Recognizing the long delay between studies establishing an intervention as evidence based and widespread adoption of the intervention in routine practice (
1), mental health leaders have sought strategies to accelerate this process. Recently, Oslin et al. (
2) suggested using the strategy of exporting evidence-based practices found effective in one population to new populations as a way to close the science-to-practice gap. Similarly, Aarons et al. (
3) encouraged “scaling out” evidence-based interventions to new populations, reasoning that it “can sometimes ‘borrow strength’ from evidence of impact in a prior effectiveness trial.” In this article we explore an emerging literature exemplifying this strategy with individual placement and support (IPS), an evidence-based supported employment model initially developed for people with serious mental illness. Few evidence-based employment interventions have been established for other disability populations, despite compelling humanitarian, empirical, and economic reasons to help people who are unemployed enter or re-enter the workforce. Thus the strategy of offering an intervention proven effective in one population to a different population in similar circumstances is worth examining.
IPS is a well-defined, standardized model of supported employment developed in the United States in the 1980s (
4). IPS follows eight basic principles: the goal of competitive employment, zero exclusion and eligibility based on client choice, attention to client preferences, rapid job search, integration of employment services and mental health treatment, personalized benefits counseling, targeted job development, and individualized, long-term support (
Table 1). A clinical manual for practitioners (
5), two fidelity measures, and many other resources incorporate these principles (
https://ipsworks.org/index.php/library). More than 20 randomized controlled trials, numerous systematic reviews, and published guidelines have concluded that IPS is an evidence-based practice that helps people with serious mental illness achieve mainstream, competitive employment (
6,
7).
The IPS model is practical and well-grounded in principles of evidence-based medicine, which include individualization, integrated care, and shared decision making (
8). Given the nature and characteristics of the IPS model, it may have potential to benefit others beyond people with serious mental illness. IPS has been extended to other populations with disabilities over the past decade, but effectiveness studies for these other disability groups have not been systematically reviewed (
9). This article reports the first systematic review of the effectiveness of IPS for disability groups other than those with serious mental illness.
Methods
To provide an overview of the current state of developments, we used a broad definition of IPS to include programs that were based on the IPS model, with adherence assessed according to fidelity scales, either the 15-item fidelity scale (IPS–15) (
10) or the expanded 25-item fidelity scale (IPS–25) (
11). Multiple observational studies have shown that higher fidelity ratings on these scales are associated with better competitive employment outcomes (
12,
13).
In this systematic review, we emphasized randomized controlled trials, which provide the strongest evidence of effectiveness, but we also examined other pertinent outcome studies (including observational studies) and the protocols for studies in process (to anticipate further developments). We excluded vocational studies not based on the IPS model.
The primary outcome of interest was the competitive employment rate, based on at least one day of competitive employment during follow-up, which is considered a proxy for other employment outcomes. In studies not reporting an employment rate at any time during follow-up but instead reporting the rate at end point, we substituted the latter as an approximation. We also summarized findings for other competitive employment and nonvocational outcomes, such as length of employment, quality of life, and symptoms of illness. Competitive employment signifies a regular community job that anyone can apply for, paying a comparable wage to all who perform the same work (at least minimum wage), an integrated workplace, and the same supervisory arrangements and other conditions for all workers. Competitive jobs differ from sheltered jobs, jobs set aside for people with disabilities, and time-limited jobs intended to provide training or work experiences.
Study Eligibility Criteria
For the systematic review, inclusion criteria were an employment program based on IPS principles, including programs with modifications or augmentations of IPS; a randomized controlled trial; participants drawn from a well-defined population other than people with serious mental illness; a minimum of 10 study participants; and prospective data collection on the competitive employment rate. We excluded studies of transition-age youth (ages 16 to 24) and people with a first episode of psychosis, because these studies typically include people with emerging serious mental illness and have been reviewed elsewhere (
14).
Search Procedures
We used both formal and informal search methods. For the formal search, we conducted a systematic review following PRISMA guidelines (
www.prismastatement.org), using a predetermined but unregistered protocol. During September 2018, we searched three electronic databases — PubMed, Web of Science, and Scopus — for all papers published before that date. We used two search word combinations: “individual placement and support” in the title or abstract and (TITLE-ABS-KEY (“individual placement and support”) OR TITLE-ABS-KEY (ips) AND (TITLE-ABS-KEY (work) OR TITLE-ABS-KEY (employ))) AND LIMIT-TO (SUBJAREA, “MEDI”)).
The informal search included notifications from various listserves (Google Scholar Alert; CSDP Disability Research Consortium) that provide weekly updates of recent papers related to IPS, disability policy, and employment services. Another source consisted of recent systematic reviews of the IPS and vocational rehabilitation literature. Finally, we scanned the reference lists of papers included in the review for additional qualifying studies.
The search process included two screens. First, two authors independently assessed each individual title and abstract, excluding papers that did not meet inclusion criteria. Second, we examined the full text of studies included after the first screen. A third author adjudicated a single disagreement.
In the case of multiple publications based on a single study, we used the first publication reporting the main findings, supplemented as appropriate with other publications (such as reports of long-term follow-up). (A PRISMA diagram summarizing the number of papers identified and excluded at each stage is available in an online supplement to this article.)
Classification of Disability Groups
To classify IPS studies of groups with disabilities other than serious mental illness, we developed a heuristic framework. Although various methods for classifying disabilities have been suggested (
www2.ed.gov/programs/rsabvrs/resources/fy2016-vr-performance-chart.pdf) (
15–
17), researchers have not reached consensus on a standardized classification system. Therefore, we inductively identified three broad categories: psychiatric disorders other than serious mental illness, substance use disorders, and musculoskeletal or neurological disorders. This classification, based on conditions for which IPS programs have been developed, does not exhaust the entire range of disabling conditions. Further, it includes substance use disorder, even though neither the U.S. federal agency responsible for determining disability benefits (Social Security Administration) nor the agency determining eligibility for vocational rehabilitation (Rehabilitation Services Administration) recognizes substance use disorder as a disability. We consider people with substance use disorders an important target group because substance use disorders often impair employment, and employment often plays a critical role in the recovery process (
18).
Statistical Analysis
We used the odds ratio to assess the overall effect size of experimental differences in competitive employment rates across studies by using the Mantel-Haenszel random-effects method. We created a forest plot graph of the meta-analysis by using RevMan 5.3 (
19). We examined heterogeneity by using the I
2 statistic. An I
2 value exceeding 50% indicates substantial heterogeneity.
Results
Overview
Our literature search yielded 1,523 unduplicated records, of which all but 37 were excluded after screening for the title and abstract, as shown in the PRISMA diagram. As shown in
Table 2, nine studies met our inclusion criteria (
20–
28). Overall, the methodological quality was adequate. Seven of the nine studies were registered as trials prior to conducting the study, and the same seven studies reported a CONSORT diagram showing the flow of participants from recruitment to end point (
20–
23,
26–
28). Statistical power was generally adequate; five studies had more than 100 participants, and none had a sample smaller than 45. The nine studies enrolled a total of 2,902 participants. The duration of follow-up was 6 months in two studies and 1 year or more in the others. Two studies (
26,
27) used national registry databases to calculate employment rate during the last month of the follow-up period. Because it is based on a shorter follow-up period, this measure underestimates the employment rate over the full follow-up period for both intervention and control groups. The most common methodological weakness was a lack of detail in the description of the intervention and of the process used to recruit the sample. Below we summarize the findings reported for each study, including design and sample, main and secondary outcomes, and the description of the IPS intervention, including information on IPS fidelity when available and any modifications and augmentations. For two studies reporting long-term outcomes (
26,
28), we also report these findings.
We also summarize findings for six observational studies of IPS for other populations and one secondary analysis of four published trials of IPS for people with serious mental disorder who had co-occurring substance use disorders. Finally, we describe four randomized controlled trials in progress.
IPS for People With Psychiatric Disorders Other Than Serious Mental Illness
Serious mental illness encompasses psychotic disorders such as schizophrenia spectrum disorders, bipolar disorder, and psychotic depression (
29). Researchers have begun studying the effectiveness of IPS and closely related approaches for psychiatric disorders other than serious mental illness, such as common mental disorders, affective disorders, posttraumatic stress disorder (PTSD), and borderline personality disorder. The term common mental disorder refers to depression, anxiety disorders, and adjustment disorders; it excludes schizophrenia-spectrum disorders, bipolar disorder, and other psychotic disorders (
30,
31). The common mental disorder grouping appears frequently in the occupational health literature (
32). We identified six randomized controlled trials of IPS for people with psychiatric disorders other than serious mental illness, four conducted in Scandinavia and two in the U.S.
People with common mental disorders.
Reme et al. (
26) conducted a randomized, controlled, and multicenter trial in Norway assessing return to work for 1,193 participants with common mental disorders. Participants came from three subgroups: employees on sick leave, those at risk of going on sick leave, and those receiving long-term disability benefits. People with common mental disorders met specific criteria on self-reported anxiety or depression scales. The intervention had two components: work-focused cognitive-behaviorial therapy (up to 15 sessions) and individual job support. The first component, work-focused cognitive-behaviorial therapy, is an evidence-based intervention for helping employees with depression return to work after being on sick leave (
33). The individual job support component followed the IPS model and was offered to the 32% of participants requesting job support, primarily those receiving long-term disability benefits. The control group received usual care, including a list of job resources. Because employment measures were extracted from the Norwegian national employee registry, the study had no missing data for the primary outcome.
At 12-month follow-up, 44% of intervention participants were employed, compared with 37% of control participants (p=.02). The statistical differences were maintained at 18 months. The effects of the intervention on the long-term disability group (N=259) were stronger at 12 months (24% versus 12%, p=.007) and 18 months (30% versus 11%). In the full sample, the intervention group also showed significant reductions in depression and anxiety symptoms and significant increases in health-related quality of life, compared with the group who received usual care. The investigators noted challenges in implementing individual job support but did not assess fidelity until after recruitment had ended. They reported that the quality of job support and adherence to IPS for job support were satisfactory.
Øverland et al. (
34), in a long-term follow-up after the intervention ended, found that the results for the long-term disability subgroup significantly favored the intervention group. However, the overall group differences were not sustained in the full sample. Over a 3-year period ending 46 months after baseline, the intervention group did not differ from the control group on income, total months employed, or months employed without receiving sick leave benefits.
This study provided limited information regarding the effectiveness of IPS for people with common mental disorders for two reasons. First, the intervention consisted of two components, confounding the impact of the cognitive-behavioral therapy and individual job support. Second, IPS fidelity was not systematically monitored.
People with mood and anxiety disorders.
Hellström et al. (
23) examined the effects on return to work and education of IPS modified for people with mood and anxiety disorders (IPS-MA) in Denmark, compared with a control group receiving usual services, including stepwise job services. In the study, 326 participants were randomly assigned either to IPS-MA, an intervention consisting of individual mentor support and career counseling (N=162), or to usual services (N=164). After 24 months, 44% of the IPS-MA participants had returned to work or education, compared with 38% of control participants, a nonsignificant difference. The groups also did not differ in number of weeks of employment or education, self-reported well-being, or interviewer-rated depression, anxiety, and global level of functioning.
The study provided a weak test of IPS because modifications eliminated several critical ingredients of IPS: integration of vocational services with mental health treatment, job development, and benefits counseling. The researchers assumed that integration with treatment was impractical because people with mood and anxiety disorders were treated in many different settings in Denmark, often by a general practitioner, psychiatrist, or psychologist. The participants looked for jobs themselves through ordinary job-seeking channels. Benefits counseling was provided on an ad hoc basis. In summary, the program departed sharply from IPS fidelity standards. The authors speculated that the lack of integration reduced the effectiveness of the IPS intervention.
People with affective disorders.
Bejerholm et al. (
20) conducted a randomized controlled trial in four geographically diverse areas of Sweden to evaluate an enhanced version of IPS adapted for people with affective disorders. IPS was enhanced by including an emphasis on motivational interviewing and cognitive strategies. The researchers randomly assigned 61 participants recruited from outpatient clinics to the enhanced IPS program or traditional vocational rehabilitation. Three control participants were lost to follow-up. Over a 12-month period, 42% of clients in the IPS-enhanced condition attained competitive employment, significantly more than in the control condition (4%). The IPS condition also had significantly better outcomes for hours and weeks employed, time to employment, depression, and quality of life. Fidelity ratings indicated that the IPS achieved high fidelity at both 6 and 12 months after the inception of the study.
People with moderate to severe mental illness.
Reme et al. (
27) conducted an 18-month, multisite, randomized controlled trial of IPS in Norway for people with moderate to severe mental illness. The study compared IPS to high-quality usual care (which included “work with assistance” or a traineeship in a sheltered business). The 410 participants enrolled in the study had a range of psychiatric diagnoses (some with multiple diagnoses), including 38% with psychotic disorders, 57% with major depression, 33% with panic disorder, 22% with alcohol/drug dependency, 20% with bipolar disorder, and 19% with general anxiety disorder. The primary outcome measure was competitive employment at 12 and 18 months, as recorded in the Norwegian national registry. All but two deceased IPS participants were included in the intent-to-treat analysis of the registry data. The percentage of participants who were competitively employed was significantly higher in the IPS group than in the control group at both 12 months (37% versus 27%) and 18 months (also 37% versus 27%). The experimental differences were similar, but not statistically significant, for the 164 participants with moderate mental illness (38% versus 28% at 12 months and 38% versus 26% at 18 months).
At 12 months, the IPS group also had significantly greater improvements, compared with the control group, on all the secondary outcomes: psychological distress, symptoms of depression, subjective health complaints, functioning, health-related quality of life, and global well-being. The groups did not differ at 6-, 12-, or 18-month follow-ups on receipt of any disability or unemployment insurance benefits.
Fidelity was initially below the cutoff for fair fidelity for four of nine sites, but at the second and third assessment, fidelity ranged from fair to exemplary at all sites.
Veterans with PTSD.
Davis et al. (
22) conducted a randomized controlled trial of IPS for 85 military veterans with PTSD, comparing IPS with the usual vocational services (a transitional work program) offered at the U.S. Department of Veterans Affairs (VA) medical center in Tuscaloosa, Alabama. During the 12-month follow-up period, 76% of the IPS participants gained competitive employment, compared with 28% of control participants (p<0.001). IPS participants also worked significantly more weeks and earned significantly higher income than did control participants. The authors did not report findings for any secondary, nonvocational outcomes.
The research team monitored IPS fidelity every 3 months over the intervention period. The IPS program steadily improved into the fair range of fidelity during the study.
Davis et al. (21), in a multisite replication study, conducted a randomized controlled trial comparing IPS to a transitional work program for 541 unemployed veterans with PTSD receiving medical treatment at 12 VA medical centers. The primary outcome was steady employment, defined as holding a competitive job for at least 50% of the 18-month follow-up period. The IPS group achieved a significantly higher steady employment rate than did the transitional work group (39% versus 23%, p<0.001). A higher proportion of IPS participants also attained any competitive job (69% versus 57%; p=0.005), and the IPS group had higher cumulative earnings than the control group (p=0.004). Other competitive employment outcomes (days employed, time to first job, employed full time) significantly favored IPS. Change in PTSD symptom ratings marginally favored IPS.
An experienced IPS trainer monitored the IPS programs and provided technical assistance and corrective feedback as needed. With the exception of two sites, all achieved the benchmark for good fidelity after start-up.
Observational studies.
Nygren et al. (
35) conducted a pre-post study in Sweden evaluating IPS for 65 workers on government-funded sick leave. The sample had a mixture of diagnoses, mostly depression or anxiety disorder. Most participants were younger than age 30. Over a 1-year follow-up, 25% of the participants gained employment, and 14% enrolled in an educational program. Participants who worked showed reduced psychiatric symptoms and improved global functioning. The IPS program achieved fair fidelity assessed by using the IPS-15, but it lacked a zero exclusion policy and was not integrated with mental health treatment.
Studies in progress.
A randomized controlled trial was launched in 2018 to evaluate IPS for youth with borderline personality disorder in Melbourne (personal communication, Chanen AM, October 30, 2017). The study examines competitive employment and education outcomes over a 12-month period for 108 youths between ages 15 and 25. Participants will be randomly assigned to IPS or to usual vocational services. Participants in both conditions will receive clinical services through Orygen Youth Health, which offers early intervention to youth with serious mental disorders, including a specialized program for youth with borderline personality disorder (
36).
In preparation for the formal evaluation, a pilot study at the Orygen borderline personality disorder clinic examined outcomes for services provided by a part-time IPS specialist. Over an 18-month period, 11 (48%) of the 23 youths receiving IPS gained competitive employment or started an educational program.
IPS for People With Substance Use Disorder
Two randomized controlled trials of IPS for people with a primary diagnosis of substance use disorder have been conducted. One was a pilot program for people with opioid use disorder who were attending a methadone clinic (
25). The other was an employment program based on IPS for previously incarcerated U.S. veterans with substance use disorders (
24).
People with opioid use disorder.
Lones et al. (
25) conducted a randomized controlled trial of IPS for people with opioid use disorders enrolled in a methadone treatment program in Portland, Oregon. The researchers randomly assigned 45 participants to IPS or a 6-month waitlist. The IPS program consisted of a single IPS specialist who received supervision from an experienced IPS trainer. The IPS specialist attended weekly treatment team meetings at the methadone clinic. The waitlist group was offered IPS 6 months after study enrollment. Over the 6-month follow-up, 50% of the IPS group obtained a competitive job, significantly more than 5% of the control group. The authors did not report any secondary nonvocational outcomes. According to an independent fidelity review, the IPS program achieved fair fidelity.
People with substance use disorders in the criminal justice system.
LePage et al. (
24) developed a group-based vocational program, called About Face (AF). In a randomized controlled trial, they compared AF to an augmentation of AF incorporating IPS principles (AF+IPS) for 84 study participants who were U.S. military veterans with at least one felony conviction. The sample included 88% with a substance use disorder and 45% with depression. Over a 6-month follow-up, 46% of the AF+IPS group gained employment, significantly more than 21% in the AF-only group. The AF+IPS group also worked significantly more hours and earned more wages than the AF-only group, but nonvocational outcomes were not reported. The authors rated the AF+IPS program as attaining fair fidelity.
Observational studies.
Several randomized controlled trials of IPS for clients with serious mental illness have included a substantial proportion of clients with co-occurring substance use disorders. In these studies, IPS participants typically have had significantly better employment outcomes than control participants. For example, Mueser et al. (
37) conducted a secondary analysis aggregating outcomes from four randomized controlled trials of IPS, comparing experimental differences for 106 clients with a recent substance use disorder, and found that 60% of IPS participants with co-occurring mental illness and substance use disorder obtained competitive employment, significantly more than 24% of the control groups.
Several program evaluations have examined IPS employment services within the VA system. In these studies, the samples have been mixed diagnostically, but most participants had a diagnosis of alcohol use disorder or drug use disorder, often co-occurring with a psychiatric disorder. Rosenheck and Mares (
38) assessed outcomes for 321 homeless veterans with substance use disorders or psychiatric disorders in IPS, compared with a historical control group, and found significantly better competitive employment outcomes for the IPS group. Leddy et al. (
39) examined competitive employment outcomes for 440 veterans enrolled in IPS employment services in nine VA hospitals. Compared with veterans referred to transitional VA vocational interventions, those in IPS were significantly more likely to be competitively employed 6 months after referral. Neither study had robust methods for monitoring IPS fidelity.
Studies in progress.
In the United Kingdom, Marsden launched the IPS–Alcohol and Drug Dependency Trial (IPS-AD) in 2018. This multisite, randomized controlled trial of IPS plans to enroll 2,400 participants in seven sites (clinical trial registration, doi.org/10.1186/ISRCTN24159790).
IPS for People With Musculoskeletal and Neurological Disorders
Musculoskeletal and neurological disorders include injuries or pain affecting the musculoskeletal system and neurological impairments affecting role functioning, including work functioning. This broad classification includes spinal cord injuries, pain syndromes, and traumatic brain injuries. Although rehabilitation programs for people with musculoskeletal and neurological disorders are widespread, U.S. rehabilitation programs usually address aspects of physical rehabilitation such as mobility and tasks of daily living, and few include vocational rehabilitation interventions. Outside the United States, return-to-work programs for employees with injuries or illness and employment interventions for musculoskeletal disorders are more common, with a large evidence base (
40). This literature is mostly limited to interventions for employees and typically excludes people not in the labor force. We found only one controlled study of IPS, one observational study, and two protocols.
Veterans with spinal cord injury.
Ottomanelli et al. (
28) conducted a randomized controlled trial comparing IPS to treatment as usual, including referral to state vocational rehabilitation, for U.S. military veterans with spinal cord injuries. The multisite study recruited veterans being treated at spinal cord injury clinics in six VA medical centers and randomly assigned 81 participants to IPS and 76 participants to treatment as usual. Another 44 veterans treated at VA medical centers not participating in the randomized study served as a second control group (the “observational” control group). Over a 1-year follow-up period, the IPS group had a significantly higher rate of competitive employment than either control group: 26% of IPS participants, compared with 11% and 2%, respectively, of the randomly assigned and observational control groups. At 2-year follow-up, the findings were stronger, with additional IPS participants gaining competitive employment and no change in the two control groups: 31% of IPS participants, compared with 11% and 2%, respectively, of the two control groups (
41).
Ottomanelli et al. (
42) also examined changes over time in health-related quality of life, disability, social integration, and mobility by using self-report questionnaires but found no differences between IPS and control participants. Participants who held a competitive job reported significantly better social integration and mobility.
The research team monitored IPS fidelity every 6 months over the intervention period by using the IPS-15. Overall the IPS programs were rated in the fair range for fidelity, reflecting modifications to the IPS model necessitated by the nature of spinal cord injury. For example, employment services were integrated with the medical treatment for spinal cord injury rather than with mental health care. Other modifications made to the IPS model for this population included different approaches to disclosure and job development (
43).
Observational studies.
Rødevand et al. (
44) conducted a pilot interview study of IPS for eight patients with chronic pain in a Norwegian hospital outpatient pain clinic. Over a 12-month period, three patients (38%) gained employment. All but one patient reported favorable experience with IPS; the one exception withdrew from IPS when his symptoms worsened. This study suggested that IPS could be successfully integrated with a multidisciplinary pain rehabilitation program.
Studies in progress.
Linnemørken et al. (
45) described a randomized controlled trial evaluating the effectiveness of IPS for unemployed Norwegians receiving treatment for chronic pain at a hospital outpatient clinic. All participants will receive multidisciplinary pain management. The IPS program will be implemented according to the Norwegian translation of the IPS manual (
5) and integrated with pain management services. The control group will receive a resource manual on community employment services. The research team plans to enroll 80 participants and follow them for 2 years.
Howe et al. (
46) described a protocol for a randomized controlled trial in Norway to evaluate the effects of a vocational intervention for patients with mild to moderate traumatic brain injury. The intervention integrates cognitive rehabilitation training with supported employment, based loosely on IPS fidelity standards. The control condition will be treatment as usual, described as usual rehabilitation services provided by a multidisciplinary rehabilitation team. The study will examine the impact of the intervention on competitive employment outcomes, including work productivity, and changes in self-reported symptoms, emotional and cognitive functioning, and quality of life.
Observational Studies of IPS for Other Populations
Youth with developmental disabilities.
Noel et al. (
47) conducted a program evaluation of a statewide implementation of IPS for high school students with intellectual disabilities or psychiatric disabilities in Illinois. The state vocational rehabilitation agency led this study, facilitating collaboration between 10 community mental health centers and local school systems. The participating sites all initiated IPS services and successfully enrolled youth into their IPS programs.
IPS program leaders assessed competitive employment outcomes by using a program-level quarterly employment rate (number of clients competitively employed at some time divided by the total number of IPS clients enrolled during a quarter). In the last quarter of the follow-up period, the mean quarterly employment rate for the 10 sites was 36%.
Fidelity reviewers from the state agency completed fidelity reviews by using the IPS-25. Four of the 10 sites met the IPS fidelity standards for good fidelity. The main implementation barriers for these start-up programs were a lack of collaboration between IPS and the schools, competing expectations, and stigma. In addition, in several sites, the IPS program was competing with existing prevocational programs that were firmly entrenched in the school systems.
People with autism spectrum disorders.
McLaren et al. (
48) described a pilot IPS program for five young adults with autism spectrum disorders who obtained and maintained competitive employment within 1 year. In addition to gaining employment, participants and their families also reported improvements in independence, self-confidence, and family relationships. The IPS program, consisting of a single half-time IPS specialist, achieved good IPS fidelity. One limitation was the lack of organizational support because the program was located within a large teaching hospital with no history of providing employment services.
Synthesis
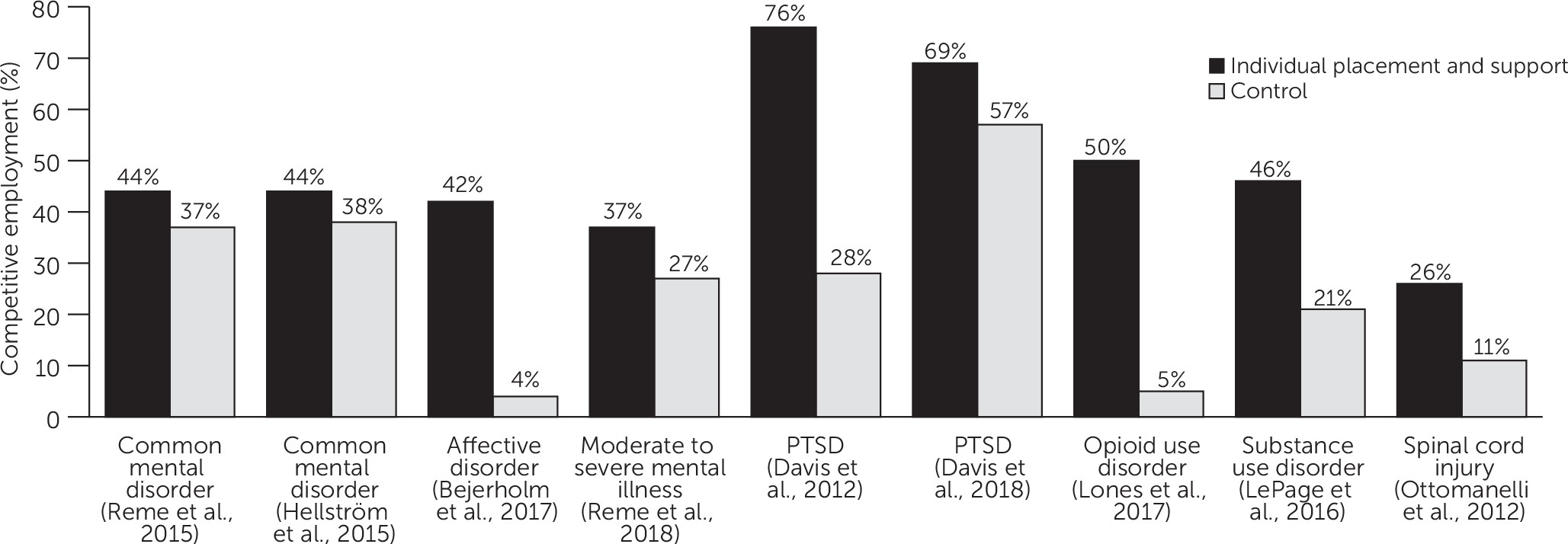
Figure 1 shows the competitive employment rates in nine randomized controlled trials of IPS in populations other than those with serious mental illness. In eight of nine studies the competitive employment rate was significantly higher for the IPS group than for the control group.
Figure 2 displays a forest plot showing the odds ratio effect size for each study and the overall effect size. The forest plot provides a visual representation of the overall positive findings. The overall weighted odds ratio was 2.23 (95% confidence interval [CI]=1.53–3.24, p<0.001). It is not surprising, given the diversity of disability groups included in the analysis, that the index of heterogeneity (I
2) was large, indicating high heterogeneity. Therefore, the overall odds ratio generated by the meta-analysis should be interpreted cautiously.
Other employment outcomes were consistently positive in these studies. On the other hand, the findings were mixed for nonvocational outcomes, such as symptoms and quality of life, although not all studies measured these outcomes.
Discussion
IPS, developed and validated for people with serious mental illness, has been increasingly used to help other populations achieve competitive employment. Research on its effectiveness in other populations has developed rapidly, with two controlled trials published in 2012, seven trials published since 2015, and several additional controlled trials in progress. Five of the nine controlled trials included in this systematic review had small sample sizes (<100), suggesting that much of the current evidence base should be regarded as tentative. Nevertheless, the findings have been encouraging, with eight of nine studies showing significantly higher competitive employment rates for IPS. The meta-analysis, which provided a synthesis of these nine studies spanning diverse disability groups, offered further support for the conclusion that IPS had much better competitive employment rates overall. Although further research is needed, the current review supports the strategy of offering IPS, an intervention proven effective in one population, to other disability groups in similar circumstances.
The findings for effectiveness of IPS for veterans with PTSD have been replicated in a multisite trial, lending strength to the conclusions for that population. Among the other studied populations, the IPS results were weaker and had not been replicated.
The published research, including observational studies and case reports, has thus far not shown any negative evidence for IPS. In the absence of such data, IPS offers a potentially beneficial employment model for all disability groups, warranting additional rigorous research studies. Because the employment rates for IPS in this review varied by disability group, drawing conclusions about groups other than veterans with PTSD would be premature.
Although other employment outcomes were also positive in these studies, the findings regarding nonvocational outcomes had inconsistent measures and results. Several studies also augmented IPS with cognitive-behavioral therapy, confounding any results for symptom reduction. Several studies included in the systematic review also had substantial attrition in self-reporting of nonvocational outcomes, also suggesting caution. Randomized controlled trials of IPS for people with serious mental illness have typically found symptom control and quality of life improvements accrue to both IPS and control participants who become employed, rather than specifically to those assigned to IPS (
49,
50). We would expect similar findings (employment correlated with nonvocational outcomes) in populations other than people with serious mental illness.
Reviews of randomized controlled trials of IPS for people with serious mental illness have reported mean competitive employment rates across studies exceeding 50% for IPS and about half that rate for control groups (
7,
51,
52). Using 50% for IPS as a benchmark, only the two studies of veterans with PTSD and the study of people with opioid use disorder reached this benchmark. Furthermore, comparisons between the current studies and the extant IPS literature ignore confounding variables, including modifications to the IPS model, adherence to fidelity, and national policies in other countries. For example, in Scandinavia, where several studies were conducted, national policies foster high job security and generous welfare benefits, which provide disincentives to working and suppress employment rates, for both IPS and control participants (
53).
Our review does not clarify whether employment services must be tailored to the characteristics associated with a specific disability or condition. People in all disability groups are heterogeneous and probably need an individualized approach like IPS, undergirded with a set of pragmatic principles that are not specific to any impairment or condition. Many challenges facing anyone who is unemployed are similar regardless of a person’s specific disability or condition. Modifications to IPS fidelity standards may be necessary in some cases, but IPS principles thus far appear to be appropriate across disabilities.
Workers who have become unemployed by circumstance (such as factory closings, automation, or industry changes) or who face social disadvantages in the labor market (such as members of racial-ethnic minority groups and refugees [
54]), are of great interest to economists, society, and policy makers (
55,
56). Although studies of such populations were not included in this review, IPS is also being adopted for groups defined by their receipt of welfare or unemployment benefits rather than by their disability or medical condition (
57,
58).
Limitations in the studies reviewed in this article included some small samples, departures from the IPS model, short follow-up periods, and lack of replications. Although some modifications to IPS are clearly warranted (for example, changes related to the type of health services in which IPS is embedded), the need for other deviations is unclear and needs further research. The meta-analysis was limited by differing follow-up time frames, heterogeneity of the populations served, use of nonstandardized interventions by control groups, and the influences of diverse disability policies and labor laws in the nations where the studies were conducted.
Conclusions
This first systematic review of the effects of IPS supported employment for populations other than people with serious mental illness showed generally positive results on competitive employment for diverse populations, including people with anxiety, depression, PTSD, spinal cord injury, or substance use disorders. But studies were limited by number (only nine controlled trials), small sample sizes, lack of replication (only research on veterans with PTSD has been replicated), diverse modifications, and uncertain fidelity. Nevertheless, these positive initial findings should lead to further trials with other disability populations and possibly to modification of IPS for different populations. Although more research is needed to establish generalizability, IPS should be offered to veterans with PTSD. We also recommend exporting IPS to other new populations, including civilians with PTSD.