Personal recovery refers to changes in one’s attitude to life and illness, with emphasis on hope and the establishment of a meaningful life (
1–3). Connectedness, hope, identity, meaning and purpose, and empowerment have been identified as key themes in the personal recovery concept—and have provided the acronym CHIME (
4). Personal recovery has been contrasted with clinical recovery, where symptom reduction and increased functioning are the main treatment focus (
2).
There has been debate over the relationship between personal recovery and the traditional clinical recovery goal of reduced symptomatology and improved functioning (
5). This has important clinical implications. Some studies have shown that people with psychosis can participate in working toward personal recovery regardless of their clinical and functional competence (
6), whereas others have shown that service users with more clinical symptoms and a lower functioning level prefer clinical recovery goals, such as reducing symptoms and confusion (
7). Some have argued that personal recovery is more of a self-realization concept, in accordance with Maslow’s pyramid (
8,
9), and that for some service users, more basic needs must be met before self-realization can occur (
10,
11). Because CHIME is widely endorsed in the recovery literature (
12), more knowledge about the applicability of the framework is needed. An important step toward increased knowledge is to clarify whether personal recovery, as conceptualized by the CHIME framework, is considered relevant to most people with psychosis. A better understanding of this issue can help inform mental health services and the development of recovery-oriented practices. A few studies have used qualitative data to investigate the applicability of the CHIME framework, and results have supported the category structure (
13,
14) but have also suggested an expanded conceptualization of recovery, in which experienced difficulties are more prominent (
14). However, no studies have quantitatively examined the applicability of the framework.
Support of and focus on personal recovery have become increasingly important aspects of mental health services in many countries (
5,
15). Lately, several recovery-oriented interventions have been developed and implemented in mental health systems internationally (
16). For example, Illness Management and Recovery (IMR) treatment (
17) aims to improve the ability of individuals with severe mental illness to better manage their illness in areas such as symptomatology, functioning, knowledge, progress toward goals, and hope (
18,
19). However, one of the biggest obstacles to the implementation of recovery-oriented practices is the lack of knowledge about how recovery can be best supported (
20). More knowledge about factors associated with perceived support for personal recovery is important for improving treatment and health service development and bridging the gap between the personal recovery vision and clinical practice.
This cross-sectional study aimed to answer the following research questions: Is personal recovery as defined by the CHIME framework considered important for service users with psychosis? Are there any differences between service users with different levels of rated importance? How much perceived support for personal recovery do the service users receive? And what covariates are associated with perceived support?
Methods
Design
The study had a cross-sectional design, with baseline data from a Norwegian research project—a randomized trial of implementation of the Norwegian national clinical guidelines for treatment of psychosis (ClinicalTrials NCT03271242: “A pairwise randomized study on implementation of guidelines and evidence based treatments of psychoses”). The study was approved by the Regional Committee for Medical and Health Research Ethics (REK Sørøst B 2015/2169), following the principles in the Declaration of Helsinki.
Sample and Setting
Inclusion criteria were mental health service user, age ≥16, and
ICD-10 diagnosis of psychosis (F20–29) (
21). Exclusion criteria were an inability to understand and answer the questionnaires in Norwegian. A total of 325 service users participated in the project. Service users (N=4) with missing data on the INSPIRE measure were excluded from analysis in this study. A total of 39 clinical units and hospital departments with outpatient clinics, day units, mobile teams, and inpatient wards from six health authorities across Norway participated, including three university hospitals.
Measures
Service user–rated measures.
The INSPIRE Measure of Staff Support for Personal Recovery was used to examine the importance of personal recovery and to assess experienced support from a mental health clinician. The INSPIRE is a 27-item self-report questionnaire that measures perceived staff support for personal recovery (
22). It consists of two subscales: support (20 items) and relationship (7 items). The relationship subscale was not completed in this study. The support items cover five domains: connectedness, hope, identity, meaning and purpose, and empowerment, which were identified through a systematic review and given the acronym CHIME (
4). Participants first rate each support item for whether they consider it important for their recovery (e.g., “An important part of my recovery is: Feeling supported by other people”—yes or no). If yes, participants rate the extent of support they experience from their mental health clinician (“I feel supported from my worker with this”) on that item on a 5-point Likert scale (0, not at all; 1, not much; 2, somewhat; 3, quite a lot; and 4, very much).
The number of “yes-important” responses was used as the dependent variable to examine whether personal recovery was considered important and whether any differences existed between service users with different levels of rated importance. The support score was used as the dependent variable to examine perceived support for personal recovery and covariates associated with perceived support.
The Behavior and Symptom Identification Scale (BASIS-24) is a brief self-report measure of six domains of mental well-being and functioning, with good validity and reliability for assessing mental health status from a service user perspective (
23,
24). Two of the six domains were used. The depression-functioning domain was included as a measure of the level of participants’ depressive symptoms. The substance abuse domain was also included and was transformed into a dichotomous variable (substance abuse versus no substance abuse). Abuse was defined as a score of 3 (often) or 4 (always) on any of the items in the domain. Item 22 (“Did anyone talk to you about your drinking and drug use?”) was excluded because it was considered irrelevant. Subdomain scores were calculated as described in the BASIS-24 instruction guide (
25), providing a score between 0 and 4, with higher scores indicating more severe problems.
Participants’ satisfaction with life was assessed with one item from the Manchester Short Assessment of Quality of Life (MANSA) (
26). “How satisfied are you with your life as a whole?” was rated on a 7-point scale (1, couldn’t be worse; 7, couldn’t be better).
Participants also rated six statements about their overall experience with getting help to manage their lives and their illness for the past 6 months. The six statements pertaining to overall experience were named as follows. Setting goals: “I have been well trained in setting goals and working to achieve them.” Increased knowledge: “I have gained useful knowledge about stress, vulnerability, and social support.” Coping: “I have gained useful knowledge about coping with stress and illness.” Health service use: “I have gained useful knowledge about how to use health services better.” Medication: “I have gained useful knowledge about the medicines I use.” Early detection and prevention of relapse: “I have prepared a plan for the early detection of any signs of aggravation, and what should be done then.” The questions were rated on a 5-point scale (1, strongly disagree; 5, strongly agree), with an additional option of answering “not relevant.”
The participants also reported whether they had participated in IMR groups during the past 6 months (yes or no). This variable was named IMR experience.
Clinician-rated measures.
The Clinical Global Impressions Scale (CGI) was originally developed for use in National Institute of Mental Health–sponsored clinical trials (
27). This study included the CGI severity component (CGI-S), in which clinicians rate the severity of service users’ mental illness in the past 7 days on a 7-point scale (1, normal, not at all ill; 7, among the most extremely ill service users) (
28).
The Global Assessment of Functioning Scale (GAF) is a standardized assessment of impairment caused by mental factors (
29) in which clinicians rate the level of functioning and severity of service users’ symptoms on a scale from 1 to 100. Lower scores indicate more severe symptoms and lower levels of functioning. The split version of the scale used in this study has two subscales: symptom (GAF-S) and functioning (GAF-F) (
30).
First, we identified covariates on service user characteristics (age, gender, ethnicity, community treatment order status, and mental health care history), service user–rated measures (depression-functioning, satisfaction with life, and substance abuse), and clinician-rated measures (GAF-S, GAF-F, and CGI-S). These were chosen on the basis of prior research as described above and were factors that we hypothesized might affect or mediate the outcomes in the study.
Second, because of the small part of the variation explained by these variables in the regression models, we included data on health service characteristics, such as the six statements pertaining to overall experience (overall experience) and IMR experience variables, to determine whether this explained more of the outcome. We hypothesized that experience with IMR and related recovery themes (overall experience) might increase both level of importance and perceived support.
Procedures
Clinicians at participating clinical units recruited service users and performed the clinical ratings. Questionnaires were administered to service users by the secretary or other personnel at the clinics. Service users were provided a place to sit to fill out the questionnaires or took the questionnaire home with them. When the service user was finished, the questionnaire was put in an envelope, which was closed and returned to the clinic. Recruitment began in June 2016. Eligible service users already in contact with the clinic at the time and newly referred service users assessed to have psychosis were asked to participate. Recruitment continued until March 2017. Only participants who gave written informed consent were included.
Analysis
To assess the characteristics associated with number of yes-important answers and with the total support score, bivariate and multiple linear regression models were estimated. First, models with participant characteristics (age, gender, ethnicity, community treatment order status, and mental health care history), participant-rated measures (depression-functioning, satisfaction with life, and substance abuse), and clinician-rated measures (GAF-S, GAF-F, and CGI-S) were estimated. Next, covariates on service users’ overall experiences in managing their life and illness (overall experience statements) and whether they had participated in IMR (IMR experience) were added. Because participants were recruited to the study by different units, a hierarchical structure (cluster effect on unit level) could have been present in the data. Assessment by an intraclass correlation coefficient (ICC) found that there was essentially no cluster effect in outcome variables (ICC=0.001 for number of yes-important answers and ICC=0.01 for support score). Hence, no adjustment for within-unit correlations was needed. Correlation analysis did not identify any multicollinearity issues among covariates. Residual diagnostics did not show any significant deviations from linear regression model assumptions. Both bivariate and multiple models were estimated for cases with no missing values on covariates. Results with p values below 0.05 were considered statistically significant. The analyses were performed with SPSS, version 25.
Imputation of missing values on the GAF (N=40), the MANSA (N=8), and the overall experience (N=25) scales was performed by first generating the empirical distribution for each variable. A random number was drawn from that distribution and used to replace the missing value. The process was repeated until all missing values were imputed. Missing values on demographic variables were not imputed.
Results
Sample Characteristics
The characteristics of the 321 participants are shown in Table
1.
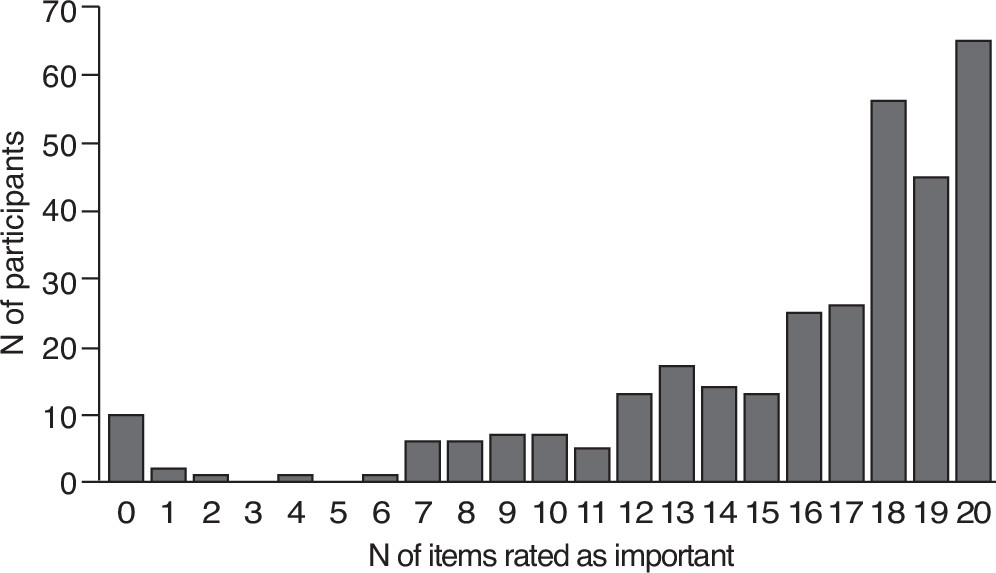
Importance of Personal Recovery
The 321 participants rated the 20 INSPIRE support items as important or not important to their recovery. The percentages who gave a rating of important to each item ranged from 66% to 91% (Table
2). Ten (3%) participants rated all 20 items as not important. A total of 167 participants (52%) gave an “important” rating to between 17 and 20 items. Figure
1 further illustrates participants’ ratings of items as important to personal recovery.
Differences Between Service Users With Different Levels of Rated Importance
A multiple linear regression model examined characteristics associated with ratings of important (Table
3). The model explained 4.8% of the total variation in the number of ratings of important. When covariates on service users’ overall experience with managing their life and illness for the past 6 months (the six statements) and information on participation in IMR groups for the past 6 months (IMR experience) were included, the model explained 8.1% of the total variation. No significant associations were found in the multiple linear regression model.
Support for Personal Recovery
Participants rated the level of support they had experienced from their mental health clinician in terms of the 20 INSPIRE support items. The ratings per item ranged from 2.27 to 2.83 (Table
2), showing that, on average, the service users reported levels of support from somewhat (rating of 2) to quite a lot (rating of 3).
A multiple linear regression model examined characteristics associated with experienced support (Table
4). The model explained 14.8% of the total variation in experienced support. When covariates on service users’ overall experience with managing their life and illness for the past 6 months (the six statements) and information on participation in IMR groups for the past 6 months (IMR experience) were included, the multiple linear regression model explained 31.1% of the total variation in experienced support. In the multiple model, lower GAF-S score, higher depression-functioning score, and male sex were significantly associated with lower levels of perceived support. Also, higher scores on the coping statement (“I have gained useful knowledge about coping with stress and illness”) and the statement about early detection and prevention of relapse (“I have prepared a plan for the early detection of any signs of aggravation, and what should be done then”) were significantly associated with higher perceived support, as was having participated in IMR groups during the past 6 months (IMR experience).
Discussion
This study showed that most service users with psychosis considered personal recovery, as operationalized with the CHIME framework, to be important. The study found no differences between service users who rated personal recovery as less important and those rating it as more important. Overall, service users experienced only moderate support for personal recovery from their mental health clinician. Higher self-reported depressive symptoms, lower GAF-S score, and male sex were significantly associated with less perceived support. Having participated in IMR groups, having gained knowledge about coping with stress and illness, and having a plan for early detection and prevention of relapse for the past 6 months were significantly associated with higher perceived support.
The main finding was that the great majority of a large, heterogeneous group of service users with psychosis across several clinical units reported that personal recovery was important to them, regardless of age, ethnicity, symptomatology, functioning, community treatment order status, and time in mental health care. This finding has implications for clinical practice, providing empirical evidence that recovery-oriented treatments are relevant for most service users with psychosis in various mental health services.
However, although the great majority of participants reported personal recovery to be of high importance, they experienced only a moderate degree of personal recovery support from their mental health clinician. Several factors can influence the level of experienced support for recovery, not the least being the degree to which various clinicians and various mental health units are recovery oriented. Our findings show that previous experience with IMR and related themes, such as knowledge about coping with stress and illness and having a plan for early detection and prevention of relapse, were significantly associated with higher perceived support. This suggests that recovery-oriented treatments such as IMR and related themes may be effective in helping people feel supported in their process of personal recovery, a result in line with a recent meta-analysis showing greater improvement in personal recovery outcomes when service users were involved in recovery-oriented mental health treatment versus usual care or other types of treatment (
31). Future research should examine perceived support and IMR treatment in relation to the different CHIME domains.
In addition, we found that higher self-reported depressive symptoms, lower GAF-S score, and male sex were significantly associated with less perceived support. This finding is of clinical importance. That is, it is important not to be blinded by high levels of general symptoms or depression, because these service users nevertheless believe that personal recovery is important. Although we cannot draw conclusions regarding causality among these associations, our results point to the importance of providing support for personal recovery, even among service users with high levels of general symptoms and depression. Future research should examine how patterns of importance ratings change over time and how perceptions of support are influenced by treatment.
Previous research has shown that affective symptoms seem to be more closely linked than psychotic symptoms to personal recovery and related themes, such as quality of life (
5,
32,
33). Our finding that a higher level of self-reported depression was related to less perceived support underlines the important notion of an association between affective symptoms and personal recovery among service users with psychosis.
A major strength of this study was the broad group of participants with psychosis and the many different units that participated, which allowed us to gain information that can be generalized to a range of mental health services for service users with psychosis. A limitation of the study was the lack of data on the representativeness of the sample. Because participants were not randomly selected, they may not accurately represent the overall Norwegian population of individuals with psychosis. Other important limitations were the cross-sectional nature of the study, which prevented conclusions regarding causality, and that interrater reliability between the GAF scales and the CGI scale was not assessed.
Conclusions
This study showed that the great majority of a large, heterogeneous group of service users with psychosis across several clinical units reported that personal recovery was important for them, regardless of age, ethnicity, symptomatology, functioning, community treatment order status, and time in mental health care. This finding has implications for clinical practice, providing empirical evidence that recovery-oriented treatments are relevant for most service users with psychosis in various mental health services. Recovery-oriented treatments such as IMR, and related themes, such as help for coping with stress and illness and having a plan for early detection and prevention of relapse, appeared to help people with psychosis feel supported by clinicians in their personal recovery process. Specific attention should be given to service users with high levels of general symptoms and depression, because these service users experienced less support for personal recovery, even though personal recovery was equally important for them.
Acknowledgments
Dr. Slade acknowledges support from the Center for Mental Health and Substance Abuse, University of South-Eastern Norway, and the Nottingham Biomedical Research Centre, National Institute for Health Research.