In 2018, the World Health Organization highlighted that the burden of mental illness continues to grow. This not only has a significant impact on health but also has major social, human rights, and economic consequences for countries all over the world. Serious mental illness is defined as “a diagnosable mental, behavioral, or emotional disorder . . . that has resulted in severe functional impairment” (
1). It includes schizophrenia, bipolar disorder, and borderline personality disorder, as well as major depression and anxiety disorders that cause severe and persistent functional impairment. Autism spectrum disorder (ASD) is also associated with persistent and significant social and communication impairments (
2,
3).
Access to a comprehensive standardized evaluation, leading to personalized recovery-oriented care and to psychosocial rehabilitation interventions, remains extremely limited for individuals with schizophrenia and is almost nonexistent for those with borderline personality disorder or ASD (
4). In France, a national network of rehabilitation centers was set up under the French decree on the territory national mental health plan for recovery-focused care. Individuals who have serious mental illness or ASD (disorders that present similar difficulties and rehabilitation needs) and who are engaged in ongoing treatment delivered in public or private mental health establishments are referred by their psychiatrists to third-line rehabilitation centers for complementary, customized evaluations and care. The REHABase database project is a result of this national network.
Psychiatric rehabilitation helps people with serious mental illness to “be successful and satisfied in the living, working, learning, and social environments of their choice” (
5) by designing customized, recovery-oriented rehabilitation plans based on their perceived difficulties, resources, needs for care, objectives, and preferred and valued roles. Evaluations in psychiatric rehabilitation are used to design individualized recovery-oriented intervention plans, and to assess their effectiveness on clinical and functional outcomes. However, rather than being regarded as as therapeutic outcomes, these components are generally used to describe a population; for example, investigators often examine the predictors of subjective quality of life (
6) or job satisfaction (
7) or participants’ perception of the suitability of services received in relation to their care needs (
8).
Rehabilitation brings together a wide range of recovery-oriented interventions. They include strengths-based case management, improvements in physical and mental health and well-being, low-dose psychotropic medication, cognitive remediation, cognitive-behavioral therapy, psychoeducation, social skills training, stigma reduction, family support, supported housing, and supported employment (
5,
9,
10). Combining interventions is the key to effective therapy. For instance, case management is more effective when combined with other therapies (
11,
12). Psychosocial rehabilitation has demonstrated significant positive effects on hospitalization rates (
13), symptoms, and social aspects of schizophrenia (
14,
15). It has also shown effectiveness in the treatment of bipolar disorder (
16), borderline personality disorder (
17), and ASD (
18). Today, although these interventions figure in international guidelines, they are not widely used in routine clinical practice, and not all patients have access to a comprehensive evaluation. Psychosocial impairments are still underdetected and underestimated, and thus they remain untreated, leading to poorer functional outcomes and quality of life.
Quantitative research on recovery among individuals with serious mental illness has been conducted from a clinical perspective (i.e., focusing more on clinical and functional outcomes than on empowerment, autonomy, and agency, which are key to personal recovery) (
19). Recovery rates remain low to moderate, depending on the definition of clinical recovery. For example, Salzer et al. (
20), who defined recovery as absence of substantial interference or limitation in major life activities in the past 12 months, found a rate of approximately one-third among 2,401 participants with a lifetime serious mental illness. In a review and meta-analysis, Jääskeläinen et al. (
21), who defined recovery as clinical remission and social recovery for at least 2 years, found a rate of 13.5% in a sample of persons with schizophrenia.
Subjective recovery does not perfectly fit the medical definition of recovery. Therefore, it depends on a person’s life goals (
22). Supporting personal recovery (defined as “a deeply personal, unique process of changing one’s attitudes, values, feelings, goals, skills and/or roles . . . a way of living a satisfying, hopeful and contributing life even with the limitations caused by illness” [
23]) is therefore one of the major objectives of psychiatric rehabilitation (
5). Andresen and colleagues (
24) defined five stages of recovery on which they later based the STORI (STage Of Recovery Instrument), which is part of the REHABase assessment. The first stage is the moratorium, during which the person is overwhelmed by his or her disability. The second stage is awareness, when hope returns. The person starts developing skills during the third stage, preparation. Then comes rebuilding, where recovery truly starts, with steps forward and steps back, and finally growth, which is considered as the end goal of recovery. Individuals now have faith in their abilities and can handle any setbacks. Of interest, all these stages were found to correlate with other scales that evaluate hope or with recovery-based scales that use other theoretical models. However, the authors suggested that the five stages might overlap, because only three consistent clusters were found in a cluster analysis. This lack of specificity might also be explained by the nonlinear aspect of the recovery process.
The rehabilitation centers in France offer personalized cognitive remediation, psychoeducation, and cognitive-behavioral therapy to help participants implement their life plans according to their strengths and weaknesses (
25) for a limited duration (2–3 years of follow-up). The centers aim to help participants develop strategies they can use on their own. Service users also have representative committees and participate in writing presentation documents. In this article, we present initial data on the clinical profiles, requests, and recovery stages of persons with serious mental illness or ASD participating in the REHABase project. We hypothesized that participants’ requests for help would differ according to their recovery stage.
Methods
The REHABase project is an observational, prospective, and multicenter cohort study launched in 2016 for a planned minimum duration of 15 years. REHABase is supported by the French Regional Health Agencies of Auvergne-Rhône-Alpes and Nouvelle-Aquitaine. Since 2016, five support–psychosocial rehabilitation centers have contributed to the data collection: Lyon, Grenoble, and Saint-Etienne since January 2016 and Bordeaux and Limoges/Poitiers since December 2017. The centers selected to participate in the REHABase network were previously involved in psychosocial rehabilitation and recovery-oriented care. Regular group meetings were held to select the instruments used for the clinical and neuropsychological evaluations, monitor quality control, and ensure good interrater reliability.
Before inclusion in systematic data collection, participants are first given a diagnosis with the specific clinical interview from
DSM-5 (
26). Those with ASD have a documented diagnosis through the Adult Asperger Assessment (
27) or Autism Diagnostic Interview (
28) and Autism Diagnosis and Observation Schedule (
29). Second, their eligibility for inclusion in REHABase is confirmed based on their Global Assessment of Functioning (GAF) score (<61, which was defined as the cutoff for social recovery in the Jääskeläinen et al. [
21] meta-analysis in 2013). Exclusion criteria are minimal, and all participants who meet the diagnosis criteria for severe mental illness or have ASD without intellectual disability and a GAF score of <61 can benefit from the standardized evaluation. The evaluation may, however, be postponed until partial remission for those referred during a psychotic or manic relapse. An information sheet is given to participants to inform them about data confidentiality and their right to withdraw at any time.
The study obtained all of the authorizations required under French legislation (French National Advisory Committee for the Treatment of Information in Health Research, 16.060bis), including information processing (French National Computing and Freedom Committee, DR-2017-268).
Participant data are anonymized before being transferred to the database. Clinical data are collected by using an electronic case report form specifically developed on the Web-based OpenClinica open-source software. The database is securely accessed via ordinary Web browsers.
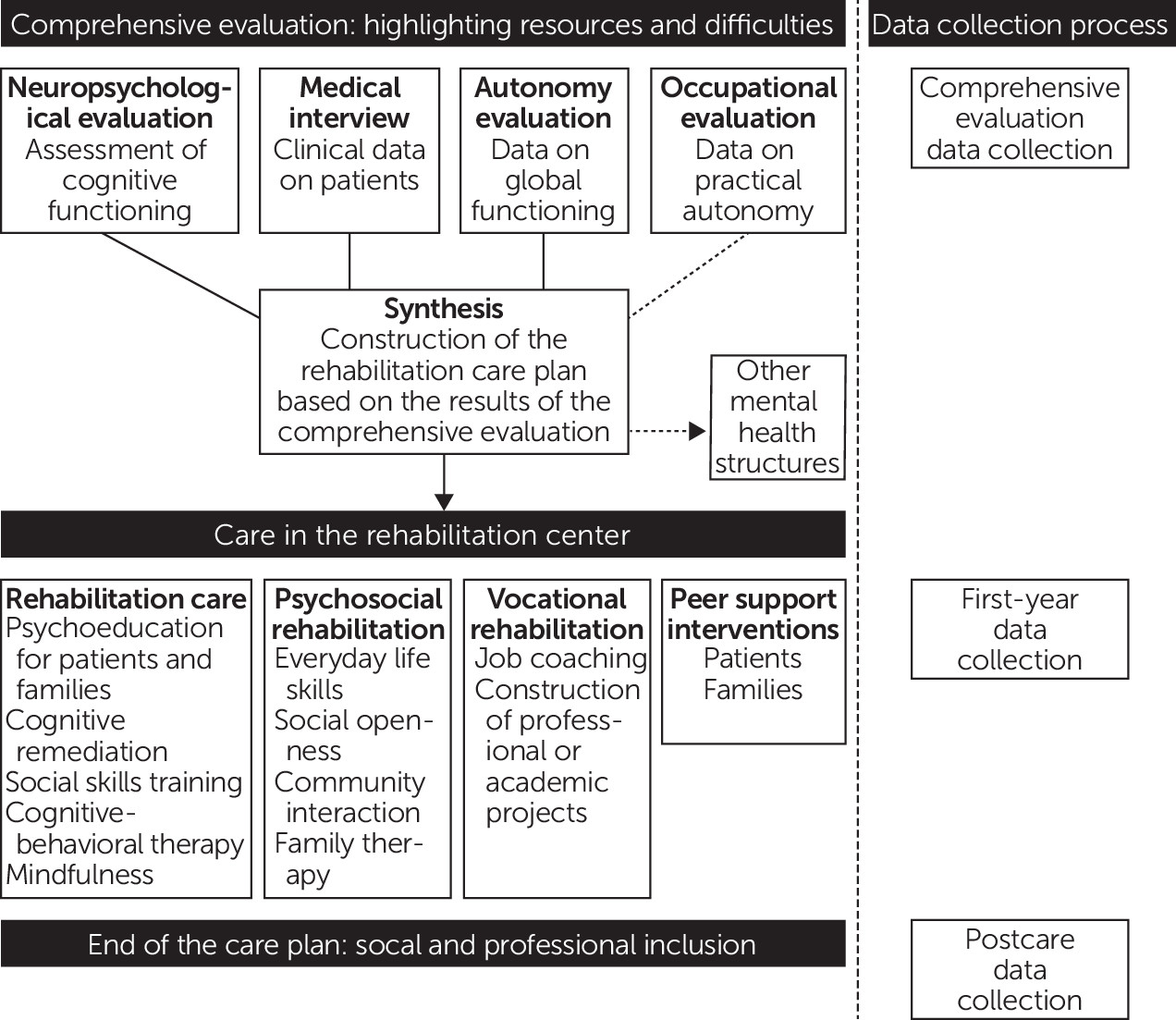
Anyone with serious mental illness or ASD can use the rehabilitation centers. The participants are frequently referred by public mental health services or private psychiatrists. They first undergo a medical interview for registration and diagnosis confirmation. This interview is followed by an initial assessment, including a cognitive and functional evaluation to highlight the individual’s strengths and weaknesses, autonomy, and occupational level. Next, the clinician and participant jointly select relevant therapeutic tools and define personalized rehabilitation care plans. Follow-up is planned to last 2 to 3 years. Evaluations are scheduled at baseline, annually, and after the end of the action plan (
Figure 1).
These first results from the REHABase study provided information on the general characteristics of service users, their level of well-being, their needs for care and psychosocial interventions, the recovery path of the participants with serious mental illness, and their level of dissatisfaction according to their recovery stage. The results focused on data extracted from the satisfaction scale adapted from the Client Assessment of Strengths, Interests and Goals (CASIG) and on recovery stages extracted from the STORI. CASIG was developed by the University of California, Los Angeles (
30). The satisfaction scale includes a structured interview and visual analog scales that consider nine life dimensions. STORI is a 50-item self-report measure developed by the University of Wollongong in Australia (
24) that is used to assess progress in the recovery process. Mental well-being was evaluated with the 14-item autoevaluation Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). For this first presentation of project data, only descriptive analyses were carried out. Descriptive statistics (mean, median, and standard deviation for quantitative data and frequency distribution for qualitative data) were calculated to summarize the baseline characteristics for each variable.
Results
Between January 2016 and August 2018, a total of 1,397 participants were enrolled in REHABase (
Table 1 and
Table 2). Additional information about sociodemographic, general medical, psychosocial, addictions, and neuropsychological data collected is presented in
Table 1 (see also online supplement). Participants were treated with antipsychotics (N=884, 63%), antidepressants (N=426, 30%), anxiolytics (N=370, 26%), and mood stabilizers (N=154, 11%).
Participants’ WEMWBS mean score showed altered mental well-being (mean=42.3; median=42; interquartile range=16–70, compared with a mean score of 51 in a sample from the working general population and 52 in a sample of students [
31]). Possible scores on the instrument range from 5 to 70, with higher scores indicating good well-being. The WEMWBS scores indicated that 36% (N=131) of participants had low well-being (score in the 4th percentile or lower), 29% (N=105) had mildly low well-being (score between the 5th and 25th percentiles) and 35% (N=127) had a satisfactory level of well-being. According to the Insight Scale, only 58% (N=167) of participants had a good level of insight (score ≥9) and 42% of participants had a low level of insight (N=121).
Figure 2 shows the recovery stages and care needs of the participants. The satisfaction scale (adapted from the CASIG) assesses a person’s satisfaction with nine life dimensions. As expected, the higher the dissatisfaction level, the more the participant requested help.
Participant dissatisfaction decreased as progress was made along the recovery path (
Figure 3), except in the last recovery stage. More precisely, the dissatisfaction rate was paradoxically much higher among participants in the final STORI recovery stage (5th stage, growth) than among those in the previous stage (4th stage, rebuilding). In stage 5, the level of dissatisfaction (extracted from the satisfaction scale) was higher than in stage 4 in eight of the nine areas. More than 50% of participants in the growth stage remained dissatisfied with their professional training and employment.
Discussion
The rehabilitation centers and the REHABase cohort project came about thanks to multiple stakeholders, including associations, families, and caregivers. Initial data show that most participants asked for help in four areas: employment, cognitive functioning, symptom management, and interpersonal relationships. The results highlight that the dissatisfaction and needs of participants with serious mental illness vary according to the recovery stage. Those who have reached their final recovery stage still require further help in most areas. The dissatisfaction rates were similar for participants at the beginning and at the end of the recovery process.
Responding to needs is one of the key elements of high-quality care that facilitates recovery (
32). Therefore, psychosocial rehabilitation interventions that focus on participants’ goals should be more effective than other types of intervention (
33). Recovery has been described as comprising five processes (
34): connectedness with others; hope, giving a purpose to recovery and enabling the person to achieve it; identity, i.e., being aware that one is not defined by the illness, although it is a small part of one’s identity; finding meaning in life; and taking responsibility for recovery. One aim in developing the STORI was to establish the stage at which specific care should be offered to a participant and consequently to develop guidelines for providing appropriate care based on an individual’s needs. Given the nonlinear nature of personal recovery, such a goal may be overly ambitious at this time, and future research will be needed to determine whether the recovery process includes five distinct stages or only three, as documented in other models (
35–
38). Despite these limitations, the STORI is useful in clinical practice, because identifying a patient’s current stage of personal recovery can inform clinical decision making about the most appropriate intervention (
38).
Fifty-three percent of the REHABase participants were already actively engaged in recovery (rebuilding phase, 21%; growth phase, 32%). Less than a quarter were still in the moratorium phase, and according to the stages established by Andresen et al. (
24), these participants might still be looking for hope. The REHABase project could help determine the effects of psychiatric rehabilitation on an individual’s progress through recovery in comparison with improvements in clinical and functional outcomes. The data collected in the REHABase project could also be used to suggest a refinement of the stage model proposed by Andresen et al. (
24). The REHABase project may contribute to shifting the culture of care toward more recovery-oriented practices by introducing personal recovery into clinical decision making about psychosocial interventions (
38).
Compared with samples in previous studies and control populations, the REHABase project has a high proportion of participants with relatively low well-being scores. Whereas Tennant et al. (
39) showed that the median WEMWBS score was 50 in a student sample and 51 in a general population sample, with interquartile ranges of 45–55 and 45–56, respectively, the REHABase participants had a median score of 42, with an interquartile range of 16–70. This result reflects the overall altered life satisfaction and self-realization in severe mental illness and ASD.
Initial data on participant employment indicated that only 10% of participants worked in a mainstream environment, 68% were dissatisfied with their professional situation, and 78% expressed a need for help in this area. This finding is consistent with data from previous research—work plays a central role in the recovery process (
40). It is thus necessary to assess a participant’s needs in terms of rehabilitation interventions (
41,
42). In France, persons with schizophrenia have more difficulties accessing employment (employment rate of 11.5%), compared with their counterparts in other countries, such as Germany (employment rate of 30.3%) (
43). Graduating from a university and accessing competitive employment are also challenging for people with ASD. A Swedish sample of 50 participants with ASD who were prospectively followed for 20 years had a graduation rate of 14% and employment rates of 33% or 27%, depending on the presence of psychiatric comorbidities (
44). Professional training or competitive employment was a major life goal for 78% of the participants included in REHABase, and these individuals identified vocational rehabilitation as their primary care need.
REHABase includes various scales that measure a participant’s most unsatisfying dimensions, goals, and life priorities. For example, in the satisfaction scale adapted from CASIG, the care needs and priorities are evaluated in nine dimensions. As expected, the proportion of unsatisfied participants decreased during the recovery process. However, surprisingly, it increased again in the final stage of recovery (i.e., growth) for all the dimensions assessed. This result needs to be interpreted carefully given the cyclical nature of personal recovery and its potential correlations with other variables, such as low insight (
45) and self-stigma (
46). Individuals who are in the growth stage at the beginning of psychiatric rehabilitation and who have low insight into their illness might consider themselves as both recovered from mental illness and dissatisfied with one or more major life activities. Therefore, the effects of psychiatric rehabilitation on personal recovery should be investigated taking into account the fact that such effects will be influenced by the simultaneous changes in insight into illness and self-stigma during the follow-up period. Finally, it is important to note that the study was cross-sectional, and no causal statements can be extracted from the data.
Conclusions
Participants’ needs were not met in several major life activities, and further research is needed to better characterize these needs. Indeed, improving the fit between needs and the care available, which could reduce both the duration and the cost of care, should be a priority, considering the large numbers of individuals affected by serious mental illness and ASD and the need to optimize the use of public funds. Improving our understanding of the trajectories of illness and the effects of psychosocial rehabilitation remains a major challenge. To our knowledge, REHABase is the first national project to collect transnosographic data on psychiatric service users, promoting care strategies based on participants’ self-determination (empowerment). The two main focuses of this project are the functional impact of the disorder on participants’ daily lives and the impact of the psychosocial therapies provided by the psychosocial rehabilitation centers. Future results should improve our understanding of the recovery process.
Furthermore, the REHABase data will be used to study factors that determine or hinder recovery (e.g., self-stigma) (
47,
48). The impact of personalized psychosocial rehabilitation will be reported for several variables: psychosocial condition, cognitive processes, well-being, social inclusion, interpersonal relationships, and professional situation. Finally, by recording the effectiveness of personalized rehabilitation action plans, the REHABase project may be key to improving the quality of care and to developing guidelines.
Acknowledgments
The authors thank Kim Barrett for editorial assistance; Floriane Todoroff for her contribution to the figures; Emmanuel Gauthier and Mara Conil for data management; and the members of the REHABase Network (the following teams have all participated in developing the study: C2RL, Limoges; C2RP, Bordeaux; C3R, Grenoble; CL3R, Lyon; CREATIV & URC Pierre Deniker, Poitiers; and REHALise, Saint-Etienne).