Organization and Outcomes of Integrated Inpatient Medical and Psychiatric Care Units: A Systematic Review
Abstract
Objective:
Methods:
Results:
Conclusions:
Highlights
Methods
IMPU Definition
Search Strategy
Eligibility Criteria
Data Extraction
Study Quality Assessment
Data Synthesis
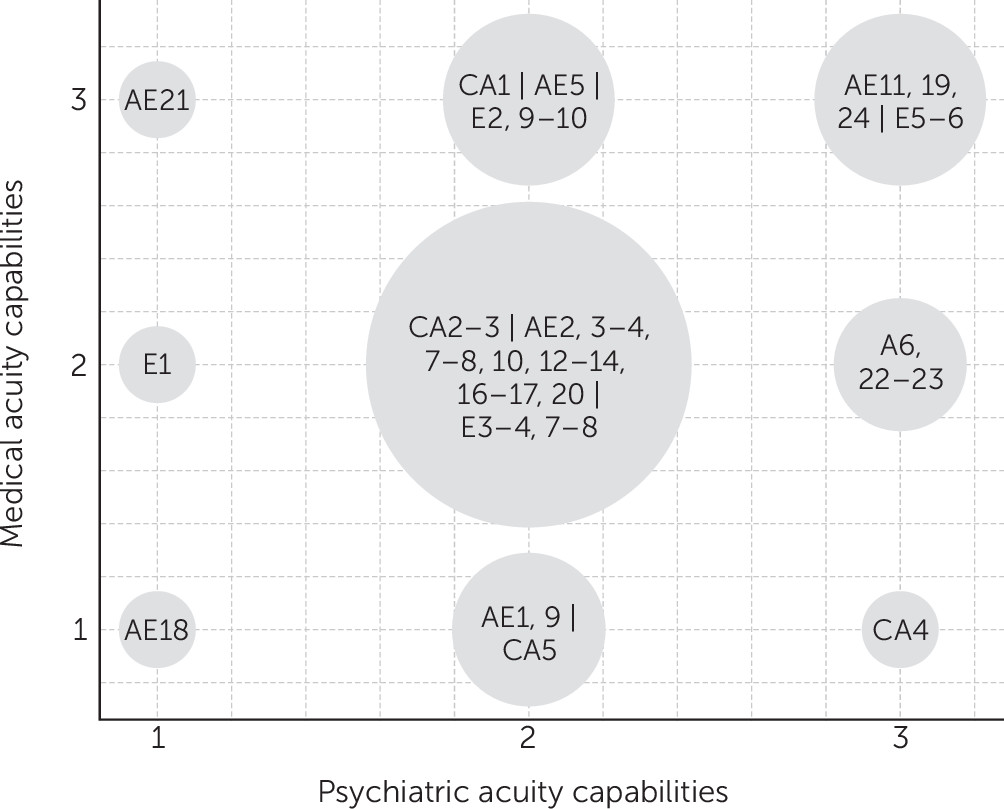
Unit Type
Acuity Capability
Main Findings
Results
| IMPU no. and referencea | Countryb | Year | Hospital typec | Unit typed | Aimse | Sizef | Patient age in years | Physiciansg | Residents | Nurses | Length of stay (LOS) in days | Acuityh | Study design, outcome, GRADEi | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | P | |||||||||||||
| CA1 (21) | US | 1976 | G/C | NSU | — | M: 19 (L, S) | Adolescence | Ped (A), psych (NR) | Not defined | Ped, cross-training | NR | 3 | 2 | NR |
| CA2 (37, 38) | US | 1991 | U/T | PMU | 3, 5 | P: 8 (O) | range 4–18 | Psych (A, MD), ped (A) | Psych and ped | Psych, cross-training | M=27 | 2 | 2 | NR |
| CA3 (41) | US | 1994 | U/T | PMU | 1 | P: 16 (L) | range 15–22 | Psych (A, MD), ped (A, MD) | NR | Psych, med, cross-training | NR | 2 | 2 | NR |
| CA4 (42) | US | 1995 | U/T | PMU | — | P: 9 (L, S) | range 5–18 | Psych (A, MD), ped (C) | Specialty residents | Psych, cross-training | NR | 1 | 3 | NR |
| CA5 (46, 47, 50) | ISR | 1999 | U/T | PMU | 3 | P: 9 | range 8–18 | Psych (A), ped (C) | NR | Psych | NR | 1 | 2 | NR |
| AE1 (24, 26, 57) | US | 1980 | U/T | NSU | 4 | M: 32 | M=44, range 16–63 | Psych (A, MD), med (A) | Med, psych, and double board | Med cross-training | M=9 | 1 | 2 | For reference 57, cohorts pre-post unit conversion; GRADE C. No significant differences for recidivism and return to responsible activity. |
| AE2 (23) | US | 1981 | G/C | NSU | 1 | P: 10 (O, S) and M: 25 | NR | Psych (A) med (NR) | Med | Med cross-training | M=7 | 2 | 2 | NR |
| AE3 (25) | US | 1982 | U/T | PMU | 4 | M: 13 (O) | ≥16 | Psych (A, MD) med (A) | NR | Med cross-training | NR | 2 | 2 | NR |
| AE4 (11, 27, 32, 55) | US | 1983 | U/T | MPU | 1, 5 | M: 15 (O) | ≥16, M±SD=46.2±14.2 | Med (A, MD) psych (C, MD) | Med and psych | Med | M=14 | 2 | 2 | NR |
| AE5 (28) | US | 1984 | U/T | PMU | 1, 2, 4, 5 | M: 14 (O) and P: 24 | ≥60% were >60 | Psych (A, MD) med (A) | Psych | Med | Median=4 | 3 | 2 | NR |
| AE6 (30, 58, 60) | US | 1985 | U/T | PMU | 4, 5 | P: 20 (L) and P: 80 | M±SD=40.4±17.1 | Psych (A), med (A) | Psych | NR | M=13 | 2 | 3 | For references 58, 60, cross-sectional design of IMPU vs. C-L service and psychiatric inpatient unit; GRADE C. C-L service had longer LOS (22.1±40.8 days) than IMPU (13.2±12.3 days) and psychiatric inpatient unit (13.5±9.9 days). |
| AE7 (29) | US | 1985 | U/T | PMU | 4 | P: 23 (O) | >13 | Psych (A, MD), med (A) | Psych | Psych and med | M=25 | 2 | 2 | NR |
| AE8 (11, 59) | US | 1985 | U/T | PMU | 1, 5 | P: 19 (O) | M±SD=54.1±18.3 | Psychiatrist (A, MD), med (C) | Med for emergency | Psych, med experience each shift | M=23.1 | 2 | 2 | For reference 59, cohorts pre-post unit conversion; GRADE C. LOS increased from 13.9 to 23.1 days, cost of treatment on IMPU increased at a greater rate than the hospital’s average. |
| AE9 (56) | US | 1986 | G/C | ND | — | 1–12 of unknown type | M=39.7, range 11–96 | Med (A) | NR | NR | M=37 | 1 | 2 | NR |
| AE10 (31, 33, 61) | US | 1986 | ND | PMU | 1, 4 | P: 8 | NR | Psych (A, MD), med (C) | Med | Med with cross-training | M=17 | 2 | 2 | For reference 61, consecutive cohorts of IMPU patients; GRADE C. LOS decreased from a mean of 20.5 days in 1984/85 to a mean of 16.8 days in 1986. |
| AE11 (7, 34, 65) | US | 1989 | U/T | CU | 2, 3, 4 | M: 15 (L, S) | M±SD=47±17 | Dually trained or med (A), psych (A) | Med, psych | Dually trained, cross-training | M=17.5, median=13 | 3 | 3 | For reference 65, interrupted time series: IMPU vs. internal medicine wards (IMWs); GRADE C. Functioning: IMPU GAF +19.5±20.9 (p<.05), Karnofsky Performance Scale (KPS) score +24.3±19.5 (not statistically significant), IMW GAF 11.2±16.3 (p<.05), IMW KPS 22.4±21.4 (not statistically significant). Total hospital LOS: IMPU 18± 13 vs. IMW 13±8 days (p=.01). |
| AE12 (62) | CAN | 1992 | G/C | PMU | 1, 4 | P: 6 and P: 49 on larger unit | M±SD=39.5±14.7 | Psych (A, MD), med (C), neu (C) | Psych | Psych | M=19 | 2 | 2 | For reference 62, cross-sectional design of IMPU vs., general adult inpatient service (GAIS) and geriatric psychiatry service (GPS) patients; GRADE C. LOS IMPU 19.3±21.2 days, GPS 38.6±49.4 days (significantly different from IMPU and GAIS), GAIS 18.6±18.9 days. |
| AE13 (40, 45) | IRL | 1994 | G/C | PMU | — | P: 3 and P: 22 on larger unit | M=33, range 14–72 | Psych (A), med/surg (A) | NR | Psych | Median=2 | 2 | 2 | NR |
| AE14 (63) | AUS | 1995 | U/T | PMU | 3, 4 | P: 4 and P: 30 on larger unit | M±SD=43.7±17.7, range 17–87 | Psych (A, MD), med (C) | Psych | Med and Psych, cross-training | M=22 | 2 | 2 | For reference 63, cross-sectional: IMPU vs. general psychiatry unit (GPU) patients; GRADE D. IMPU LOS 22±23 days vs. GPU LOS 25±22 days. |
| AE15 (44) | US | 1995 | G/C | PMU | — | P: 20 (O) | NR | Psych (A) | Psych | NR | M=21 | 1 | 2 | NR |
| AE16 (64) | JAP | 1996 | G/C | PMU | 4, 5 | P: 63 (O, S) | M±SD=54±16 | Psych (A), med (C) | Psych | Psych with med or surg experience, cross-training | M=122 | 2 | 2 | For reference 64, cohorts: first vs. latter 2 years; GRADE D. Mean LOS shortened (from 158 to 122 days, not statistically significant). 73% of general medical illnesses cured or improved; 65% of psychiatric disorders unchanged. |
| AE17 (48) | UK | 1999 | U/T | PMU | 2 | I: 12 | Median=49, range 19–78 | Psychiatrist (A), med (C) | NR | Doubly qualified | Median=18 | 2 | 2 | NR |
| AE18 (49) | TWN | 2001 | U/T | PMU | — | P: NR | M=46.3, range 18–77 | Psych (A), med (C), surg (C) | NR | NR | M=20 | 1 | 1 | NR |
| AE19 (8, 9) | CHE | 2004 | U/T | PMU | 1, 2, 3 | P: 18 (L, S) | Range 16–65 | Psych (A), med (A) | Psych | Mixed | M=26, median=21 | 3 | 3 | For reference 9, consecutive cohorts; GRADE D. Mean LOS increased from 14 days in 1999–2000 to 21 days in 2003–2004 (p<.001). |
| AE20 (67) | NL | 2010 | U/T | MPU | 1 | M: NR | M±SD=52.8±15.1 | Psych (A), med (A) | NR | Mixed | M=24 | 2 | 2 | For reference 67, GRADE C. Controlled before and after medical costs of IMPU vs. medical wards were lower (€104, 95% CI=€35–€174, p<.01). Total costs after IMPU admission were higher than for medical ward admission (€263, 95% CI=€68–€458, p<.01). |
| AE21 (7) | US | 2018 | U/T | MPU | 1, 2, 3 | M (O): NR | NR | Med (A), psych (C) | NR | Med | NR | 3 | 1 | NR |
| AE22 (7) | US | 2018 | G/C | PMU | 1, 2, 3 | P: 102 (L,S) | NR | Psych (A), med (C) | NR | Psych, cross-training | NR | 2 | 3 | NR |
| AE23 (7) | US | 2018 | U/T | PMU | 1, 2, 3 | P: 24 (l, S) | NR | Psych (A, MD), med (C) | NR | Psych, cross-training | NR | 2 | 3 | NR |
| AE24 (54) | NL | 2019 | U/T | MPU | 1, 3, 5 | NR (L) | Median=46, range 18–94 | Trauma surg (A), psych (C) | NR | Dually trained | Median=10 | 3 | 3 | NR |
| E1 (20) | UK | 1973 | C/G | MPU | — | G: 4 and G: 17 on larger unit | Elderly population | Ger (A), psych (C) | NR | Ger | M=20 | 2 | 1 | NR |
| E2 (22) | UK | 1980 | U/T | PMU | — | G: 16 and P: 8 and G: 25 on larger unit | “Pensionable age” | Ger (A), psych (A) | NR | NR | 98% for ≤ 1 month | 3 | 2 | NR |
| E3 (35, 39) | US | 1989 | U/T | PMU | 5 | I: 14 | M=68, range 18–92 | Psych (A, MD) | NR | NR | M=22 | 2 | 2 | NR |
| E4 (36) | US | 1990 | C/G | MPU | 4 | P: NR | NR | Psych (A), med (C) | NR | Mixed, cross-training | M=24 | 2 | 2 | NR |
| E5 (43) | US | 1995 | C/G | PMU | — | P: 20 (L, S) | M±SD=76±10, range 39–96 | Psych (A), med (A) | NR | Med with variable psych experience | M=15 | 3 | 3 | NR |
| E6 (66) | DEU | 2007 | C/G | AU | 2, 3, 5 | G and PG: 64 | >60 | Ger (A), psych (A), neuro (C) | NR | Mixed, cross-training | Median=18 (geriatric), median=26 (psychogeriatric) | 3 | 3 | For reference 66, mixed methods before and after; GRADE C. Majority of employees: treatment quality and allocation of patients were improved after opening. No. of transferals decreased significantly. Median LOS decreased from 22 days in 2000 to 18 days in 2001 (p<.001). |
| E7 (51) | UK | 2008 | ND | ND | — | NR: 26 (O) | “Old age” | Psych (A), ger (A) | NR | Mixed | NR | 2 | 2 | NR |
| E8 (52) | UK | 2008 | C/G | ND | 1 | 21 | >65 | Psych (NR), ger (NR) | Med and psych | Mixed | M=44 | 2 | 2 | NR |
| E9 (53, 68–70) | UK | 2011 | U/T | MPU | 2, 4 | G: 28 | Median=85, IQR=80–88 | Ger (A), psych (C) | NR | Ger and 3 extra psych | Median=11 | 3 | 2 | For reference 68, randomized controlled trial; GRADE B. No significant difference in days spent at home between IMPU and standard care (69). Qualitative interviews with caregivers from the IMPU who appreciated IMPU improvements. Communication and engagement of family caregivers were still perceived as insufficient. Reference 70 included cost-effectiveness analysis; GRADE B. The IMPU was very cost-effective when usual criteria were applied. |
| E10 (7) | US | 2018 | U/T | MPU | 1, 2, 3 | G: 25 (O) | Elderly population | Med (A), psych (C) | NR | Med, cross-training | NR | 3 | 2 | NR |
Context
Aims
Unit Type
Age group focus.
Patient population.
Structural Characteristics
Unit size.
Ward features.
Medical staff.
Nursing staff.
Other disciplines.
Process Characteristics
Referral and admission.
Collaboration.
Training.
Treatment.
Acuity capabilities.
Outcomes
Economic outcomes.
Quality.
Discussion
IMPU Types
Maximizing Value
Lessons From Integrated Care
Limitations
Future Directions
Conclusions
Footnote
Supplementary Material
- View/Download
- 886.84 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).