Interventions to Improve Metabolic Risk Screening Among Adult Patients Taking Antipsychotic Medication: A Systematic Review
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Methods
Overview
Search Strategy
Criteria for Study Selection
Inclusion criteria.
Exclusion criteria.
Data Extraction and Classification
Outcome Measures
Quality Assessment
Data Analysis
Results
Characteristics of Included Studies
| Study | Country | Setting | Populationb | Intervention | Design/intervention duration | Sample size (comparison/intervention group) | Synopsis of findings |
|---|---|---|---|---|---|---|---|
| Abdallah et al., 2016 (29) | UK | MH outpatient, community | Schizophrenia; any oral antipsychotic and long-acting depot treatment in MH; exclusion of clozapine | Intervention targeted the primary care–MH care interface; MH clinicians liaised with GPs via letters to improve metabolic screening; patients empowered to seek general medical care with their GPs; care home staff participated in monitoring of weight and BP. | Prospective audit with 10 weeks of follow-up/10 weeks | 95/33 | Improvement was noted in GPs’ performance of monitoring; care homes took on responsibility to monitor weight and BP; optimal monitoring achieved for glucose. |
| Barnes et al., 2008 (31) | UK | MH outpatient, community | SMI; psychotic spectrum disorders, 82%/84%; mood disorders, 13%/12%; SGA, 62%/65%; FGA, 36%/33% | QIP that included a benchmarked audit of baseline monitoring delivered to providers; educational activities for providers; lifestyle management pack for providers and patients; physical health check reminder card given to patients | Retrospective audit with 1 year of follow-up after intervention/1 year | 1,966/1,516 | Proportion of patients screened for four metabolic measures increased from 11% to 23%. |
| Barnes et al., 2015 (30) | UK | MH outpatient, community | SMI; psychotic spectrum disorders, 72%; mood disorders, 13%; any antipsychotic | QIP that included a benchmarked audit of baseline monitoring delivered to providers; educational activities for providers; lifestyle management pack for providers and patients; physical health check reminder card given to patients | Retrospective audits in 6 years; up to 6 years of follow-up after intervention/1 year | 1,966/1,591 | Proportion of patients screened for four metabolic measures increased from 11% to 34%; over 60% of patients were screened by the MH providers. |
| Cotes et al., 2015 (32) | USA | MH outpatient, community | SMI; any antipsychotic | QIP with provider and leadership education; education of patients and family; local leaders given results of benchmarked monitoring audits | Retrospective audit with up to 22 months of follow-up after intervention/22 months | 230/265 | The 10 MH centers audited varied widely in intervention uptake; despite local increases in MM, no significant change was seen at the state level. |
| DelMonte et al., 2012 (27); Lee et al., 2016 (28)c | USA | MH inpatient | SMI; mood disorders, 51%/51%; psychotic spectrum disorders, 36%/36%; SGA only | Clinicians ordering SGA for inpatients received a “pop-up” reminder in EMR to order glucose and lipid testing; a dedicated clinician (“champion”) supported provider behavior change. | Retrospective audit with up to 4 years of follow-up after intervention/4 years | 171/129 | Implementation of a “pop-up” alert in an inpatient EMR increased the proportion of patients with both glucose and lipid testing from 13% to 48% at 6 months and 51% at 4 years. |
| Fischler et al., 2016 (33) | Canada | MH inpatient | Schizophrenia, schizoaffective disorder; any antipsychotic | An implementation study to improve adherence with schizophrenia CPG; CDSS ordered complete MM when antipsychotics were prescribed; clinicians and leaders received benchmarked feedback on their performance. | Prospective audit with up to 12 months of follow-up after intervention/12 months | 192/184 | Proportion of patients screened for four metabolic measures increased from 36% to 56%. |
| Gallagher et al., 2013 (34) | Ireland | MH outpatient, community | SMI; schizophrenia, 48%/50%; mood disorders, 33%/30%; SGA, 90%/93%; FGA, 20%/15%; exclusion of clozapine | Patients on antipsychotics were identified by a registry and summoned to a health screening and promotion clinic to conduct MM; patients were educated about the need for monitoring; liaison with GPs for treatment of metabolic abnormalities; patients’ records were supplemented with a designated MM sheet. | Prospective audit with up to 3 months of follow-up after intervention/2 clinic days during 3 months | 40/40 | Attendance rates for health promotion clinic were over 70%; all four metabolic measures were screened in over 75% of patients. |
| Gill et al., 2016 (35) | Ireland | MH outpatient, community | SMI; any long-term depot antipsychotic | Patients were invited by letter to attend a semiannual health monitoring clinic staffed by psychiatrists, nurses, and an administrator; clinic conducted MM; liaison with GPs for treatment of metabolic abnormalities; patients’ records were supplemented with a designated MM sheet. | Prospective interrupted time-series with 1 year of follow-up after intervention/1 year | 23/23 | Attendance rates for health promotion clinic were over 90%; screening for glucose and lipids increased from 9% to 61% following the intervention. |
| Gonzalez et al., 2010 (36) | UK | MH outpatient | SMI; any antipsychotic, excluding clozapine | MM practice was audited and results were communicated to senior physicians; brief educational sessions were delivered to physicians; patients’ records were supplemented with a designated MM sheet. | Retrospective audit with 1 year of follow-up after intervention/1 year | 126/106 | Intervention achieved increases in MM rates; MM sheet was implemented in nearly half the charts. |
| Green et al., 2018 (37) | UK | MH inpatient | SMI; any antipsychotic | QIP that was overseen by an implementation science expert; input from clinicians and patients before and during the program; monitoring tool was created; education given to staff and patients | Retrospective baseline audit of 10 months; prospective audit with 15 months of follow-up/15 months | 247/318 | Improvements were observed in MM for BMI and BP; QIP education and codesign with patients was well received by the clinical team. |
| Gumber et al., 2010 (38) | UK | MH outpatient | SMI; SGA only | Patients taking antipsychotics were identified by a registry and referred to a metabolic clinic for MM; GPs received the results of the monitoring; physicians received benchmarked audit and educational activities; patients’ records were supplemented with a designated MM sheet. | Prospective audit with up to 12 months of follow-up after intervention/ongoing clinic with 1–2 months of implementation and promotion of clinic | 54/110 | High monitoring rates in the comparison group obscured possible effects of the intervention; no changes in monitoring were observed. |
| Hinds et al., 2015 (39) | USA | MH outpatient, academic | SMI; SGA only; excluding known diagnosis of diabetes | Pharmacist-led initiative to promote glucose monitoring; EMR database used to identify gaps in glucose testing; electronic alert sent to treating physician to conduct MM | Prospective audit with up to 3 months of follow-up after intervention/3 months | 104/86 | A 10% absolute increase in screening rates of a glucose measure was observed. |
| Hor et al., 2016 (40) | Malaysia | MH outpatient, general hospital | SMI; psychotic spectrum disorders, 75%; mood disorders, 15%; any antipsychotic | MM protocol was developed and endorsed by clinical leaders; patients’ records were supplemented with a designated MM sheet; protocol assigned responsibility for MM to specific team members; barriers to monitoring were assessed. | Prospective audit with up to 1 week of follow-up after intervention/1 week | 300/32 | Anthropometric measures saw a greater increase than blood testing; waist circumference was measured less often because of cultural and religious barriers. |
| Kioko et al., 2016 (41) | USA | MH outpatient, community | SMI; SGA only | QIP with implementation of a paper MM tool; clinical staff educated on metabolic health | Prospective audit with up to 3 weeks of follow-up after intervention/3 weeks | 50/50 | Intervention group was associated with increases in monitoring for glucose and lipids, relative to comparison group. |
| Kirchner et al., 2016 (42) | USA | MH inpatient and outpatient, VA | Schizophrenia, schizoaffective disorder; any antipsychotic | QIP that was overseen by an implementation science expert; clinicians received educational materials and electronic reminders in EMRs; audit and feedback of monitoring rates were given to clinicians and managers; patients in need of MM were identified on a weekly basis by the EMR, and this was communicated to the metabolic champion. | Prospective audit with up to 6 months of follow-up after intervention/6 months | 17/15 | Intervention was associated with increases in monitoring for weight, glucose, and lipids, relative to comparison group. |
| Kreyenbuhl et al., 2016 (43) | USA | MH outpatient, VA | SMI; mood disorders, 58%; psychotic spectrum disorders, 30%; SGA only; excluding known diagnosis of dementia | Intervention targeted patients as agents of change; patients received personalized feedback on their MM and education on metabolic health via tablet devices in waiting rooms; patients were empowered to discuss metabolic health with their provider; the comparison group received generic printed materials on metabolic health without personalized information. | Randomized controlled trial of 1-year duration | 119/120 | No changes in monitoring were observed; high monitoring rates in the comparison group obscured possible effects of the intervention. |
| Lai et al., 2015 (44) | Taiwan | MH outpatient, psychiatric hospital | Schizophrenia; SGA only | EMRs were supplemented with an electronic prompt for physicians to conduct MM. | Retrospective interrupted time-series; 2 years before and 2 years after intervention/2 years | 38/37 | Intervention increased rates of patient visits adherent with monitoring guidelines, among those prescribed high-risk (clozapine or olanzapine) versus intermediate-risk SGAs. |
| Latoo et al., 2015 (45) | UK | MH outpatient, community | EIP; any antipsychotic | QIP that was overseen by a multidisciplinary clinical team and patients; barriers to MM were assessed; a monitoring tool and clinical prompts were introduced; collaboration with GPs increased, and specialized physical health clinics were introduced. | Retrospective audit with 6 months of follow-up after intervention/6 months | 55/52 | Screening for all four metabolic measures increased from 7% to 40% after the intervention. |
| Lui et al., 2016 (46) | USA | MH inpatient | SMI; any antipsychotic | Implementation of a mandatory admission electronic order set that included all four metabolic measures | Retrospective audit with 6 months of follow-up after intervention/6 months | 9,100/1,499 | Screening for all four metabolic measures increased from 2% to 100% after the intervention. |
| Nicol et al., 2011 (47) | USA | MH outpatient, community and academic | SMI; SGA only | A registry of patients treated by SGA was created; charts of patients due for monitoring were flagged; screening was encouraged by leadership; providers received benchmarked audits; intervention was biphasic, with the aim of gradually improving screening practices over time. | Prospective interrupted time-series with up to 3 years of follow-up after intervention/3 years | 7,300/2,000 | An increase was observed in the screening rate for glucose from 46% at baseline to 67% and 90% after 1 and 3 years, respectively. |
| Osborn et al., 2010 (48) | UK | MH outpatient | SMI; psychotic spectrum disorders, 59%/50%; mood disorders, 22%/23%; SGA, 68%/61%; FGA, 19%/11%; unmedicated, 13%/28% | Nurse-led intervention at the primary care–MH care interface; nurse liaised with primary care and later MH providers to conduct MM; nurse to conduct MM if this was not done by either provider; comparison group was treatment as usual; both groups received an education pack on MM and metabolic health directed at providers and patients. | Cluster randomized controlled trial of 6 months’ duration | 59/62 | Increased rates of MM in intervention and to a lesser extent in comparison group; most MM conducted by nurse and primary care services and not MH providers. |
| Ramanuj, 2013 (49) | UK | MH inpatient | SMI; psychotic spectrum disorders, 39%/32%; mood disorders, 33%/40%; any antipsychotic | Physicians received a benchmarked audit of MM in their service and educational activities; clinical areas were augmented with visual posters promoting MM. | Prospective audit with up to 13 months of follow-up after intervention/13 months | 16/10 | Intervention group saw increases (60%) in monitoring for lipids, relative to comparison group (25%). |
| Runcie et al., 2007 (50) | UK | MH inpatient | SMI; any antipsychotic | Local MM protocol was developed and endorsed by clinical leaders; protocol was disseminated by letters to all physicians. | Retrospective audit with 3 months of follow-up after intervention/3 months | 51/61 | Wards with a dedicated metabolic clinician showed improved monitoring; intervention did not lead to increases in monitoring overall; however, local influence of metabolic champion was noted. |
| Thompson et al., 2011 (51) | Australia | MH outpatient, community | EIP; SGA only | Physicians received education and a benchmarked audit of MM practice; local MM protocol was developed and visually displayed in clinical areas; patients’ records were supplemented with a designated MM sheet. | Prospective audit with up to 30 months of follow-up after intervention/6 months | 106/86 | Screening for all four metabolic measures increased in the intervention versus the comparison group from 22% to 81%. |
| Tully et al., 2012 (52) | Ireland | MH outpatient, community | SMI; clozapine treatment | Local MM protocol was developed; patients’ records were supplemented with a designated MM sheet; ongoing educational sessions for clinicians were conducted. | Prospective audit with up to 1 year of follow-up after intervention/1 year | 84/74 | Glucose and lipids screening in the intervention group increased to 65% and 70%, respectively; the monitoring protocol was implemented in 92% of the charts. |
| Vasudev and Martindale, 2010 (53) | UK | MH outpatient, community | EIP; any antipsychotic; unmedicated, 9%/11% | Intervention targeted the primary care–MH care interface; EIP clinicians liaised with GP via letters to facilitate physical check-ups; EIP patients were included in SMI registry of primary care; EIP clinicians received an educational workshop. | Prospective audit with up to 6 months of follow-up after intervention/6 months | 66/76 | The number of patients for whom cardiometabolic risk screening was completed by primary care providers increased from 20% to 58% after the intervention. |
| Velligan et al., 2013 (54) | USA | MH outpatient, community | SMI; SGA only | QIP that included an implementation working group that oversaw educational interventions and monitoring procedures; patients’ records were supplemented with a designated MM sheet. | Prospective controlled interrupted time-series with up to 2 years of follow-up after intervention/2 years | 100/50/ | Rates of screening for anthropometric measures increased from 0% to 80% in the intervention clinic and remained lower than 10% at the control clinics. |
| Wiechers et al., 2012 (55) | USA | MH outpatient, academic | SMI; mood disorders, 72%; psychotic spectrum disorders, 33%; any antipsychotic | QIP in a resident-led clinic; physicians received educational sessions; barriers for MM were assessed in focus groups; patients received instruction on fasting lab testing; EMR was enhanced with designated fields to record MM. | Prospective audit with up to 1 year of follow-up after intervention/1 year | 140/131 | Screening for all four metabolic measures increased in the intervention (31%) versus the comparison group, (1%). |
| Wilson et al., 2014 (56) | Australia | MH outpatient, psychiatric hospital | SMI; clozapine treatment | 2 months in a year were chosen as “physical health months” and were promoted visually and educationally to both physicians and patients by clinical directors; during this time, all patients were to be monitored; patients’ records were supplemented with a designated MM sheet. | Prospective audit with up to 1 year of follow-up after intervention/2 months plus 2 months | 107/232 | Screening rates for four metabolic measures exceeded 85% in the intervention group. |
Quality Assessment of Included Studies
Categorization and Description of Improvement Strategies
| Provider | Patient | System | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | N of improvement strategies | Education | Personalized audit and feedback | Clinical promptsa | MM toolb | Education | Empowerment | Leadership support | Patient identification | Collaboration with primary care | Clinical champion for monitoring | Practice audit and feedback | CDSSc | Barrier assessment |
| Abdallah et al., 2016 (29) | 5 | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Barnes et al., 2008 (31) | 7 | ✓ | ✓ | ✓ (v) | ✓ | ✓ | ✓ | ✓ | ||||||
| Barnes et al., 2015 (30) | 6 | ✓ | ✓ | ✓ (v) | ✓ | ✓ | ✓ | |||||||
| Cotes et al., 2015 (32) | 4 | ✓ | ✓ | ✓ | ✓ | |||||||||
| DelMonte et al., 2012 (27); Lee et al., 2016 (28) | 3 | ✓ | ✓ (e) | ✓ | ||||||||||
| Fischler et al., 2016 (33) | 9 | ✓ | ✓ | ✓ (e) | ✓ (e) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Gallagher et al., 2013 (34) | 6 | ✓ (p) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Gill et al., 2016 (35) | 7 | ✓ (p) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Gonzalez et al., 2010 (36) | 4 | ✓ | ✓ | ✓ (p) | ✓ | |||||||||
| Green et al., 2018 (37) | 8 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Gumber et al., 2010 (38) | 5 | ✓ | ✓ | ✓ (p) | ✓ | ✓ | ||||||||
| Hinds et al., 2015 (39) | 3 | ✓ (e) | ✓ | ✓ | ||||||||||
| Hor et al., 2016 (40) | 4 | ✓ (p) | ✓ | ✓ | ✓ | |||||||||
| Kioko et al., 2016 (41) | 3 | ✓ | ✓ (p) | ✓ | ||||||||||
| Kirchner et al., 2016 (42) | 8 | ✓ | ✓ | ✓ (e) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Kreyenbuhl et al., 2016 (43) | 2 | ✓ | ✓ | |||||||||||
| Lai et al., 2015 (44) | 2 | ✓ (e) | ✓ | |||||||||||
| Latoo et al., 2015 (45) | 9 | ✓ | ✓ | ✓ (e) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Lui et al., 2016 (46) | 1 | ✓ | ||||||||||||
| Nicol et al., 2011 (47) | 6 | ✓ | ✓ | ✓ (p) | ✓ | ✓ | ✓ | |||||||
| Osborn et al., 2010 (48) Full | 5 | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Osborn et al., 2010 (48) Partial | 2 | ✓ | ✓ | |||||||||||
| Ramanuj, 2013 (49) | 5 | ✓ | ✓ | ✓ (v) | ✓ | ✓ | ||||||||
| Runcie et al., 2007 (50) | 3 | ✓ | ✓ | ✓ | ||||||||||
| Thompson et al., 2011 (51) | 6 | ✓ | ✓ | ✓ (v, p) | ✓ | ✓ | ✓ | |||||||
| Tully et al., 2012 (52) | 3 | ✓ | ✓ (p) | ✓ | ||||||||||
| Vasudev and Martindale, 2010 (53) | 7 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Velligan et al., 2013 (54) | 8 | ✓ | ✓ | ✓ (p) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Wiechers et al., 2012 (55) | 5 | ✓ | ✓ (e) | ✓ | ✓ | ✓ | ||||||||
| Wilson et al., 2014 (56) | 8 | ✓ | ✓ | ✓ (p, v) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
Improvement strategies targeting providers.
Improvement strategies targeting patients.
Improvement strategies targeting systemic issues.
Intervention Effects on Metabolic Risk Screening
| Proportion screened (%) | |||||||
|---|---|---|---|---|---|---|---|
| N of | Comparison group | Intervention group | |||||
| Measure | studies | Mdn | Min | Max | Mdn | Min | Max |
| Glucose | 21 | 28 | 0 | 92 | 65 | 13 | 100 |
| Lipids | 18 | 22 | 5 | 99 | 61 | 27 | 97 |
| Body mass index, weight | 16 | 19 | 0 | 99 | 67 | 34 | 100 |
| Waist circumference | 6 | 2 | 1 | 99 | 87 | 7 | 100 |
| Blood pressure | 15 | 22 | 3 | 100 | 80 | 38 | 99 |
| All four measuresa | 8 | 11 | 0 | 36 | 57 | 23 | 100 |
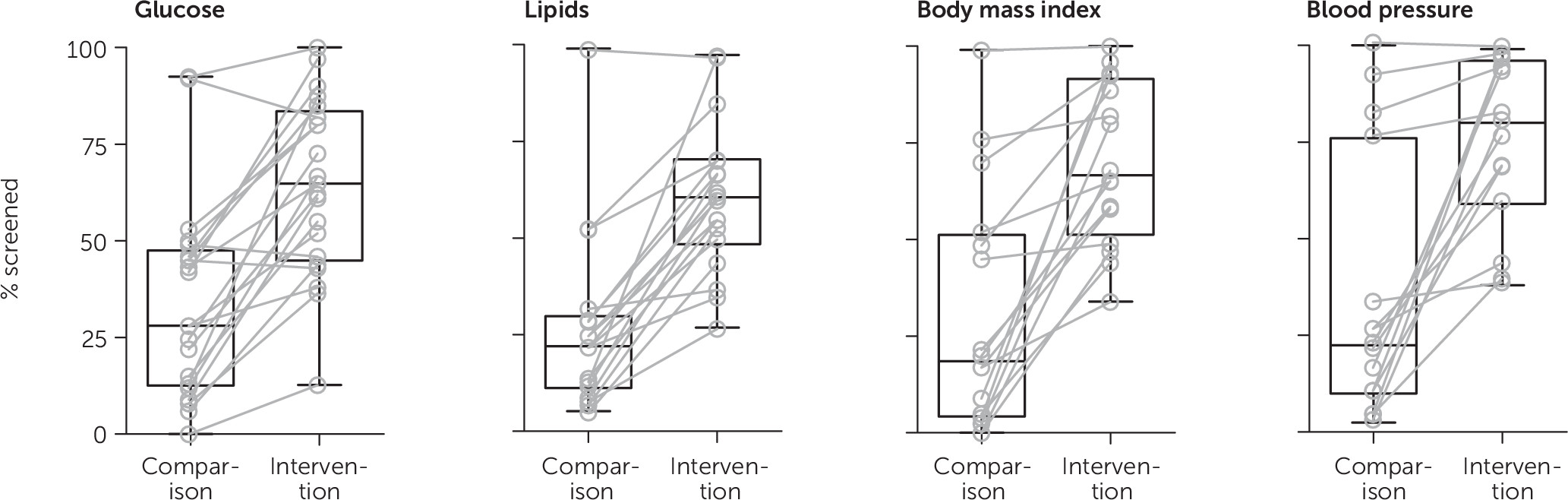
Intervention effects on glucose and lipids screening.
Intervention effects on anthropometric and physical measurements.
Additional summary of intervention effects.
Discussion
Conclusions
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 181.47 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).