Addressing the general medical needs of people with serious mental illness is a pressing public health challenge. Most people with serious mental illness have one or more chronic general medical conditions that can be exacerbated by obesity and tobacco use and can reduce life expectancy by up to 26 years (
1–
4). Yet, people with serious mental illness are less likely to receive guideline-concordant primary care, have more nonpsychiatric emergency department visits and inpatient stays, and spend more on medical services, compared with those without serious mental illness (
5–
8).
Strategies that integrate primary care and treatment for patients with serious mental illness can improve engagement in primary care, manage chronic disease risk factors, and—in some cases—reduce emergency department use among these patients (
9–
14). These integrated care strategies—sometimes referred to as “reverse integration”—often combine care management, chronic disease management using patient registries, and primary care colocation in specialty mental health facilities. Providers participating in alternative payment models, such as accountable care organizations (ACOs), may use these strategies to improve primary care for people with serious mental illness.
ACOs—networks of doctors, hospitals, or medical practices held accountable for the total cost and quality of care of assigned patient populations—form an alternative payment model built on fee-for-service payment (
15). To earn savings, ACOs must meet spending targets based on historical spending patterns, which tasks participating providers with lowering spending while also meeting quality targets. Adults with serious mental illness, for whom care coordination and chronic disease management could reduce acute care utilization, may benefit from the holistic treatment encouraged by ACO contracts (
15,
16). Alternatively, ACO contracts could further fragment care for patients with serious mental illness. Efforts to reduce service utilization could lead to undertreatment, as happened under some Medicaid full-risk capitated managed care contracts (
17). The spending targets included in ACO contracts could encourage mental health service “carve-outs” to managed behavioral health care organizations, separating mental health services from other medical care and potentially limiting access to primary care or other services for beneficiaries with serious mental illness (
18,
19).
The few studies examining organization and quality of mental health treatment under ACO contracts suggest that most ACOs have not integrated behavioral health and primary care and have found few changes in utilization rates associated with these contracts (
20–
24). Yet, these studies also found that certain ACO characteristics, such as inclusion of safety-net providers in the ACO network, were predictive of integrated care (
20,
21). Similarly, ACOs and ACO-like organizations responsible for shared losses in their contracts (downside financial risk), such as Massachusetts’ Alternative Quality Contract, saw greater reductions in inpatient spending for their patients with mental illness after contract start (
22,
23).
However, these studies have typically not distinguished between patients with serious mental illness and those with any mental illness, even though care settings and service use differ by diagnosis and symptom severity. Patients with serious mental illness are disproportionately represented among high-cost, high-need patients, whose complex physical, social, and behavioral health needs have resulted in historically high medical expenditure (
16). We analyzed the organizational structure and care delivery strategies reported in a national survey of ACOs to estimate the prevalence and correlates of three strategies to integrate primary care and treatment for serious mental illness among ACO respondents.
Methods
Study Design and Survey
We conducted a cross-sectional analysis of responses to the 2017–2018 National Survey of Accountable Care Organizations (NSACO). We fielded the 2017–2018 NSACO from July 2017 to March 2018. The survey included questions about ACO contract and organizational characteristics and also specific mental health care delivery capabilities (
25). We invited participants by using both Web and paper invitations to improve response rate; among all respondents, most completed the survey online (80%). The Dartmouth College Committee for the Protection of Human Subjects approved the survey protocol and communication with potential respondents, including informed consent.
Setting and Participants
Survey participants included leaders of organizations participating in ACO contracts, such as the organization’s chief executive or population health administrator. We defined ACO contracts as contracts that hold organizations responsible for the total cost of care and quality of care for a designated patient population, consistent with previous survey waves and the Centers for Medicare and Medicaid Services (CMS) rules (
26,
27). We constructed the sampling frame by using publicly available lists of Medicare ACO participants combined with ACO registries curated by consultant groups specialized in tracking ACO activity (Leavitt Partners and Salesforce). We included all ACOs participating in 2017–2018 contracts, excluding dialysis treatment organizations, organizations without contact information, organizations not meeting our definition of an ACO (ineligible), and pilot organizations surveyed during survey development. Of an estimated 862 eligible organizations, 55% returned a survey and 49% completed the survey (a figure in an
online supplement to this article provides further details).
Main Outcome Measure
Our primary outcome was self-reported use of strategies to integrate primary care and treatment for serious mental illness endorsed in response to this survey question: “Do any providers in your ACO use the following strategies to integrate primary care and treatment for serious mental illness, like schizophrenia or bipolar disorder?” Response options included: 1) “A care manager to ‘address general medical health treatment coordination’ OR to ‘address non-medical needs (e.g., job support, housing),’” 2) “Patient registries to track general medical health conditions (e.g., hypertension, glucose control),” and 3) “A co-located primary care clinician seeing patients in specialty mental health setting” (see
online supplement for additional survey details). Because the term ACO could refer to contracts, an organization as a whole, or an entity that is part of a larger organization, we asked respondents to “respond on behalf of the organization most commonly participating in ACO contracts.”
Covariates
Self-reported contract and organizational characteristics asked in the 2017–2018 NSACO were used as covariates (see
online supplement). Contract characteristics included whether the respondent had an ACO contract with Medicare, Medicaid, or a commercial payer; whether the respondent’s ACO shared financial risk (i.e., took on downside risk) in its Medicare, its largest Medicaid, or its largest commercial contract; and whether the respondent’s ACO had prior experience with risk-based contracting. We also measured contract features specific to mental health services in respondents’ non-Medicare contracts; unlike Medicare contracts, commercial and Medicaid ACO contracts may exclude mental health services. We asked whether a respondent’s largest Medicaid contract—or, separately, largest commercial ACO contract—included mental health services in the total cost-of-care calculation (the spending benchmark), any behavioral health quality measures, quality measures specific to serious mental illness (e.g., adherence to antipsychotics for schizophrenia), or a “carve-out” of mental health services by contracting out care to a managed behavioral health care organization. Organizational characteristics included leadership of a respondent’s largest ACO contract (physician led versus not), size (quartile of number of physician full-time equivalents in largest contract), and types of providers included in the largest ACO contract (academic medical centers, public hospitals, federally qualified health centers, and specialty behavioral health providers). Finally, we asked respondents whether any providers in the ACO used any of three collaborative care strategies to integrate primary care and treatment for depression or anxiety (care management, consulting mental health provider, or patient registry; coded as a count of 0, 1–2, or 3 collaborative care strategies).
Statistical Analysis
Each integrated care delivery strategy was measured as a 0,1 binary outcome, where 1 indicated that the respondent reported using this strategy at least once in at least one location to care for patients with serious mental illness.
To form outcomes for analysis, we created a vector of care integration strategies (care manager, patient registry, and colocated primary care clinician) “stacked” by strategy at the ACO level. For example, for respondents reporting using a care manager only, this vector would equal 1,0,0. We regressed this stacked outcome on all ACO characteristics and strategy type (
28). We also included interaction terms between each ACO characteristic and strategy type indicator to test whether the association between ACO characteristics and use of a care integration strategy differed by strategy type. To estimate the relationship of interest, the association between the marginal (i.e., unconditional) probability of each care integration strategy and the ACO characteristics, we fit the model by using generalized estimating equations, specifying a logit link function, an unstructured correlation matrix, and robust standard errors (
29,
30). This approach—an extension of standard logistic regression—permitted regression coefficients on ACO characteristics to vary by care integration strategy, an estimated correlation matrix between care strategies, and statistical inferences accounting for any statistical dependencies between the outcomes for the same ACO. (Additional details explaining our rationale and full model results are available in the
online supplement.)
To more easily interpret effects, we transformed log-odds into the expected average change in probability of implementing each integrated care strategy studied, holding other variables at their observed values (average marginal effects). We considered p<0.05 statistically significant.
Missing Data
We used multiple imputation to account for missing covariate data from 48 respondents (12%) (estimates below use imputed data; for complete case results, see
online supplement). We included all covariates from our analytic model in the imputation model and specified 10 data sets across which to pool final estimates.
Results
Characteristics of ACOs, 2017–2018
Of ACO respondents, 399 answered the survey questions about the three strategies used to integrate primary care and treatment for serious mental illness. Most respondents contracted with Medicare (84%) and commercial payers (72%), while just a quarter had an ACO arrangement with Medicaid (24%) (
Table 1). Most respondents reported having prior experience with risk-based contracts (64%), but a minority (37%) reported sharing financial risk in at least one contract (Medicare contract, the largest Medicaid contract, or the largest commercial ACO contract). Few respondents (21%) reported that the largest Medicaid or largest commercial ACO contract included a financial carve-out of mental health services to managed behavioral health care organizations. Less than half of respondents (43%)—including respondents that did and did not report having a financial carve-out—reported that the largest Medicaid or largest commercial ACO contract included mental health services in the total cost of care calculation (the financial benchmark). A third of respondents (34%) reported that the largest Medicaid or largest commercial ACO contract held them accountable for any behavioral health care quality measures, and just 18% were subject to performance measures specific to serious mental illness, such as follow-up after mental health hospitalization or antipsychotic adherence in these non-Medicare contracts.
ACO-Reported Use of Integrated Care Delivery Strategies, 2017–2018
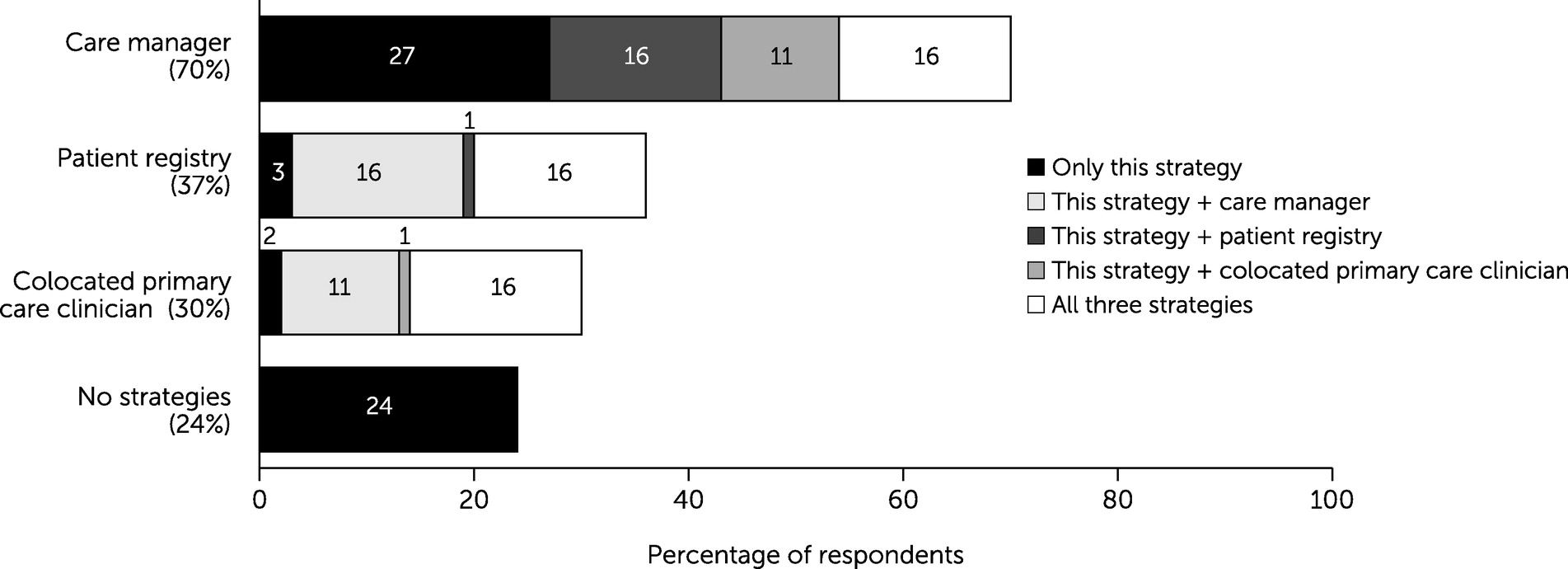
When asked whether any providers in the ACO integrated primary care and treatment for serious mental illness by using a care manager, patient registry, or colocated primary care provider, respondents most commonly reported using a care manager to address physical or social needs (N=281, 70%;
Figure 1). Approximately one-third of respondents reported using a patient registry to track general medical conditions (N=146, 37%) or having a colocated primary care clinician (N=118, 30%;
Figure 1). Approximately one-quarter of respondents (N=107, 27%) relied exclusively on care managers to integrate services, another quarter reported using a combination of a care manager and either a patient registry or colocated primary care clinician (N=109, 27%), and 16% (N=65) of respondents reported using all three strategies. Nearly a quarter of respondents (N=96, 24%) reported using no strategies.
ACO Characteristics Associated With Use of Any Integrated Care Delivery Strategy
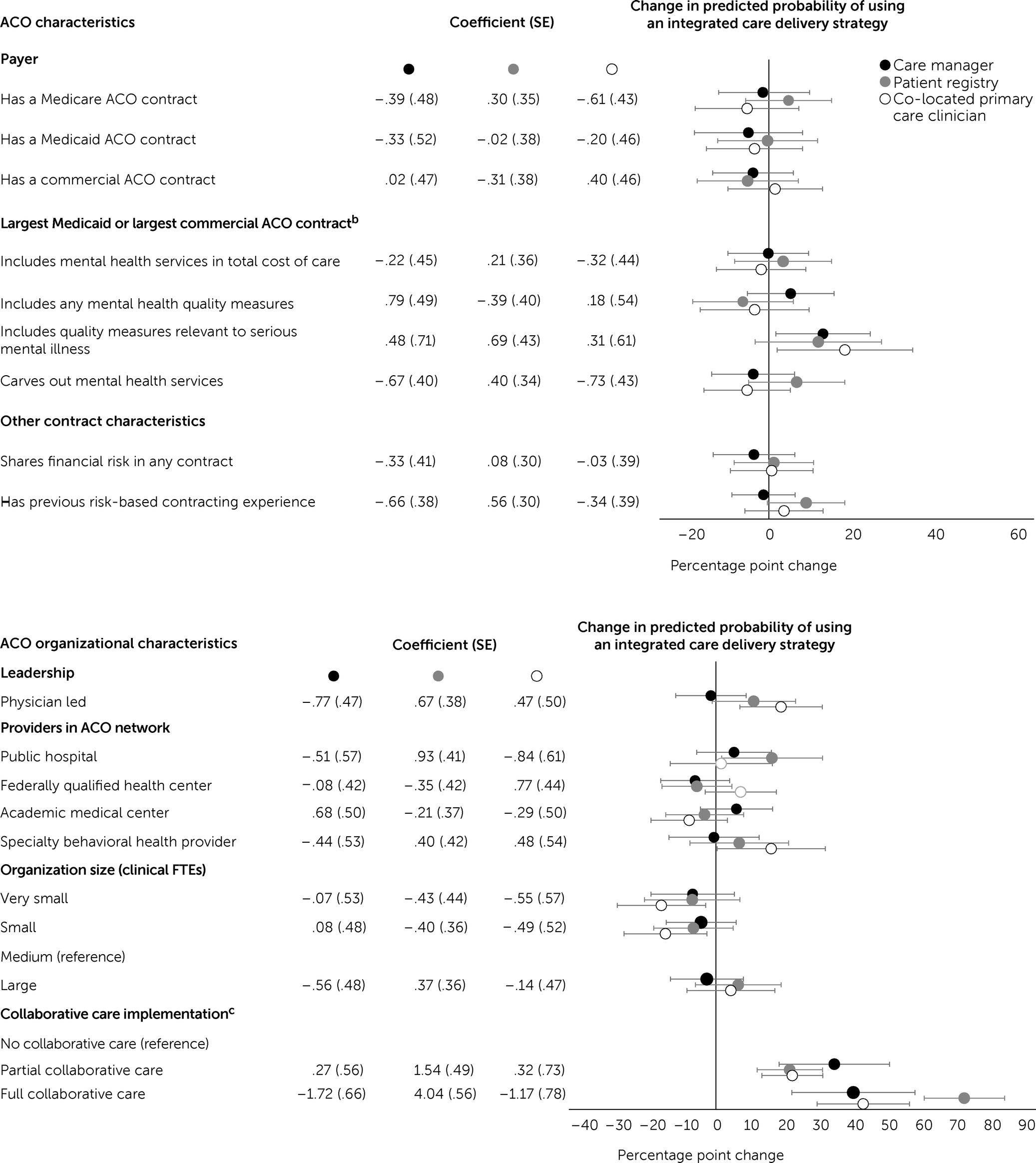
ACO respondents subject to quality measures relevant for populations with serious mental illness in their largest commercial or largest Medicaid contract were 12 percentage points, or 20%, more likely to use patient registries to track physical health conditions (95% confidence interval [CI]=−3, 27;
Figure 2). The association between behavioral health quality measures and care integration strategy use did not differ significantly for care managers or colocated primary care clinicians relative to patient registry (
Figure 2).
Among organizational characteristics that we measured, only one—use of collaborative care for patients with depression or anxiety—had a consistently positive statistically significant association with the likelihood of use of each of the three integrated care strategies for patients with serious mental illness. After the analysis adjusted for ACO contract and organizational characteristics, respondents implementing one or two collaborative care strategies were 22 percentage points (95% CI=12, 31), or 80%, more likely to report using patient registries, compared with respondents using no collaborative care strategies, with similar associations for care managers or primary care colocation. Respondents implementing all three collaborative care strategies were 73 percentage points (95% CI=61, 84) more likely to report using any integrated care delivery strategy for their patients with serious mental illness, suggesting that respondents fully implementing collaborative care were well positioned to integrate care for serious mental illness as well. Finally, physician-led ACOs were 19 percentage points (95% CI=7, 31) more likely to report having primary care colocation. However, ACOs that were physician led were no more likely than other ACOs to adopt care managers or patient registries.
Discussion
Using data from a national survey of ACOs, we found that only one-third of respondents reported using either patient registries or colocated primary care clinicians to integrate primary care and treatment for serious mental illness. We have reported strategies that ACO respondents asserted were used by any provider at least once in one location. Thus, our results underscore how rarely these evidence-based practices are used. That few respondents reported using a registry was surprising; chronic disease burden is significant among patients with serious mental illness, and registries offer an opportunity to manage disease risk factors at the population level. Our finding that a quarter of respondents reported primary care colocation is comparable to findings reported in studies that examined prevalence of primary care colocation by using provider practice location data (
31,
32).
That care manager was the most commonly reported strategy is not surprising; care managers could include any member of the care team assisting patients in coordinating treatment for their medical or nonmedical needs (e.g., housing or employment). Prior studies have documented that ACOs frequently use care management programs to coordinate care and reduce spending, even though these programs vary significantly in scope and quality (
33,
34). If respondents were subject to social desirability bias, the broad description included in our question text may have biased estimates upward. Again, these data likely overestimated the use of all three integration strategies among ACO providers and might be better interpreted as a best-case scenario or upper bound on their use.
Inclusion of quality measures relevant for populations with serious mental illness (i.e., antipsychotic adherence for patients with schizophrenia) in a respondent’s largest Medicaid or largest commercial contract was the only contract characteristic significantly associated with self-reported use of each of the three integrated care strategies studied. Incorporating quality measures relevant for the population with serious mental illness in payment contracts could be important to support integration in the future, particularly as more state Medicaid agencies participate in ACO contracts.
Even though reverse integration and collaborative care target different patient populations and settings of care, we found that self-reported use of three collaborative care strategies to treat depression or anxiety was correlated with efforts to integrate primary care for patients with serious mental illness. Although our estimates of collaborative care use may be inflated—respondents could have interpreted collaborative care to mean any program that integrates mental health treatment in primary care settings—our finding that collaborative care use was correlated with integrated care for patients with serious mental illness could reflect shared resources across settings of care. Respondents’ use of collaborative care strategies to integrate care for patients with depression or anxiety may have aligned clinical priorities and resources that are applicable to both integration models, such as shared clinicians or a common electronic medical record (
21,
35,
36).
We had hypothesized that respondents who included specialty behavioral health providers in their ACO would be more likely to report using strategies to integrate primary care and treatment for serious mental illness. Since 2010, these specialty behavioral health providers have been eligible for federal grants focused on implementation of integrated primary care services, such as Primary and Behavioral Health Care Integration awards from the Substance Abuse and Mental Health Services Administration (
37). However, just 14% of respondents reported including a specialty behavioral health provider in their ACO network, and inclusion of these providers was not associated with integrated care use. These findings suggest that specialty behavioral health providers continue to face barriers to ACO contract participation, such as limited adoption of electronic health records (
21,
38).
This study used novel survey data to examine strategies ACOs used to integrate mental health and primary care services for patients with serious mental illness. However, the study had several limitations. Our survey had a comparatively low response rate, limiting the generalizability of our findings. We did not provide definitions for the three studied integrated care strategies beyond the question wording. Because respondents may have interpreted these strategies broadly, our estimates of these measures—especially prevalence of care managers—may be overestimated. Because care managers have such a broad scope of services, defined by the Agency for Healthcare Research and Quality as any team member coordinating or handling patient needs, respondents may have reported using care managers to integrate primary care and treatment for serious mental illness even if these personnel had limited experience coordinating these particular services (
39). We do not know how frequently ACO-attributed beneficiaries received integrated care services or how often ACO providers employed these strategies. For questions in which we asked about respondents’ largest ACO contract, we do not know whether results would differ if the question had been asked about “any ACO contract” instead. Our reliance on cross-sectional data means that we can state only the associations between ACO characteristics and strategy use.
Conclusions
A third of respondents to a national survey of ACOs reported using either patient registries or primary care colocation to integrate primary care and treatment for patients with serious mental illness. The sole contract characteristic significantly and positively associated with integrating each care strategy for these patients was the presence of quality measures targeting people with serious mental illness in an organization’s largest Medicaid or largest commercial ACO contract. Among organizational characteristics, the most consistent predictor of reported integrated care use was self-reported use of collaborative care for treatment of depression or anxiety.