | 100.0 | 72.0 |
| Shiner et al., 2013 (35) | VHA | 93.0 | 53.0 | 100.0 | 6.0 |
| Shiner et al, 2018 (36) | VHA | 88.8 | 100.0 | 28.0 | |
| Sripada et al., 2018 (37) | VHA | 87.0 | 100.0 | 4.0 | |
| Sripada et al., 2018 (38) | VHA | 87.0 | 100.0 | 4.0 | |
| Stecker et al., 2013 (41)a | VHA | 84.0 | 28.0 | 100.0 | 0 |
| Tuerk et al., 2013 (39)a | VA PTSD clinic | 95.0 | 41.4 | 100.0 | 100.0 |
| Watts et al., 2014 (40) | VA PTSD clinic | 93.0 | 53.0 | 100.0 | 6.0 |
| Zayfert et al., 2005 (48) | Anxiety clinic | 18.0 | 37.8 | 100.0 | 83.0 |
Predisposing, Enabling, and Need Variables Related to Initiation of TC-CBT
| Factor | Qualitative themesa | Quantitative variablesb |
|---|---|---|
| Predisposing | ||
| Demographic characteristics | None | Age (N=5), race (N=2), marital status (N=1), military era (N=2), gender (N=2) |
| Mental health beliefs | Concerns about stigma (N=2), denial that treatment is necessary (N=2), readiness (N=2), trust and alliance with therapist (N=3), fear of repercussions related to military career (N=1), preference for psychopharmacology approaches (N=1), interest in trauma-centered therapies (N=2), credibility of treatment and perceived efficacy (N=1), emotional intensity of treatment (N=2), perceived side effects (N=2), timing of symptom relief (N=1), perception of VA (N=1) | Prior group psychotherapy (N=1), interest in trauma-centered therapies (N=1) |
| Enabling | ||
| Logistic issues | Time (N=4), affordability (N=2), distance (N=2), poor therapeutic relationship (N=2), redeployment and contracts (N=1) | Affordability (N=1), PTSD service connection (N=3) |
| Provider Organizational structure and resources | Training of providers (N=1), timing of discussion of treatment options with providers (N=2), consistency of providers (N=1), concerns about privacy (N=3), negative experiences with VA (N=1) | Clinical exposure to prolonged exposure (PE) and cognitive-behavioral therapy (CBT) (N=2), referral source (N=2), access to PE and CBT champions (N=1), provider training (N=2), clinician believes PE effective, workflow for patients with PTSD (N=2), region (N=1), gender of clinician (N=1), race of clinician (N=1) |
| Need | Clinical priorities (i.e., suicidality, substance dependence) (N=1), crisis (N=1), remission (N=1) | PTSD severity (N=3), comorbid depression (N=3), delay in treatment (N=2), length of stay (N=1) |
| Factor | Total N | Studies (N) | Average OR | 95% CI | Weighted OR | 95% CI |
|---|---|---|---|---|---|---|
| Predisposing | ||||||
| Demographic characteristic | ||||||
| Age | 645,407 | 9 | 1.67 | 1.08 to 2.90 | 1.56 | 1.51 to 1.61 |
| Vietnam era (reference: other military era) | 964 | 3 | 1.48 | .75 to 3.21 | 1.58 | 1.00 to 2.15 |
| Female gender (reference: male) | 288,848 | 8 | 1.13 | .61 to 2.49 | 1.18 | 1.08 to 1.27 |
| Black or other race-ethnicity (reference: white) | 288,470 | 9 | 1.38 | .47 to 12.65 | 1.16 | 1.03 to 1.28 |
| Married (reference: unmarried) | 496 | 4 | 1.22 | .62 to 2.82 | 1.44 | .87 to 2.00 |
| Income | 116 | 2 | 1.78 | .37 to 9.08 | 1.52 | −1.19 to 4.89 |
| High school diploma or higher (no high school diploma) | 406 | 4 | .86 | .32 to 3.07 | .99 | .32 to 1.66 |
| Mental health beliefb | ||||||
| Concerns about stigma | 58 | 1 | 8.18 | .95 to 70.44 | 8.18 | .95 to 70.44 |
| Readiness for treatment (reference: ambivalence) | 58 | 1 | .32 | .03 to 3.74 | .32 | .03 to 3.74 |
| Side effects | 58 | 1 | .14 | .02 to 1.37 | .14 | .02 to 1.37 |
| Preference for medication | 58 | 1 | .06 | .01 to .23 | .06 | .01 to .23 |
| Previous psychotherapy | 274,206 | 5 | 1.67 | .90 to 3.47 | 1.01 | 1.01 to 1.02 |
| Trauma-centered interest | 476 | 1 | 2.13 | 1.37 to 3.30 | 2.13 | 1.37 to 3.30 |
| Enabling | ||||||
| Motivators | ||||||
| Disability claim (reference: none) | 133 | 1 | 2.01 | .38 to 10.65 | 2.01 | .38 to 10.65 |
| Logistic issues | ||||||
| Time | 58 | 1 | 3.12 | .94 to 10.36 | 3.12 | .94 to 10.36 |
| Relocation | 58 | 1 | 1.38 | .12 to 16.26 | 1.38 | .12 to 16.26 |
| Affordability | 58 | 1 | 2.96 | .31 to 28.57 | 2.96 | .31 to 28.57 |
| VA service connection (reference: no service connection) | 631,067 | 3 | 1.89 | 1.31 to 3.22 | 2.30 | 2.18 to 2.42 |
| Organizational structure | ||||||
| Mental health referral source (reference: primary care) | 61,452 | 2 | 2.09 | 1.22 to 3.86 | 2.28 | 1.05 to 3.50 |
| Staff training | 76,849 | 4 | 1.29 | 1.02 to 1.72 | 1.19 | .64 to 1.70 |
| Staff exposure | 693,796 | 3 | 2.70 | 2.15 to 3.83 | 2.30 | 2.09 to 2.52 |
| Adaptability of TC-CBT to workflow | 63,052 | 2 | 3.13 | 1.78 to 5.56 | 4.66 | 1.60 to 7.72 |
| Need | ||||||
| PTSD severity | 1,890 | 8 | 1.51 | 1.02 to 2.47 | 1.46 | 1.13 to 1.78 |
| Amount of time treatment delayed | 274,490 | 2 | 1.67 | 1.13 to 2.63 | .93 | .92 to .95 |
| Comorbid depression (reference: none) | 288,486 | 9 | 1.62 | .91 to 3.53 | 1.21 | 1.14 to 1.29 |
| Comorbid substance misuse (reference: none) | 287,562 | 5 | 1.64 | .93 to 3.37 | 1.01 | .96 to 1.07 |
Predisposing characteristics.
Enabling resources.
Need factors.
Findings From Subgroups of High-Quality Studies
Heterogeneity of Predictors
Discussion and Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 92.75 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).