Clinician turnover is a concern for health care organizations, particularly community behavioral health settings. Annual turnover rates for behavioral health treatment providers in the United States generally hover around 30%−35% (
1–
4), although some single-site reports indicate higher rates (e.g., 49% [
5,
6]) or lower rates (e.g., 18% [
7]). Although turnover can sometimes bring benefits—for example, allowing organizations to attract clinicians who are more aligned with evidence-based practices (
4,
8)—turnover can lead to organizational costs, particularly in recruitment and training (
9), and can erode a treatment team’s cohesiveness (
8,
10). Turnover may make it difficult for behavioral health organizations to maintain adequate program staffing, thus increasing the potential for disrupted care (
8).
Limited studies have examined the impact of turnover on quality of care in behavioral health settings, and extant studies have found that the impact of turnover on client outcomes is mixed. One small study in a psychiatric inpatient unit found that longer periods without clinician turnover were associated with decreased overall client psychological distress (
11). In a study of programs for adolescent substance abuse, Garner and colleagues (
4) found that agency-level clinician turnover was not significantly associated with outcomes, such as severity of substance abuse problems or days of using substances. However, sites with higher turnover showed greater decreases in illegal activity by clients. Researchers theorized that turnover may have provided an opportunity for “realignment” of the team (e.g., hiring more qualified clinicians), potentially improving the provision of evidence-based practices (
4). Later, the same researchers examined the relationship between clinician turnover and adolescent substance abuse treatment outcomes, this time distinguishing direct turnover (the clinician who treated the client) from indirect turnover (a clinician who served on the same team but did not treat the client). When the analysis controlled for characteristics that have also been associated with treatment outcome, none of the outcome measures (e.g., severity of substance abuse) were affected by direct or indirect turnover (
12).
Although we are aware of only three studies that have assessed the relationship between clinician turnover and client outcomes in behavioral health (
4,
12,
13), several have examined the relationship between turnover and client outcome in other health care settings. North and colleagues (
10) found that nursing units with higher turnover required more temporary cover from outside nursing staff. Temporary cover was associated with increased client falls and medication errors. Other research suggests that high turnover impairs work group learning on nursing units, which may be associated with increased medication errors (
13). Similarly, increased nurse turnover has been found to be associated with more incidents of physical restraint of patients and an increased likelihood for the facility to be cited for deficiency (
14). In addition, turnover of primary care providers has been shown to be associated with decreased patient satisfaction and reduction in preventive service use (
15), and turnover of clinicians treating patients with chronic pain has been shown to be associated with patients’ lower self-efficacy and physical functioning (
16).
This study aimed to add to the scant literature examining the impact of clinician turnover on client outcomes in behavioral health settings. Given prior research linking turnover with poor implementation of evidence-based practices (
8,
17), it is likely that turnover is similarly linked with poor client-level outcomes. One weakness of the extant literature is that turnover is often measured at the organizational or unit level, potentially diffusing the strength of impact on individual clients. Turnover of specific clinicians—those who work directly with the client most often—could have a stronger impact on client outcomes. This study examined the relationship between turnover of specific clinicians and their clients’ behavioral health outcomes over 12 months. Given the theoretical negative impact that turnover has on therapeutic processes and some supporting prior research, we hypothesized that clinician turnover would be associated with negative client outcomes. These findings could help behavioral health administrators better understand potential impacts of turnover beyond the known concerns with costs and care quality.
Methods
This study was part of a larger comparative-effectiveness trial to address well-being and client-centered care among behavioral health providers, and the methods have been described more fully in a previous publication (
18). We collected data on clinician retention and client outcomes between March 2014 and April 2016. Our university’s institutional review board approved the study. All participants gave written informed consent.
Setting
This study took place at two community behavioral health centers that provide similar services. The first serves several rural counties in a midwestern state (rural site) and employs approximately 230 staff serving approximately 6,000 clients annually. The second site is in an urban area of a different midwestern state (urban site) and employs approximately 260 staff serving approximately 4,000 clients annually.
Participants
Participants included clinicians providing direct care to clients (e.g., psychiatrists, nurses, counselors, and case managers) and clients from each organization. For the parent study, we first recruited clinicians who were engaged in direct service with adult clients and interested in participating in the study interventions; 192 completed baseline measures (
18). While we recruited clinicians, we consulted electronic medical records to identify adult clients (ages ≥18) served by each participating clinician during the previous month and used a random-number generator to select a subsample of up to five clients of each participating clinician to recruit. Clients who declined participation were replaced by the next randomly selected client on the list until researchers exhausted the list of active adult clients. We enrolled 470 clients (an additional 138 declined). All participation was voluntary, and participants received a modest incentive for participation ($10 gift card for each clinician survey completed at baseline and at 3, 6, and 12 months, and $20 for client interviews conducted at baseline and at 6 and 12 months).
Linking Clients and Clinicians
Because clients in community behavioral health settings frequently see multiple clinicians (e.g., psychiatrist and case manager), we asked clients to identify the person they see most often; if this clinician was participating in the study, we examined agency records to identify whether that clinician stayed or left during the 12-month period. Some clients did not identify a clinician whom they saw most often or they identified a clinician who was not participating in the study. Of the 470 clients and 192 clinicians enrolled, we were able to link 328 clients to 121 clinicians seen most often.
Measures
Clinician measures.
Clinician turnover was extracted from agency records at 6 and 12 months. Human-resource representatives at each organization reviewed the data to confirm whether enrolled clinicians were still employed, transferred to another position, or left their organization. Agency records contained the date of leaving or transfer as well as a brief reason for leaving (e.g., retired or terminated).
Client measures.
Client outcomes (symptoms of depression and anxiety, functioning, and client activation) were all assessed with widely used measures. Depression was measured with the nine-item Patient Health Questionnaire (
19,
20), which had strong internal consistency (α=0.85) in our sample. Anxiety was measured with the seven-item Generalized Anxiety scale (
21,
22), which also demonstrated high internal consistency (α=0.91) in our sample. Mental and physical health functioning were measured with the physical and mental health summary scores from the 12-item Short Form Health Survey, which demonstrated good test-retest reliability (0.89) (
23–
27) and internal consistency (physical health summary score, α=0.79; mental health summary score, α=0.69 in our sample) in our sample. Patient activation was measured with the Patient Activation Measure–Mental Health (
28–
30), which has strong test-retest reliability and demonstrated high internal consistency in our sample (α=0.85). Other client variables were age, sex, race, diagnosis, and client-clinician familiarity, measured by the number of months that the client reported knowing the clinician at baseline.
Data Analysis
We conducted t tests and chi-square tests to identify any baseline differences in client outcomes and other characteristics between clients whose nominated clinician stayed or left the job during the 12-month observation period. For each outcome, latent linear growth curve modeling was used to analyze the change process captured by a latent intercept and a latent slope variable (
31). We coded time as 0 for baseline, 1 for 6 months, and 2 for 12 months in the models. To assess our hypothesis that clinician turnover would be associated with more negative client outcomes, we included a binary predictor named clinician turnover for the latent intercept and slope. Clinician turnover indicated whether a client experienced turnover of the clinician that he or she saw most often during the 12-month observation period (1, yes; 2, no). For this study, we were interested in the turnover effect on the slope of each outcome, which captured the change in outcome after each 6-month interval.
We controlled for a few baseline measures (covariates) in the growth curve model for each outcome to rule out the possibility that a significant association between clinician turnover and the slope of the outcome, if detected, was the result of a preexisting difference in the covariates between the clients who experienced clinician turnover and those who did not. These covariates included the baseline status for each outcome measure, client age, client-clinician familiarity, sex (0, female; 1, male), and site (0, rural site; 1, urban site). Initially, we also considered race as a covariate. However, given that 95% of the clients at the rural site were white, the effects of site and race were highly conflated. Thus we excluded race from the analyses. Because client-clinician familiarity was highly skewed, we normalized that variable using log transformation.
To examine whether the effect of clinician turnover was moderated by any of the covariates, we also included the interaction terms between each of the covariates and clinician turnover in the model. When a significant interaction effect was identified, we probed the interaction by plotting the turnover effect (and 95% confidence intervals) against a range (±2 SD) of values on the corresponding moderator. The effect, given a specific level of the moderator, was significant if the corresponding confidence interval did not cover 0. All continuous covariates were mean-centered. Analyses were conducted in Mplus 8.0 (
32). Because clients were nested under clinicians, we used the “Type=complex” command with robust maximum likelihood estimation method (MLR) in Mplus to obtain the correct standard errors accounting for the clustering effect. MLR is also an appropriate method to handle missing data (
33).
Results
Descriptive statistics for variables included in the analyses are shown in
Table 1, by clinician turnover status. [A table in an
online supplement to this article presents descriptive statistics by site.] Of the 121 participating clinicians identified as most frequently seen, 31 (26%) left their position during the 12-month period; 15 were from the rural site, and 16 were from the urban site. Turnover rates were roughly equal across sites. Most of the 31 clinicians who left (N=22, 71%) were either case managers or therapists. Of clinicians who left, 26 (84%) resigned, four (13%) were terminated, and one (3%) retired.
Of the 328 participating clients, 78 (24%) experienced clinician turnover—51 (65%) during the first 6 months of the monitoring period and 27 (35%) during the second 6 months. At baseline, clients who later experienced clinician turnover had higher mental health functioning, greater patient activation, and lower depression and anxiety, compared with clients who did not later experience clinician turnover (N=250, 76%).
Given the purposes of this study, we report the main and interaction effects from the growth curve models for the slope of the five outcomes. Clinician turnover showed significant effects relevant to all outcomes, except depression (
Tables 2 and
3). The results for the other four outcomes are described below.
Anxiety
As shown in
Table 2, the main effect of turnover on clients’ change in anxiety was moderated by the baseline status on the anxiety measure (
B=–0.16, p=0.01), when other factors were held constant. Our probe of the interaction suggested a significant positive effect of turnover on the slope of anxiety for clients with low or moderate anxiety, indicating that clinician turnover was associated with increased anxiety over time for these clients [see figure in
online supplement].
Patient Activation
The turnover effect on the change in patient activation was also moderated by the baseline status on the measure (
B=–0.29, p<.01), when other factors were held constant (
Table 2). Our probe of the interaction suggested that the turnover effect changed from positive to negative as baseline patient activation increased. The effect was significantly negative only for clients with relatively high baseline patient activation [see figure in
online supplement].
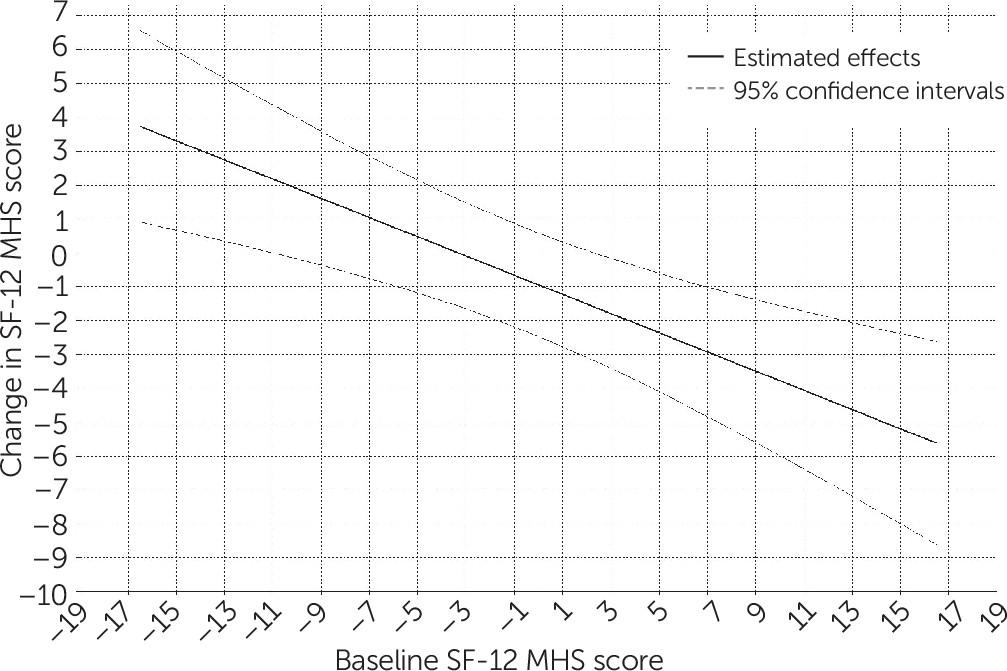
Mental Health Functioning
The turnover effect on the slope of mental health functioning was moderated by baseline mental health functioning (
B=–0.32, p<0.01), when other factors were held constant (
Table 3). The turnover effect on mental health functioning changed from positive to negative as baseline mental health functioning increased (
Figure 1). Although it appeared that turnover was associated with declines for clients with relatively high baseline mental health functioning, turnover was associated with significantly increased mental health functioning over time for clients with relatively poor baseline mental health functioning.
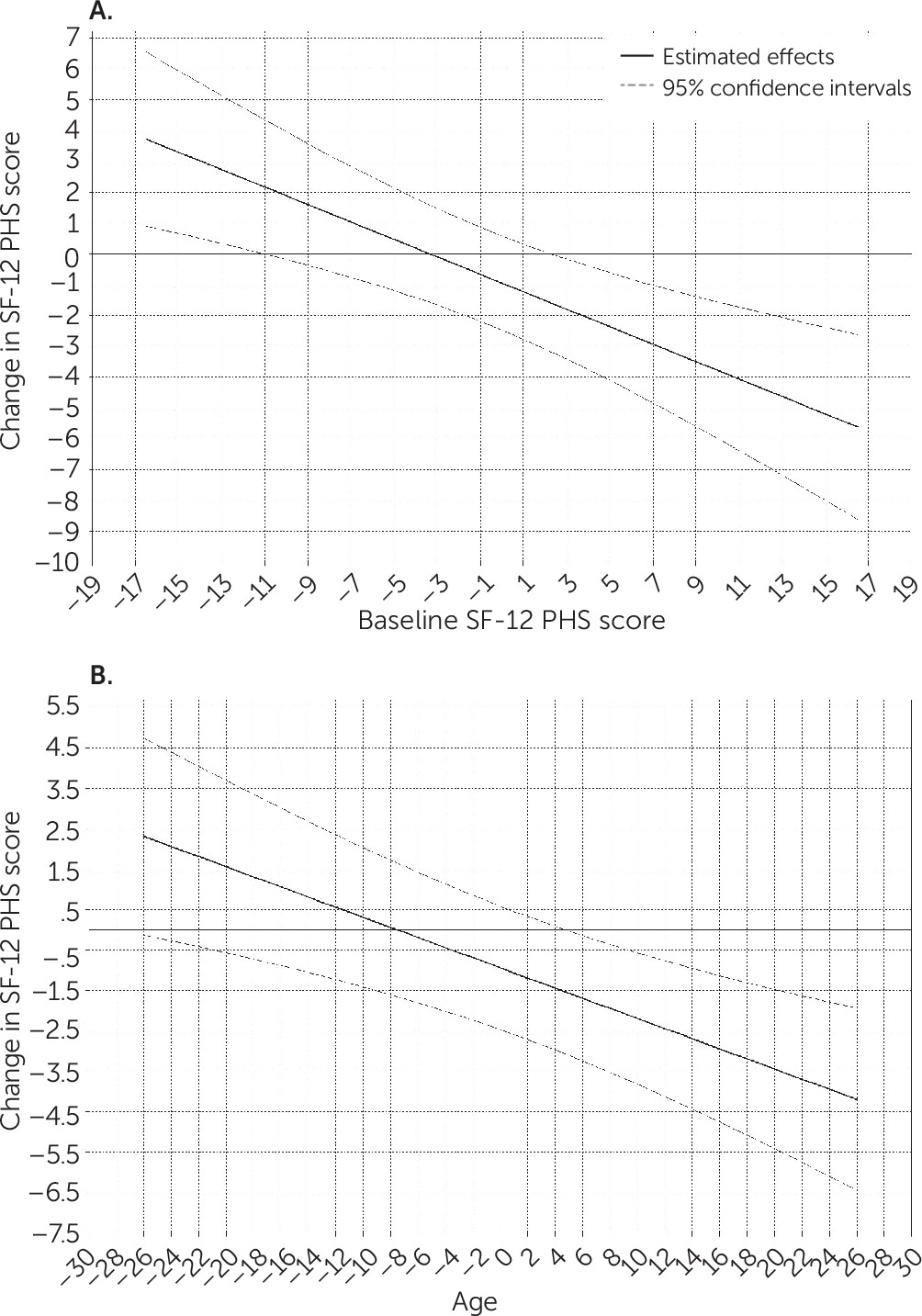
Physical Health Functioning
The model for physical health functioning suggests that the turnover effect on the slope of physical health functioning was moderated by baseline physical health functioning (
B=–0.32, p<0.01) and age (
B=–0.13, p<0.01), when other factors were held constant (
Table 3). As shown in
Figure 2, the turnover effect on physical health functioning decreased from positive to negative as baseline physical health functioning increased or age increased, indicating that turnover was associated with decreased physical health functioning over time for clients with relatively high physical health functioning at baseline or who were older.
Discussion
This study examined the relationship between clinician turnover and client outcomes in community behavioral health settings. In our sample of 121 clinicians, 26% left their position during the course of the study, consistent with other research indicating approximately 30% annual turnover of community behavioral health clinicians (
4). Turnover creates significant concerns in behavioral health organizations (e.g., financial costs in recruiting and training and expertise loss). Researchers and administrators frequently presume that clinician turnover has a detrimental impact on clients, theorizing that losing a positive relationship and transitioning to a new clinician represents a significant disruption in care. However, few studies have directly assessed clinician turnover and client outcomes, particularly in community behavioral health settings.
Our primary finding suggests that clinician turnover was associated with the most detrimental outcomes for clients doing well at the beginning of the observation period, but turnover was not uniformly associated with negative outcomes. For both physical and mental health functioning, clinician turnover was related to negative outcomes for clients with relatively higher baseline functioning. Similarly, negative associations with turnover were seen for clients whose baseline patient activation was higher and for clients who had low or moderate baseline anxiety symptoms. Turnover had no significant relationship with depression. Curiously, we also found that turnover was associated with no changes or positive changes for clients who experienced more difficulties at baseline. Turnover was associated with significant increases in mental health functioning over time for clients with relatively poor baseline mental health functioning. Clinician turnover was not related to significant change in anxiety for clients with high baseline anxiety and was also unrelated to significant change in physical health functioning for clients with low baseline physical health functioning. An important secondary finding was that for physical health functioning, the relationship with turnover was moderated by age. Specifically, clinician turnover was associated with a stronger negative effect on functioning for older clients. Thus, for those who are younger, turnover may affect functioning less, possibly because their physical health may be more resilient in the face of disruptions in care.
Although prior research on the impact of clinician turnover on behavioral health outcomes is limited, the findings have been similarly mixed (
4,
12,
13). Previous studies have primarily examined turnover at the team or organizational level. Our study builds on and is consistent with work by Garner and colleagues (
12) by directly linking clinicians with the clients that they personally treated. Our results suggest that clinician turnover is not exclusively associated with clinical decline and may have more complex relationships with outcomes than found in prior studies. In particular, turnover may be more detrimental for clients who are doing well (i.e., have high baseline mental health functioning) and have more clinical gains to lose.
It is important to note that clients with similarly high baseline mental health functioning who did not experience clinician turnover did not experience a similar increase in symptoms during the course of the study. This argues against the idea that effects reflect regression to the mean. We could speculate on the counterintuitive finding that turnover appeared beneficial for clients with low mental health functioning; for example, starting over with a different clinician who forms a stronger alliance or better implements evidence-based practices might be helpful. However, we did not have that level of detail in our data. Future work is needed to identify the mechanisms of improvement or reductions in client outcomes following clinician turnover.
This study had limitations. The two sites differed significantly in the racial demographic characteristics of clients and clinicians (i.e., race was conflated with site); therefore, we could not include both race and site as a covariate or potential moderator. The study was also limited by focusing on the clinician who was nominated by the client at baseline as the person seen most often; the importance of that person to the client or the amount of time spent with the clinician may have changed over time. Because of statistical power concerns, we assessed turnover at any time during the 12-month period, but the timing of the turnover may have a differential impact (e.g., recent loss versus a loss the client has had time to adjust to). Future research with larger samples of clinicians should include timing of turnover as a moderating variable. Similarly, we were unable to examine how the organizations responded to turnover. For example, turnover on teams that share caseloads may be less problematic than turnover of clinicians who have individual caseloads (
34), because team members who already have relationships with clients might ease the transition.
Conclusions
The findings of this study suggest that clinician turnover may have differential impacts on clients depending on clients’ initial levels of functioning and symptoms and may be particularly detrimental for those who are older and have better functioning and fewer symptoms. Clients who are doing better may have more to lose when clinicians leave. Future work is needed to identify how to best serve clients experiencing turnover to reduce these observed impacts.