Pregnancy-related, or perinatal, depression (
1) is depression during pregnancy or up to 1 year postpartum. It is the most common complication of pregnancy for mothers nationwide and is a serious threat to a mother’s ability to provide responsive and nurturing parenting. It has an estimated prevalence rate of 8%–19% nationwide (
2). Studies have documented even higher rates in low-income populations, with measured prevalence as high as 59% for socioeconomically disadvantaged mothers (
3). Perinatal depression is a burden not only to the mother who is experiencing depressive symptoms but also to her entire family system, with potential lifelong implications for infants in a critical developmental window (
4). When maladaptive neural patterns are set during critical developmental periods, they are difficult to change later in life (
4,
5). High rates of unidentified and untreated maternal depression lead to negative life outcomes for mothers and children as well as potentially avoidable lifetime health and societal costs (
3,
6,
7).
Early identification and treatment of perinatal depression can improve outcomes for mothers and children by promoting both parenting success and early childhood development (
8). Screening and diagnosis in primary care settings is an effective way to increase identification of perinatal depression (
9). Available data indicate that routine perinatal and postpartum depression screening is undertaken in only 15%–20% of women; of those diagnosed through screening, only 40%–60% will receive treatment (
3).
Integrated care, the provision of behavioral health treatment in primary care and other medical outpatient settings, improves rates of detection and treatment and patient outcomes while reducing overall health care costs by leveraging team and population health care models (
10–
17). Integrated care is known to improve behavioral health care access, a particular challenge in rural and socioeconomically disadvantaged populations (
18). Because of the elevated risk of behavioral health challenges for perinatal women, integrated obstetric and gynecological (OB-GYN) care models are particularly important and have shown improvements in depression, adherence, and overall treatment satisfaction (
19,
20). Effective models include psychiatry, psychology, and social supports and have been pragmatically and effectively implemented, including with larger, socioeconomically disadvantaged populations (
5,
19,
21,
22). Findings from a 2016 meta-analysis of computer and Web-based interventions for perinatal mental health suggested that they also show promise for effective treatment of perinatal depression and complicated grief (
22).
Virtual health technologies, particularly telepsychiatry, in the form of live interactive video conferencing, are demonstrating their importance in addressing challenges in integrated care delivery. Integrated care with telepsychiatry improves access and availability to psychiatric providers, increases workflow efficiency, enables scaling of integrated care services, and improves patient outcomes (
16). Despite the promise of telepsychiatry for perinatal care, a review of the literature revealed no reports or evaluations on perinatal telepsychiatry outside of a policy review and assessment of feasibility of implementation (
18).
We sought to pilot a model of telepsychiatry-enabled integrated care for an underserved perinatal population. We hypothesized that this model would improve screening and identification of depression and other perinatal mental health issues, increase access to treatment, and improve patient engagement in treatment and perinatal outcomes. The purpose of this evaluation was to measure rates of screening for and identification of behavioral health challenges, access to and engagement in behavioral health treatment, and short-term outcomes (breastfeeding and birthweight) with known association to long-term outcomes and compare them with nationally reported rates. In this manuscript, we describe the specific telepsychiatry-enabled integrated care model and include process and outcome data from a 14-month implementation.
Methods
Partners and Clinic Sites
This project was funded by a local private foundation; it was collaboratively implemented by a Colorado-based accountable care organization and health plan (primarily serving Medicaid and Children’s Health Insurance Program recipients), its telehealth subsidiary organization, and an urban outpatient women’s clinic within a large hospital system. In 2015, before the project started, 54% of the clinic’s patients had Medicaid benefits, 23% were uninsured, and 11% had a commercial payer source. The project began with significant practice transformation and implementation work, which is a critical component of effective clinical workflow changes.
Telepsychiatry-Supported Model of Integrated Care
The telepsychiatry-enabled model of perinatal integrated care consisted of three components: universal depression screening, a virtually embedded behavioral health clinician (BHC), and virtual integration of telepsychiatry services into a collaborative care model. Before this project started, the clinic administered the Edinburgh Postnatal Depression Scale (EPDS) at a postnatal appointment for all patients and the two-question Patient Health Questionnaire (PHQ-2) at all other perinatal visits. The nine-question PHQ (PHQ-9) was used to follow up on elevated PHQ-2 results and psychological or social concerns expressed by the patient or provider. There is literature support for using both the PHQ and the EPDS to screen for depression in the perinatal population (
23,
24). Patients completed the PHQ electronically on tablet computers provided by the clinic, making the results immediately electronically available.
A full-time, licensed BHC was virtually embedded into the clinic via video conferencing to oversee the screening of all perinatal patients (including training and periodically reminding providers to ask patients about behavioral health), follow up on positive screens and other referrals, support coordination of virtual psychiatric consultation, provide brief intervention and treatment as needed, and refer and coordinate ongoing behavioral health and social services. To foster team building and new clinical workflow implementation, the BHC primarily worked onsite for the first 2 months until transitioning to full-time virtual work via video conference.
The perinatal model was implemented by using an evidence-based collaborative care model in primary care. The BHC served as the coordinator across the care team. She consulted with patients and physicians, in this case OB-GYN providers, and served as a bridge to a program psychiatrist. The psychiatrist was available via telehealth for 8 hours of consultation per month. In keeping with the model, the psychiatrist did not provide direct patient care but instead consulted with the care team via the BHC to make diagnostic and medication-related recommendations for the care team to implement. The OB-GYN provider retained prescriptive responsibility and, through the consultative model, improved her or his own ability to manage the physical and behavioral health of current and future patients.
Data Collection
Data for this project were collected as part of standard quality improvement (QI) processes for this project. The University of Colorado Institutional Review Board reviewed the project and confirmed that it met QI criteria. We collected patient-level structure, process, and outcome measures as well as system-level process measures using mixed methods. The results summarized 14 months of data collected between June 2017 and September 2018. System-level data were collected qualitatively and included descriptions of protocol development and iterations as well as team members’ experiences. Patient-level structural measures included demographic and clinical variables collected from the subset of patients who were referred to the BHC. Process measures included the number and type of services rendered, and outcome measures included depression screening scores, psychiatric encounter outcomes, intermediary metrics related to patient treatment engagement known to be associated with positive perinatal outcomes, patient satisfaction, and emergency department or hospital utilization. Standard clinic data (i.e., demographic characteristics and diagnoses) were extracted from electronic health records; remaining data were tracked by the BHC (
Box 1).
Data Analysis
Descriptive analyses were completed regularly for QI, specifically, to guide clinic process modifications to increase patients served and improve service quality and efficiency. Satisfaction surveys were distributed to a convenience sample of patients in September 2017 and July 2018. Biannual reports were produced for the funder to include summarized quantitative data and qualitative themes. We conducted statistical analyses using Microsoft Excel and IBM SPSS Statistics, version 25.
Results
For the full list of project metrics, see
Box 1.
Patient Characteristics
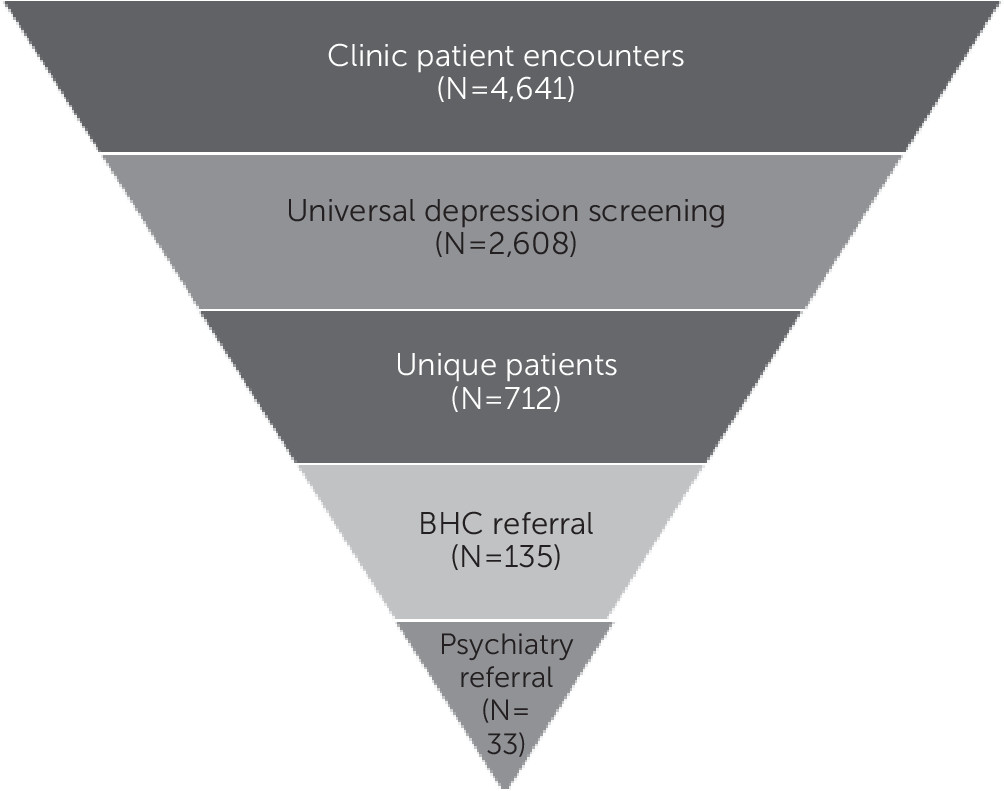
Across 14 months, the clinic served 712 unique patients, who had a total of 4,641 clinic visits. All patients (100%) completed a depression screening during at least one encounter (see
online supplement). In total, 2,608 depression screens were administered, and 135 patients (19%) were referred for behavioral health services for elevated depression screening scores or other psychosocial concern (
Figure 1). Of the 135 referred patients, 85 (63%) were Hispanic-Latina, 26 (19%) were white, 18 (13%) were black, three (2%) were Asian, and three (2%) reported unknown race-ethnicity or declined to answer. Patient ages ranged from 16 to 43, with a mean age of 29.6. There was a median of one child per household (range 0–11) and, most frequently, two caregivers in the household. Of the patients, 24% (N=33) were working full time, 44% (N=59) were unemployed, and almost one-third (N=43) did not provide employment information.
Patients came from 50 unique zip codes in the Denver metro area. Most patients (80%, N=570) were insured by Medicaid. Of the 135 patients referred for behavioral health services, 96 (71%) had a behavioral health diagnosis recorded in the electronic health record at the time of referral. The top diagnoses were depression (N=34 patients) adjustment disorder (N=31), and anxiety (N=16). Many had more than one diagnosis. Fifty-four of the 96 (56%) had one or more mood-related disorders, including anxiety, depression, dysthymia, and bipolar. Eleven (11%) had comorbid substance use disorders documented. Ninety-two (68%) of the 135 patients referred for behavioral health services had a primary general medical diagnosis, including diabetes, obesity, and asthma as well as pregnancy-related complications.
Process Measures
Of the 135 patients referred to program services, 130 (96%) engaged in behavioral health treatment. The BHC made 834 contacts, or contact attempts, to patients, including in-person (only during initial program months), virtual, phone, and voice mails (10% of contacts were no answer, no voicemail). The BHC also made 508 calls or contacts to social and community support agencies to make or follow up on psychosocial referrals. There were an average of six contacts with the BHC and four referral calls per patient. Through evidence-based practices, including assessment, brief treatment, and ongoing contact with the BHC, 117 patients were referred to (in order of frequency) therapy or counseling, support groups, psychiatry, and Colorado’s Nurse-Family Partnership. Data on patient follow-through on referrals were unavailable.
Thirty-three of the 135 patient cases (24%) required psychiatric consultation. Most psychiatric consultations (N=61, 87%) were provider-to-provider (collaborative consultations between the psychiatrist and the BHC). Most frequently, they met once per patient (range 0–7) for a total of 70 psychiatric consultation sessions. Sessions were 30 minutes, on average (range 15–90 minutes). Of the 70 consultation sessions, a majority (N=49, 70%) of sessions involved a medication-related question, and 14 (20%) included diagnostic clarification. Most consultations were regarding patients with one diagnosis before consultation (N=45, 64%). Before consultation, the most common diagnosis was depression (N=38, 54%), followed by anxiety (N=25, 36%), bipolar disorder (N=12, 17%), and posttraumatic stress disorder (N=5, 7%). Two patients had substance use disorders, two had personality disorders, and eight had unspecified diagnoses. Many patients had two or more comorbid diagnoses.
Outcomes
Patients referred to the program were more likely to present with clinically significant PHQ-9 depression symptoms at initial screening (24%, N=14 of the 58 with an initial PHQ-9) than the rest of the patients at the women’s clinic (5%, N=17 of the 339 with a PHQ-9 score) (χ2=48.72, df=1, p<0.001). Additionally, the patients referred to the program more frequently scored in the moderate to severe range of the EPDS (36%, N=32 of the 90 with initial EPDS scores), whereas only 6% (N=27 of the 445 with EPDS scores) of the nonreferred patients fell into the possible or high-risk categories of the EPDS (χ2=92.38, df=1, p<0.001). Per evaluation design, depression scores would be collected regularly from patients for the duration of their perinatal period to measure depression changes over time. However, patients varied in terms of when they initiated services at the clinic and at what point they were referred to the program, including after delivery. Because of this variation, scores did not fall cleanly into a pre-post service pattern and were not analyzed from this perspective.
At the time of report, 76 of the patients served by the integrated care program were eligible for delivery services. Of those patients, 59 (78%) had delivered at the clinic, making delivery-outcome data available. Fifty-one of 59 patients (86%) delivered full-term babies, and 56 of 59 (95%) began breastfeeding at delivery. At delivery, 58 patients had documented family-planning strategies, one patient did not, and the remaining 16 had missing family-planning information in their health records. Nine of the 59 babies were born at a low birth weight (<2,500 grams or 5 pounds 8 ounces) (
25). Excluding two sets of twins, the group receiving behavioral health services through the program had a low birth weight rate of 12%. At the time of report, 42 had returned for their 6-week postnatal visit, and 33 of the 39 (85%) who were able to breastfeed were still breastfeeding.
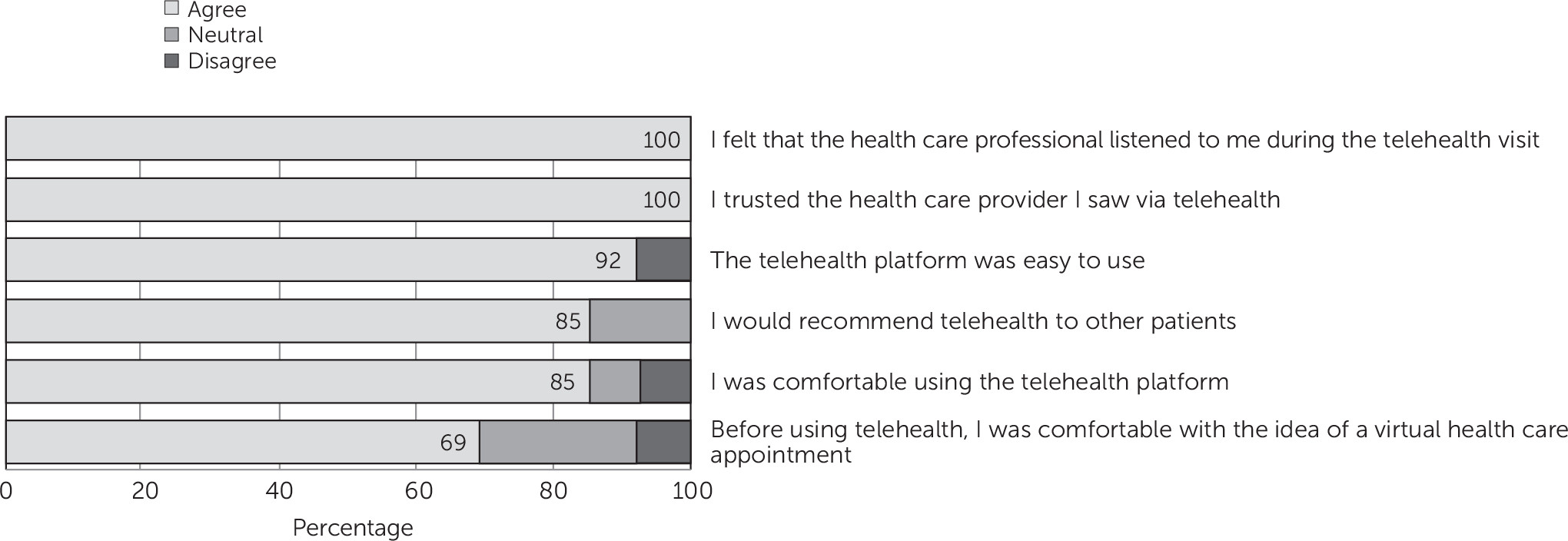
Sixteen patients completed satisfaction surveys, providing feedback on their experiences with both the behavioral health services and telehealth technology. Most patients had good experiences and would recommend telehealth to other patients (
Figure 2). There were 38 recorded emergency department visits: none for behavioral health issues and most for pregnancy-related complications. There were 55 hospitalizations (for 35 unduplicated patients) for the cohort, and only one was for behavioral health issues.
Discussion
The results demonstrated that a telepsychiatry-supported intervention for perinatal integrated care was successfully implemented in a women’s clinic serving an at-risk, socioeconomically disadvantaged population. Approximately 19% of patients screened were identified as having depression or other behavioral health needs; at least 96% of those patients engaged in at least some form of behavioral health treatment (
Figure 1). Although there was no treatment-as-usual comparison group included in the evaluation design, national estimates have cited a similar rate of prevalence but a typical treatment engagement rate of only 60% (
3), lending literature-backed support to interpretations of success.
Although all 135 of the patients who were referred to behavioral health had identified depression or other behavioral health needs, few were identified via a positive depression screen. Qualitatively, the behavioral health team observed that systematic screening improved the identification of behavioral health needs but not in the manner anticipated. Although the screening did not identify all patients in need, having universal screening as a standard of care increased the obstetrical providers’ comfort in asking patients about behavioral health issues, which did increase. Providers reported that the screening process helped normalize depression and behavioral health as a topic, and the ready presence of the behavioral health program increased providers’ confidence in their ability to address and manage behavioral health symptoms in the OB-GYN setting.
Although the evaluation lacked a comparative sample, published metrics provide some context for the program’s results. On the basis of the literature-reported 15%–20% prevalence rate of depression among perinatal populations, a 15% screening rate for perinatal and postpartum depression, and a 60% treatment rate for those identified, it can be calculated that out of 100 women, 15 would be screened, three would have a positive screen, and two of those three would receive treatment. This estimate represents only 13% of the actual population (N=15 in this scenario) with perinatal and postpartum depression (
3). Although the literature-reported depression prevalence is consistent with the measured 19% of our sample, universal screening (for a population of 712 unique patients) allowed this model to identify 100%, not just 15%, of patients in need. Of those identified, 96% then engaged in treatment, far surpassing the most generous national estimate of 60% treatment engagement (see
online supplement).
Untreated perinatal depression is associated with higher rates of low birth weight, which, in turn, is associated with higher rates of postnatal depression for the mother and a range of developmental challenges for the infant (
25,
26). Nationally, 8% of infants are born at a low birth weight (<2,500 g) (
25), and the odds of low birth weight are almost three times higher among mothers with depression (estimated odds ratio=2.94)(
27). In our sample, 12% (N=7) of nontwin infants were born at low birth weight, a positive trend given three-time greater odds for low birth rate for women with depression.
Other outcomes without comparative benchmarks include breastfeeding and behavioral health–related emergency room use. Breastfeeding is a particularly important metric for women at risk of depression. There is evidence demonstrating a bidirectional relationship such that depression is associated with lower rates of breastfeeding, and breastfeeding may protect against postpartum depression and support recovery from symptoms (
28). Among the 39 patients in this cohort who attended their 6-week postnatal visit by project end date and who were eligible to breastfeed, rates of breastfeeding were very high (N=33, 85%). Similarly, although people with behavioral health diagnoses have higher emergency department utilization than those without (
29), there was only one recorded emergency department visit for behavioral health reasons in our sample (<1%).
Limitations of this project included the absence of a controlled comparison group, no outcome measuring symptom change related to intervention, and sample attrition leading to low rates of 6-week postnatal appointment attendance and metrics. The indices of implementation success and patient treatment engagement, however, were all positive.
Conclusions
To our knowledge, this is the first evaluation of a telepsychiatry-enabled service providing perinatal integrated care. Despite evaluation limitations, the results indicated that, as hypothesized, the program was associated with improved screening and diagnosis of perinatal behavioral health issues, increased access to treatment and patient engagement, and improved patient outcomes. These preliminary observations point to telepsychiatry as a potentially effective tool for expanding models of perinatal-integrated care and lay the foundation for further study and model refinement. They also add to the growing body of evidence for the use of telepsychiatry-supported integrated care across clinical settings and patient populations.