People with serious mental illness, including schizophrenia, schizoaffective disorder, bipolar disorder, and severe depression, make up 3%−4% of the U.S. population. They have intersecting psychological, general medical, and social vulnerabilities that place them at disproportionate risk of COVID-19 acquisition, morbidity, and mortality. People with serious mental illness historically experience one of our nation’s greatest and most underrecognized health disparities, with a reduced life expectancy of at least 10 years, which is explained in part by high rates of tobacco use and multiple chronic health conditions (
1,
2). Of direct relevance to the current pandemic, the prevalence rates of cigarette smoking, chronic obstructive pulmonary disease, cardiovascular disease, and diabetes among people with serious mental illness are each about two to three times higher than in the general population (
3), directly corresponding to age-independent risk factors associated with higher rates of COVID-19 mortality (
4).
Compounding these risks are psychological, cognitive, and socioeconomic challenges experienced by people with serious mental illness that can lead to difficulties with medication adherence, self-care, living skills, and adherence to health-related recommendations. Serious mental illness is also associated with numerous social vulnerabilities that are likely to contribute to poor COVID-19 outcomes (
5), including poverty, homelessness, poor nutrition, and difficulty accessing needed medications, as well as increased risk of viral transmission associated with residing in congregate group homes, emergency shelters, transitional housing programs, long-term care facilities, and psychiatric hospitals. At the nexus of the COVID-19 crisis for people with serious mental illness are state-supported community behavioral health organizations, which have experienced profound challenges in attempting to rapidly respond without adequate capacity, further complicated by the impact of the pandemic on the physical and mental health of the staff, and with declining revenue.
The adverse impact of COVID-19 on community-based behavioral health services is illustrated by survey results released in late March 2020 from 32 California nonprofit community behavioral health agencies (
6). One-third of the agencies indicated that they had service recipients who were too sick to engage in treatment and that they did not know whether this was a result of COVID-19 infection, a worsening of psychiatric or medical illness, or both. The vast majority of agencies (87%) reported a lack of vital equipment to adequately conduct telehealth sessions, and agencies lacked access to any personal protective equipment for frontline staff. Over half (58%) reported that they had decreased delivery of needed behavioral health services, with most (81%) experiencing reduced capacity because of staff health issues or lack of child care. Because of declines in revenue, 10% of the agencies reported that they had furloughed staff, 13% had terminated positions, and an additional one-third reported that they planned to furlough or terminate positions in the absence of financial relief.
Massachusetts Statewide COVID-19 Behavioral Health Policy Reforms
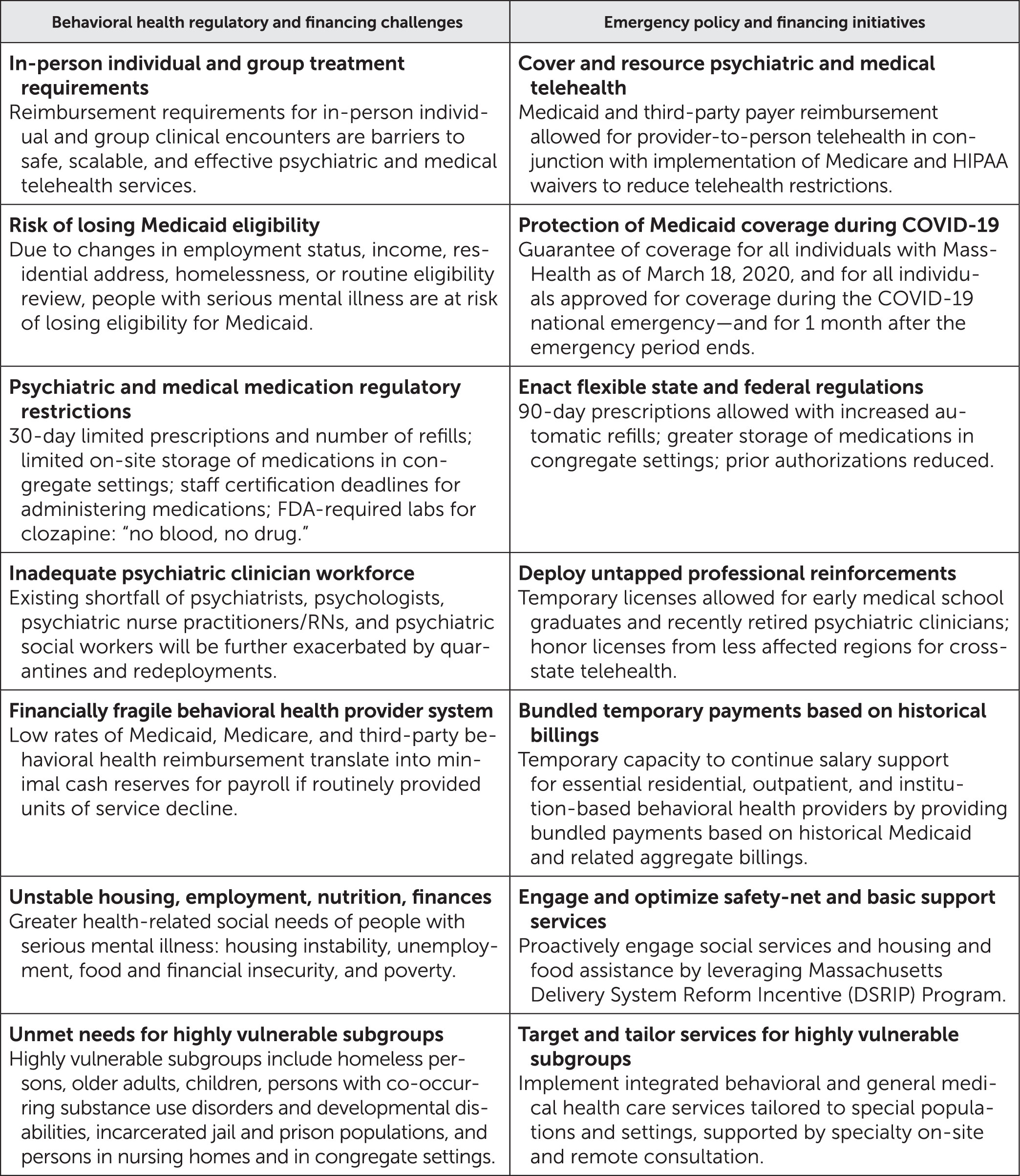
The Massachusetts Department of Mental Health provides services to approximately 30,000 people with serious mental illness annually. As the COVID-19 pandemic developed, community-based providers collaborated with the Executive Office of Health and Human Services to rapidly develop changes in guidance, regulations, and funding to provide flexibility in supporting behavioral and general medical services as the coronavirus pandemic spread (
7). In
Figure 1, we identify critical challenges and corresponding health care delivery and policy measures implemented in the State of Massachusetts as an example of a coordinated statewide response to challenges associated with the COVID-19 pandemic.
Among the most high-impact regulatory relief measures being enacted at the level of clinicians and patients are state Medicaid, third-party, and federal Medicare and HIPAA waivers allowing extensive use of provider-to-person home- and community-based telehealth assessments and treatments (
8). At the patient level, Massachusetts instituted a temporary policy preventing termination of individual-level Medicaid coverage during the national emergency. Other critical measures include allowing pharmacies to distribute larger amounts of prescribed medications and refills to individual patients, along with waivers on the amount of medication stored on site in group homes, helping to ensure an uninterrupted supply of critical psychiatric and general medical medications to patients at significant risk of relapse with the increased stress and isolation associated with the COVID-19 pandemic.
The special challenges associated with distributing clozapine, which requires in-person blood draws and labs before prescriptions can be filled (the “no blood, no drug” policy), were addressed by academic-community partnerships with input from the state. For example, Massachusetts General Hospital, McLean Hospital, and the North Suffolk Mental Health Association set up a clozapine working group to formulate guidance about how to proactively manage clozapine dispensation for the large clozapine cohort during COVID-19, consistent with national risk evaluation and mitigation guidance and an international consensus document (
9). The Massachusetts Department of Mental Health explicitly endorsed the recommendations, which removed uncertainty for clinicians and pharmacies.
Additional regulatory relief included relaxing criteria for group home staff to be recently recertified to administer medications and providing higher “combat pay” for frontline residential care workers. In an effort to provide additional physician workforce capacity, Massachusetts also approved temporary 3-month medical licenses for early-graduating medical students and recently retired physicians.
At the organization-level, an example of a critical financial lifeline enacted by Massachusetts to behavioral health providers is the provision of temporary continued distribution of a portion of historically billed Medicaid payments untethered from fee-for-service direct visits. Critical financial stabilization funds announced by Massachusetts Governor Baker and coordinated by the Executive Office of Health and Human Services included $23 million in immediate cash relief in March, followed by a commitment of $104 million, including monthly interim payments from April to July 2020 equaling 50% of providers’ historical behavioral health revenue and a 10% increase to clinical support services, acute treatment services, residential support services, children’s behavioral health services, and opioid treatment services (
7).
Focused efforts have also been aimed at helping to reduce the devastating impact of COVID-19 on the most vulnerable subgroups of people with serious mental illness, such as those who are homeless. In partnership with city and state agencies and other community stakeholders, Boston Health Care for the Homeless Program (BHCHP) rapidly deployed a comprehensive COVID-19 response strategy that included front-door symptom screening at local shelters, expedited COVID-19 testing, isolation in alternate care settings of homeless persons under investigation for COVID-19, and dedicated COVID-19 care units for individuals experiencing homelessness. Across each segment of this response, BHCHP mental health clinicians have been able to provide virtual care to patients with psychiatric and addictive disorders via telehealth-based approaches. Additional long-term support is available for basic housing and food support through the Massachusetts Medicaid Delivery System Reform Incentive Payment program and Medicaid accountable care organizations for a “flexible services program” dedicated to health-related nutrition and housing supports that will be deployed.
Conclusions
During natural disasters and states of emergency, existing inadequacies in our health care delivery system are brought into bold relief. Rapid implementation of measures at state and local levels not only may help mitigate the disproportionate morbidity, mortality, and spread of COVID-19 for people with serious mental illness but also may have substantial implications for reducing the impact of this pandemic for the broader population of vulnerable adults with complex physical, social, and psychological needs and disabilities. The State of Massachusetts represents one example of a coordinated response aimed at providing flexibility and relief at the levels of recipients of care, clinicians, staff, and organizations. Some of these transformations have accelerated previously existing trends, such as increasing the use of provider-to-patient telehealth and use of bundled capitated payment approaches. Additional measures could include leveraging mobile health and automated telehealth providing general medical and psychiatric illness self-management support and remote monitoring (
10), supplemented by automated delivery of COVID-19 patient education and symptom tracking.
At the individual level and in the critical domain of social support, family members, certified peer support specialists, and relevant federally supported state agencies could be widely engaged through the National Alliance on Mental Illness and the Substance Abuse and Mental Health Services Administration to virtually reinforce social distancing, handwashing, and stress reduction practices while helping to minimize the adverse psychological effects of social isolation, such as increased risk of depression, substance use, psychiatric relapse, and suicide. These and other adopted measures could subsequently translate to downstream reforms in how we care for these populations during more ordinary times. Once we make it through this crisis and reflect on the lessons learned in implementing these innovations and reforms, we should not waste this potentially transformative opportunity by returning to business as usual.
Acknowledgments
The authors thank Alice Oh, B.S., for her assistance in background research and editing the manuscript.