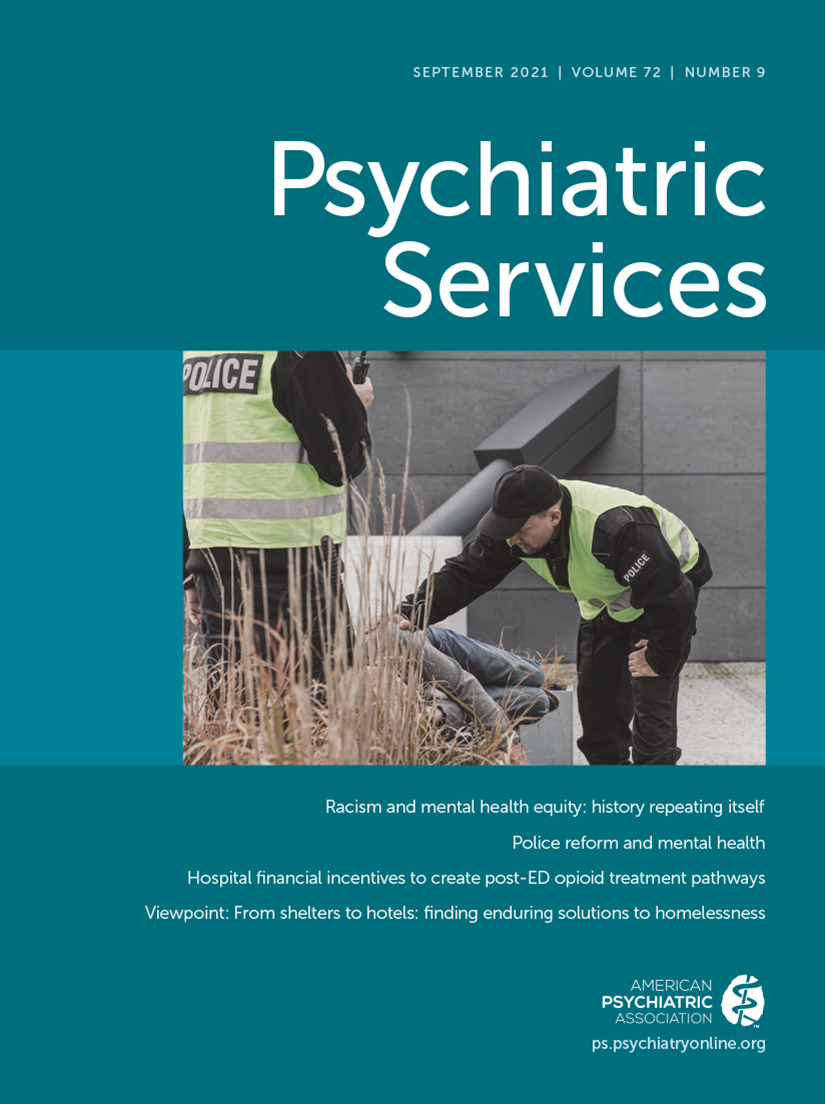
The need to reduce the role of law enforcement in responding to mental, behavioral, and social vulnerabilities, particularly in communities of color, is highlighted with tragic frequency. As a result, the United States is grappling with a growing movement to reform or defund the police and a mental health system that may not have the capacity to take on crisis response. In this Open Forum, we argue for the development of responses to mental health crises that do not involve law enforcement.
Police as Primary Responders to Mental Health Crises
How did we as a society come to rely so heavily on police to address mental health and social vulnerabilities? Shortly after the advent of early psychotropics, the Community Mental Health Act of 1963, an emerging civil rights movement, and other social advances, deinstitutionalization began, moving hundreds of thousands of people with serious mental illnesses back into communities. However, the transition occurred without adequate investment in community-based supports, leaving many people without access to treatment and at risk for a variety of social vulnerabilities associated with criminal legal system involvement. Additionally, court rulings in this era resulted in more stringent civil commitment criteria, with an emphasis on dangerousness, further defining a role for police in the apprehension of people in need of psychiatric emergency services. In the decades that followed, shrinking mental health budgets left few or no other crisis response options in many communities. Bonfine et al. (1) have rightly pointed out that criminal legal system involvement among persons with mental illnesses is also prominently driven by social and economic forces as well as by the complex clinical, behavioral health, criminogenic, and social needs of those with such illnesses.
People in need of urgent mental health care are now regularly directed to call 911. Call takers often have limited options: send police, emergency medical services, or both. Often, once the call is identified as related to mental health, police are dispatched regardless of whether there is a safety or criminal issue. Although some communities have mobile crisis teams (composed of clinicians) that can be deployed, these teams may not be accessible via calling 911. Additionally, limited hours of operation and limited capacity of mobile crisis teams often mean lengthy wait times or no immediate availability, leaving police as the only option during a crisis.
As responsibility for crisis response has shifted to law enforcement, significant changes in policing practices have also ensued. Backlash against the civil rights movement led to a tough-on-crime political ideology and the declaration of the War on Drugs. In the Reagan era, increased federal funds flowed to local law enforcement, as did tanks and military-style equipment to fight the “war,” in what many refer to as the militarization of law enforcement (2). The role of police concurrently became more warrior-like. The result has most negatively affected communities of color, whose members are disproportionately represented in all stages of the criminal legal system, from police patrol, to jails and prisons, to probation and parole.
One of the consequences of these shifts is that police are involved in the pathway to care for almost one-third of people with mental illnesses in the United States (3). Tragically, such shifts may also have contributed to the overrepresentation of people with mental illnesses among those shot and killed by police (4). Additionally, although most individuals experiencing a mental health crisis are not involved in criminal behavior, relying on police responses may increase their likelihood of arrest and thus of becoming involved in the legal system. In the context of structural racism, the burden of these negative outcomes is disproportionately experienced by people of color (5, 6), who are more likely to enter mental health care through coercive channels, more reliant on emergency care, more likely to have police involved in a mental health crisis, and more likely to be killed by police.
Those of us working in the mental health field and advocating for persons with serious mental illnesses have been more successful to date in expanding capacity to address mental health needs within the criminal legal system than we have been in improving the community mental health system. This circumstance may be in part because, in the United States, individuals do not have a constitutional right to mental health care unless they are in the custody of the state. It may also be because shrinking mental health budgets during a period of growing law enforcement budgets has allowed for law enforcement agencies to build responses that fill gaps.
Crisis Intervention Team and Co-Responder Models
The crisis intervention team (CIT) is a collaborative model that has received much attention. The model is based on strong partnerships among law enforcement, the mental health system, and advocates and is best known for including 40 hours of training on mental health issues and de-escalation strategies for select officers who then become CIT officers. Policy makers have proposed CIT training for all officers as a means of improving police responses and even as an approach to broadly addressing race-based disparities in policing. Providing CIT training to all officers may not be effective, however. The most effective CIT response is likely to be from an officer situated within a strong CIT program who is CIT-trained and who wants to be a CIT officer. The latter element is critical, and universal CIT training cannot be expected to result in all officers being equally talented, compassionate, or effective in responding to individuals in crisis. Certainly, all officers need de-escalation and basic mental health response training (which is not the same as CIT training or implementing a CIT program). But CIT training is a specialist training. Furthermore, CITs are unlikely to be a solution for addressing broader race inequities, because it was not designed for this purpose (even though many CIT training sessions include some content on cultural competence).
Recently, the co-responder model has gained attention. While there are many variations on this model, typically, clinician-officer teams respond to crisis situations in response to 911 calls or requests from other officers; they may also conduct follow-up outreach and linkage. Although it may seem sensible to elevate co-responder models as a promising practice, these models do not go far enough. Certainly, police are needed in some crisis situations because of safety concerns or criminal activity, and, in many states at present, only law enforcement can take a person into custody for involuntary transport for psychiatric assessment. However, in many situations, police presence is not necessary and in fact may escalate the situation and increase trauma, stigma, and criminalization.
At the national level, ongoing efforts to improve law enforcement response to mental health crises are exemplified by the Bureau of Justice Assistance’s Police–Mental Health Collaboration Toolkit project and the International Association of Chiefs of Police’s One Mind campaign. Writing about disaggregating the police function, Friedman (7) suggests that efforts to reduce the harms of police intervention are unlikely to be effective: “The deeper difficulty with a harm reduction strategy . . . is that much of policing is not proactive, but reactive, and we won’t ameliorate policing’s harms until we address the underlying social issues that cause people to call the police in the first place.” Thus, initiatives are needed at intercept 0 (mental health and crisis services that do not require engaging police) to reform the mental health system so that it has the capacity to truly take up crisis response (8). Police will continue to have a role in a subset of mental health crisis events, and they must be prepared to safely partner with mental health responders (for example, as part of a strong CIT program). However, expanded options at intercept 0 can reduce the law enforcement footprint in crisis response.
Shifting Responsibility Away From Law Enforcement
Shifting responsibility for mental health crisis response away from police requires an adequately funded and functional community mental health system with a workforce ready to embrace its role in crisis response (8). Such a system would include accessible and timely crisis response options that do not automatically send law enforcement. It would have an expanded workforce capacity including a robust peer workforce and the ability to hire, train, and retain experienced clinicians. We suggest that there may be a need to create an entirely new professional role—for an emergency psychiatric technician—filled by individuals who are interested in and dedicated to responding to behavioral health crises and are adequately trained to do so. This role would be structured to support meaningful partnerships with law enforcement when needed and collaborations with acute and longer-term care providers who accept handoffs from crisis workers.
Although the current political moment calls for a sense of urgency, this shift will not happen overnight. It will require communities to dramatically change how they receive, triage, and dispatch responses to 911 calls. Some communities have developed protocols for transferring 911 calls to crisis lines and/or mobile crisis teams, whereas others are experimenting with embedding clinicians within 911 call centers (9). The Federal Communications Commission’s plan for the 988 mental health emergency number may also provide an avenue for accessing a non–law-enforcement response. Examples of non–law-enforcement responses to draw upon for inspiration include CAHOOTS (Crisis Assistance Helping Out On The Streets), in Eugene, Oregon, which pairs a medic with a crisis worker, and the Psychiatric Emergency Response (PAM) team in Stockholm, Sweden (10), which pairs mental health nurses with paramedics.
A Note of Caution
As we encourage accountability in the mental health system for reducing the role of law enforcement in responding to individuals in crisis, the field must ensure that the path forward does not increase racial inequities in the criminal legal or health systems, but rather that solutions proactively seek to reduce such disparities. As Meares et al. (
11) wrote in a recent editorial, “It is essential to recall that the crisis of policing is not simply about policing. It is about the state. A critical worry is that some narrow conversations about ‘defunding’ assume that the other parts of the system are operating the way they should be, and we know they are not.” Fully scoping how to build a racially equitable crisis response system will require utilizing racial equity impact assessments in making policy decisions, critically examining how risk is assessed in crisis calls, and reducing possibilities for racial bias in deciding on the appropriate response. Furthermore, the mental health profession’s workforce capacity must be expanded to better support entry for people of color. Finally, communities of color must be fully engaged in the planning and implementation of local crisis response systems and of the structures that hold them accountable.