It is estimated that one in 25 adults in the United States experiences serious mental illness each year (
1) and that serious psychological events, including death by suicide (
2), are increasing over time. The emergence of COVID-19 with its associated burden on mental health is expected to exacerbate the incidence and prevalence of serious mental illness, and the U.S. mental health system must brace for this impact (
3–
6).
Hospital emergency departments (ED) are currently the frontline provider when triaging mental health crises in the United States (
7–
9). First responders and mental health professionals rely on EDs for brief stabilization or as a means for obtaining an inpatient bed. However, these settings often lack the resources and privacy needed to manage acute psychiatric events (
10), especially among children and adults with a developmental disability (
9,
11). Psychiatric visits that are not true emergencies are problematic because their length of stay is much longer than medical visits (
12). There is even evidence suggesting that the lengths of these visits are increasing (
12). When psychiatric ED visits are not urgent, they absorb precious health care resources and extend wait times for people with acute needs. Two large recent studies suggest that a significant proportion of mental health visits to the ED are not urgent (
9,
13) and could be evaluated and treated in different settings. Therefore, outpatient mental health crisis services play an important role in managing both acute and subacute psychiatric events, especially because EDs were a diminishing resource during the pandemic.
The Substance Abuse and Mental Health Services Administration (SAMHSA) defines mental health crisis services as “no-wrong-door safety net services” that are “for anyone, anywhere, and anytime” (
14). These services provide rapid access to psychiatric evaluation or treatment, with the goal of avoiding escalation and preventing immediate harm. Crisis services take many forms, from crisis hotline services to specialized outpatient and hospital-based models. The actual therapeutic methods employed by these settings vary by setting and expertise. Generally, they employ methods such as verbal deescalation and psychotherapeutic strategies, as-needed medications, outpatient and inpatient referrals, and treatment planning. Comprehensive psychiatric emergency programs (CPEPs) have become increasingly important models of hospital-based psychiatric care (
15). These programs have a trained group of mental health professionals that provide medical and psychiatric evaluation, often offering extended observation beds for short-term evaluation. CPEP services can even include both mobile and in-home services that provide longer-term (often 1–2 months) education, therapy, and medication management.
Two important in-person clinical services in the continuum of crisis care include psychiatric walk-in and crisis services. Psychiatric walk-in services reflect the availability of immediate, unscheduled, in-person assessment whenever the outpatient or inpatient facility is in operation (
16,
17). Substantial heterogeneity in the services offered by walk-in models ranges from treatment for ongoing symptom management (e.g., follow-up medication management) to assessment of an acute incident (e.g., determining whether a referral for inpatient treatment is warranted). Walk-in models have been shown to be helpful for improving care access among traditionally underserved groups who may struggle to maintain connections to their outpatient providers (
18). At a minimum, this service reflects the facility’s willingness and capacity to accept urgent referrals.
Unlike walk-in models, crisis services actively respond to mental health events, often through community outreach. The treatment these services provide depends on the nature of the referral and of the disciplines (e.g., social work, psychiatric nurse) present on the team. Crisis services frequently respond to acute events by providing brief interventions (e.g., brief psychotherapy, deescalation). Crisis services also often partner with local law enforcement, termed crisis intervention teams, in order to improve outcomes such as minimizing incarceration when possible. A recent Cochrane review reported that crisis services are promising and can reduce inpatient hospitalizations (
19).
No recent epidemiological research has examined the availability of these community-based approaches to crisis prevention and management in the United States. A population-level understanding of the availability of these services is important for public health planning, particularly in light of the strain that COVID-19 has placed on health care systems. To address this gap, the current study had three aims: examine changes in the availability of walk-in models and crisis services, between 2014 and 2018, across the United States; survey the characteristics of facilities that offer these services; and evaluate regional and state-to-state geographical variation in the availability of such services.
Methods
Sample
Data for this study came from the National Mental Health Services Survey (N-MHSS). The N-MHSS is a cross-sectional annual survey, sponsored by SAMHSA, of all known public and private mental health treatment facilities in the United States (
http://www.samhsa.gov/data/data-we-collect/n-mhss-national-mental-health-services-survey) (
20). Its primary purpose is to serve as an annual census of all U.S. mental health care facilities that is curated in the National Directory of Mental Health Treatment Facilities (
https://www.samhsa.gov/data/report/2020-national-directory-mental-health-treatment-facilities) and the Behavioral Health Treatment Services Locator (
https://findtreatment.samhsa.gov). The survey is completed by facility staff, including the director or an administrator. The most recent 5 years of publicly released N-MHSS data were used for this study. Data released before 2014 were excluded from this study because of substantial missing data (2010) or omission of an outcome variable of interest (2012). The mean N-MHSS response rate between 2014 and 2018 was 90%. We note that the N-MHSS is a deidentified survey. As such, it is not possible to identify how many unique facilities are represented. Further information about the N-MHSS can be found at
https://wwwdasis.samhsa.gov/dasis2/N-MHSS.htm.
The other data used in this study were retrieved from the U.S. Census Bureau (
21). Census data served as the denominator when calculating population-based rates of services per 100,000 adults (ages ≥18 years) in the United States. Census data were joined with the N-MHSS data at the state level for each year. Because N-MHSS and Census data are publicly available and fully deidentified, the governing institutional review board did not consider this study human subjects research.
Exclusion Criteria
Facilities were removed if they were listed as residential treatment facilities or owned by the U.S. Department of Veterans Affairs (VA) because these facilities were available only to those living onsite or served only veterans, respectively, and were not available to the general public. Facilities located in the Virgin Islands and other American territories were also excluded. These inclusion criteria resulted in an average of 10,032 facilities included per year.
Variables
Outcomes.
The primary study outcomes were the reported availability of psychiatric emergency walk-in or crisis services. Psychiatric emergency walk-in services were captured in a checklist of services list on the N-MHSS questionnaire (
22). SAMHSA defines psychiatric emergency walk-in services as “specifically trained staff to provide psychiatric care, such as crisis intervention, in emergency situations on a walk-in basis to enable the individual(s), family members and friends to cope with the emergency while helping the individual function as a member of the community to the greatest extent possible” (
22). The N-MHSS survey assessed crisis services with a stand-alone question: “Does this facility operate a crisis intervention team to handle acute mental health issues at this facility or offsite?” No further definition for this term is provided to survey respondents or in the N-MHSS codebook.
Characteristics of mental health facilities.
A host of facility-related descriptors were available. These included the facility setting (psychiatric hospital, separate inpatient psychiatric unit of a general hospital, community mental health center, partial hospitalization/day treatment facility, outpatient mental health facility, multisetting mental health facility, and other), whether the facility was licensed by a state mental health agency (yes or no), and type of ownership (private for-profit, private nonprofit, or public). Information about insurance acceptance was also available, including whether the facility accepted Medicaid (yes or no), whether it used a sliding scale for fees (yes or no) based on household income, and provision of substance use services (yes or no).
Analysis
To address the first study aim described above, we performed two analyses. First, we used a random-effects logistic regression model to evaluate changes in the probability of a facility offering a crisis service between 2014 and 2018 with data solely from the N-MHSS. State was considered a random effect, to account for state-level clustering. Second, population rates (calculated as the number of facilities that offer an identified crisis service per 100,000 U.S. adults per year) were reported descriptively and graphically. For the second and third aims, descriptive statistics were used to better understand the characteristics of facilities that offered crisis services. To understand state-to-state variability, national maps were generated. Census data were used in these maps as the denominator to calculate population rates (per 100,000 adults) at the state level. Between-state variations in the census-adjusted availability of the identified service were displayed by using a 5-point color-coding scheme, which was based on binning the population rates into quintiles. Only data from 2018 were analyzed for aims 2 and 3, to provide the most up-to-date information. All analyses were conducted in STATA, version 15.0. Because there were very few missing data (<3% on all variables), we conducted a complete case analysis.
Results
Between 2014 and 2018, one-third (N=16,793, 33.5%) of all mental health facilities (N=50,160) offered emergency psychiatric walk-in services, and just under one-half provided crisis services (N=24,170, 48.3%) (
Table 1) (percentages are based on totals that excluded missing data). When a facility offered walk-in services, it often provided crisis services as well (N=12,199 of 16,767, 72.8%). When crisis services were offered, walk-in services were provided half of the time (N= 12,199 of 24,136, 50.5%). Overall, 42.6% (N=21,269) of facilities did not offer either service, 33.0% (N=16,505) offered one of the services, and 24.4% (N=12,199) offered both services.
Trends in Crisis Service Availability
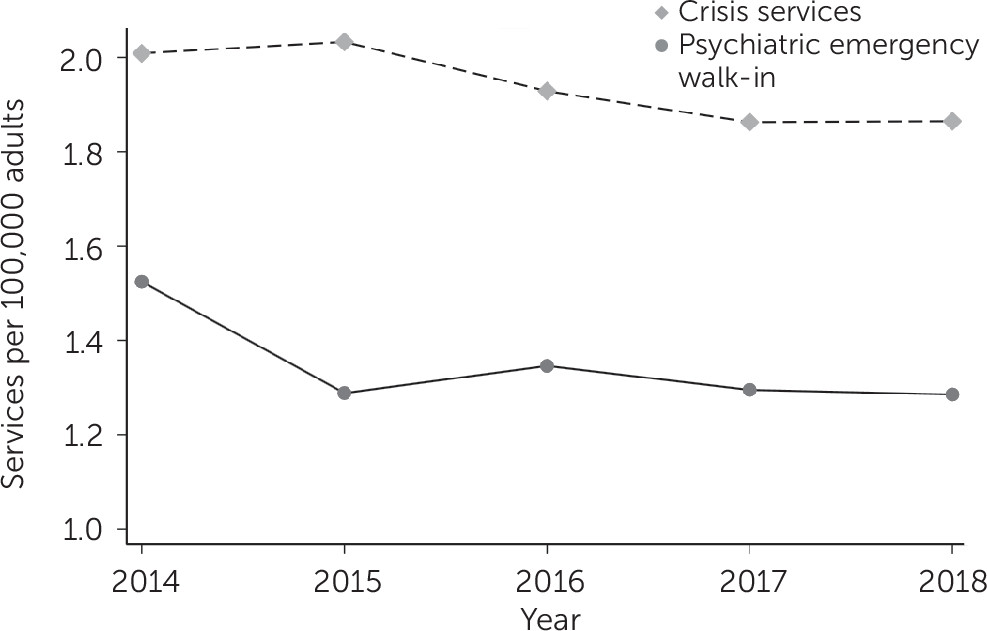
The census-adjusted estimates of services per 100,000 adults ages ≥18 years are shown in
Table 1 and
Figure 1. The proportion of facilities that offered walk-in services slightly declined between 2014 (36.4%) and 2018 (33.8%) (
Table 1). Results from the random-effects logistic model indicated a decrease in the provision of walk-in services between 2015 and 2018, compared with 2014 (all p<0.001). Provision of crisis services significantly decreased from 2014 to 2015 (p=0.04). However, no significant change was observed thereafter, when compared with crisis service availability in 2014. Between 2014 and 2018, walk-in and crisis services declined by 15.8% (1.52 to 1.28 facilities per 100,000 adults) and 7.5% (2.01 to 1.86 facilities per 100,000 adults), respectively.
Characteristics of Crisis Facilities
As shown in
Table 2, hospitals and community mental health clinics most frequently offered psychiatric walk-in and crisis services (49%−67%), whereas all other settings provided these services less frequently (except multisetting facilities, 50.5% of which offered crisis services). Most (about 80%) facilities that provided either crisis service were certified by the state. Public facilities were more likely to provide both services, especially when compared with private for-profit facilities. Almost all facilities that offered walk-in or crisis services (>97%) accepted Medicaid, although substantially fewer facilities provided services at a sliding scale (68%). About two-thirds of facilities that provided walk-in or crisis services offered substance use–related services.
Geographic Locations of Crisis Facilities
Table 2 shows the regional differences in the proportion of facilities that offered crisis services. Using only the N-MHSS data, we found that facilities in the South offered the highest proportion of both services, whereas the Northeast had the lowest.
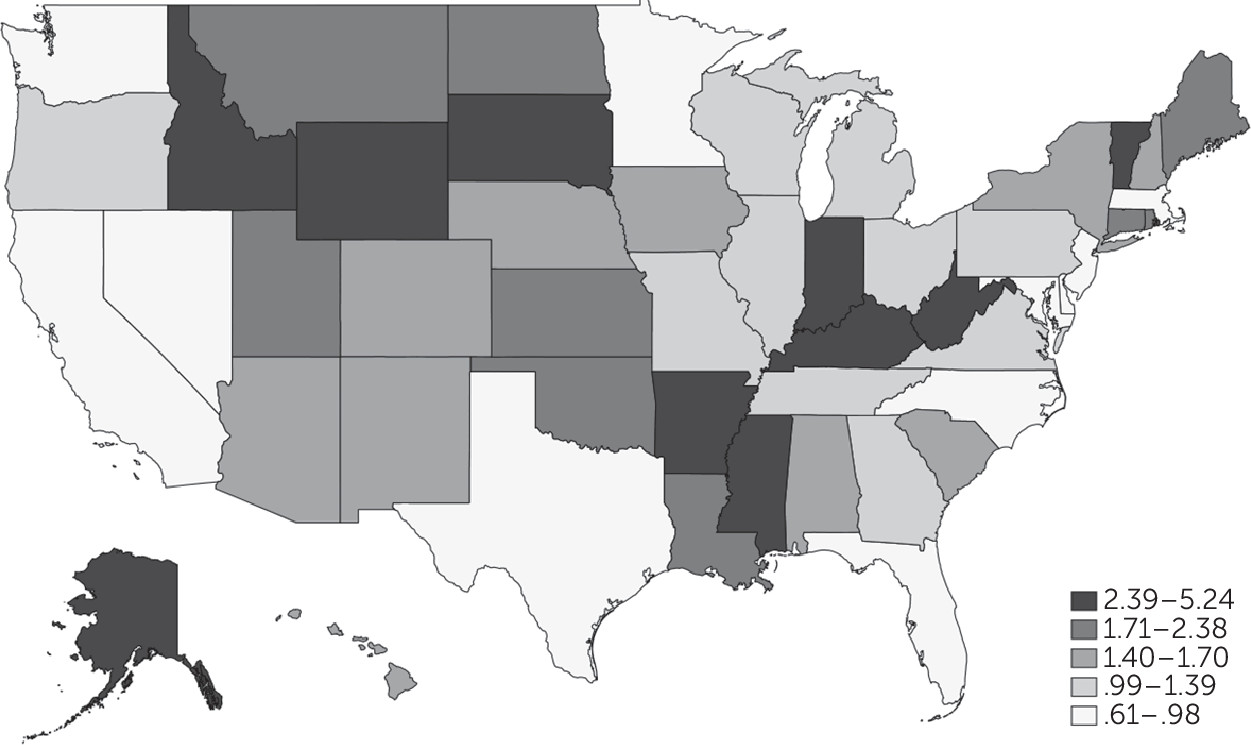
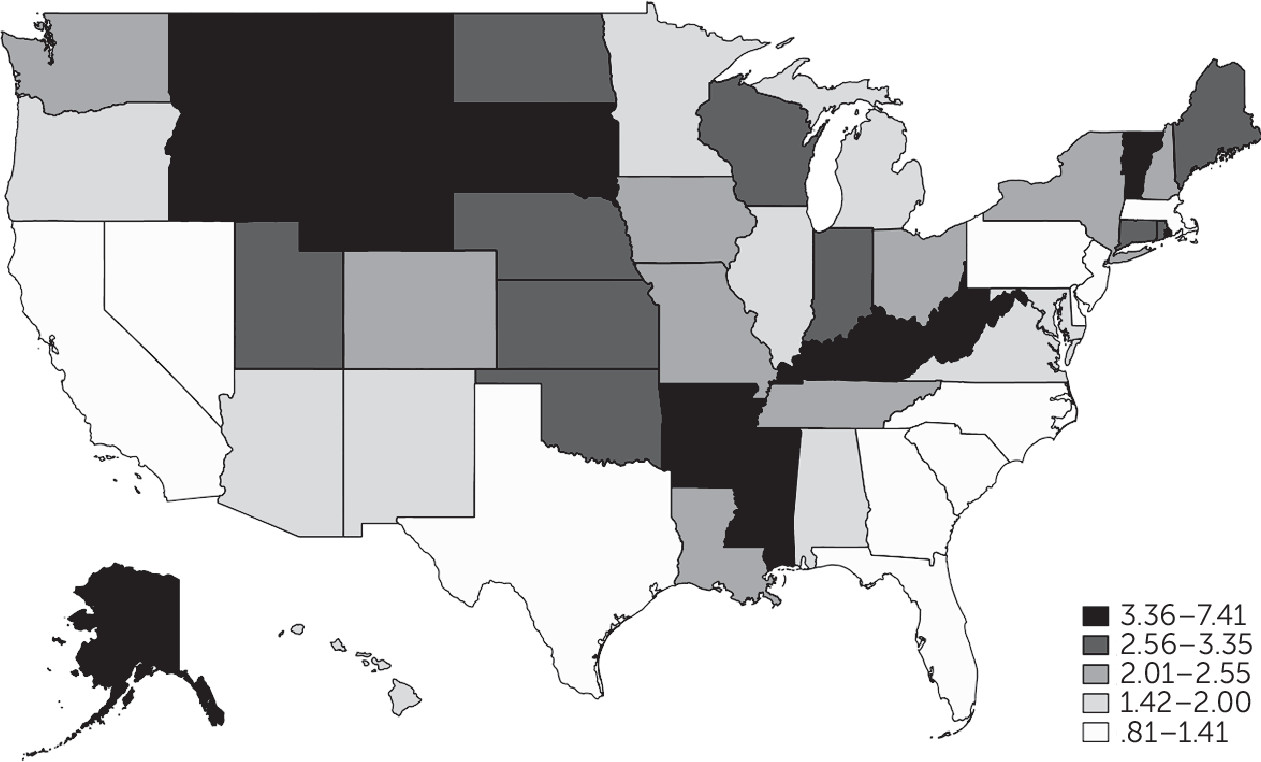
Figure 2 and
Figure 3 display state-to-state variability in walk-in and crisis services, respectively, in 2018. State-specific estimates are shown in a table in an
online supplement to this article. Both walk-in and crisis services had low availability in Massachusetts, New Jersey, Delaware, North Carolina, Florida, Texas, Nevada, and California.
Discussion
Overall, >40% of all mental health facilities in the United States did not offer the mental health crisis services evaluated in this study between 2014 and 2018. One-third offered emergency psychiatric walk-in services, and fewer than half provided crisis services; only a quarter offered both. After 2014, the likelihood of a facility offering psychiatric emergency walk-in care significantly decreased. No significant change was observed in crisis services. These findings are disconcerting in the context of recent increases in suicide and opioid-related deaths in the United States (
23,
24). The results raise concerns about the availability of mental health crisis services, particularly for those who do not access outpatient services in a traditional way, to manage acute psychiatric events either passively (through referrals and walk-ins) or actively (through outreach, such as crisis services).
The availability of psychiatric walk-in and crisis services varied substantially by geographic location. This finding reveals a lack of national policies or standards for such crisis services. In general, the Northeast region, as seen for Massachusetts, New Jersey, and Delaware, had the lowest proportion of services. However, states outside of the Northeast also had low service availability, including North Carolina, Florida, Texas, Nevada, and California. This finding raises concerns about an underdeveloped psychiatric emergency infrastructure in these regions. We believe the census-based estimates provide the greatest understanding of geographic availability of mental health crisis services, as opposed to the regional proportions (based solely on N-MHSS data), which account for population density.
The above findings are especially pertinent in the era of COVID-19. Even before the pandemic, EDs in the United States were stretched beyond their capacity (
25–
27). As the pandemic spread, the emergency management system had fewer resources than ever to attend to those with mental health issues. Our results suggest the need for licensed mental health facilities throughout the United States to expand the provision of crisis services. This is particularly the case for outpatient settings, which are the largest segment of the mental health system, but where less than one-quarter provide walk-in services and about one-third provided crisis services. As state and federal governments are generating and applying stimulus packages to address gaps in the health care system as revealed by the COVID-19 pandemic, attention could be paid to funding training and delivery of crisis services in general, because mental health care should be fully integrated into a systems-based approach to disaster response and recovery (
28). Critically, increased availability of crisis services and facilities alone is not sufficient to meet the needs of individuals in psychiatric crises. As noted by Hogan and Goldman, broader changes in policy and funding are needed. These changes include an increase in authorization and appropriation of funds by Congress, a 5% Mental Health Block Grant, increased funding for research and evaluation, additional payment mechanisms, and a central coordinating role for Congress (
29).
This study should be interpreted in light of its strengths and weaknesses. In terms of strengths, the data used in this study were nationally representative. Survey and item-response rates were high. The findings are novel, timely, and important for both national and state policies. A critical limitation was the lack of details about how, and for whom, crisis services were delivered, including the number of individuals actually served (as opposed to facilities’ capacity). Another important limitation was that details about additional crisis services were limited. These additional services include hotlines, crisis stabilization beds, CPEPs, peer supports, EmPATH (emergency psychiatric assessment, treatment, and healing) units, and psychiatric observations that were not measured by the N-MHSS or this study. Thus, this study does not reflect the true availability of crisis services in the United States nor does it demonstrate the efficacy of such interventions. The exclusion of VA administration, given that veterans face unique needs and require in-depth examinations, is another limitation. Finally, there was some conceptual overlap between the items used to capture walk-in versus crisis services, because we could not differentiate between onsite and offsite crisis services. Respondents may have selected both items or services even when only walk-in services were available, because they may have considered onsite crisis services the same as walk-in services.
Conclusions
A large proportion of U.S. mental health facilities were not delivering the mental health crisis services evaluated in this study. Between 2014 and 2018, the population-adjusted availability of crisis services decreased. The large state-to-state variability observed here reveals the need for a national approach to crisis training and service delivery. It also raises questions about whether the U.S. health care system can provide sufficient acute mental health care services both during and after the COVID-19 pandemic.