The COVID-19 pandemic has disrupted the U.S. labor market in three ways. First, it shifted the location of work for those whose jobs could be done remotely (
1). Remote workers tend to be higher earning, more educated, and non-Hispanic White, compared with the labor market at large. Second, the pandemic increased the health risks of employment for workers with essential jobs that could not be done remotely—about 42% of all workers (
2). These workers are disproportionately lower earning, less educated, and non-White. Finally, for the many workers whose jobs were not deemed essential and could not be performed remotely, COVID-19 often led to job loss. Between February and December 2020, millions of people became unemployed or left the U.S. labor force.
Workers with mental illnesses before the COVID-19 pandemic may have suffered disproportionately from the pandemic’s labor market disruptions, in terms of both their health and their employment, yet the extent of these impacts remains unclear. Evidence indicates that workers with mental illness are less likely than those without mental illness to have secondary and postsecondary education and are less likely to hold high-paying jobs. These workers are overrepresented in occupations that require manual skills and underrepresented in occupations that require nonroutine cognitive skills (
3). These patterns suggest that workers with preexisting mental illnesses may be less likely than others to be employed in jobs where remote work is feasible and, therefore, face occupational health risks (whether they are frontline essential workers or nonessential workers) or unemployment (if they are nonessential workers subject to closures, shutdowns, or staff reductions) during the pandemic.
Prior analysis has documented elevated rates of COVID-19 infection among people with mental illnesses (
4). No prior analyses have examined the employment impacts of COVID-19 on people with serious mental illness; however, these workers have seen disproportionate declines in employment in prior economic downturns (
3). The pandemic-induced recession was different from prior economic downturns, but the challenges associated with continued participation in the labor force among those with mental illnesses and the potential health risks associated with work warrant attention. In this column, we examine the job characteristics of workers with mental illnesses as a source of differential employment and health risks in the context of the COVID-19 pandemic.
To evaluate the job characteristics of workers with mental illness relevant to the context of COVID-19, we classified workers by levels of psychological distress prior to the pandemic and then used information about their occupations to categorize their jobs by essential or nonessential industry and by the feasibility of remote work. We analyzed data from the 2016–2018 National Health Interview Survey (NHIS), collected from the Integrated Public Use Microdata Series (
5). The NHIS collects information from respondents on symptoms of mental illness by using the Kessler Screening Scale of Psychological Distress (K6). This scale has been found to be a reliable measure of the prevalence of mental illnesses and serious mental illnesses (e.g., schizophrenia, bipolar disorder, major depression) in the overall population, although it does not provide specific diagnoses. We used cutoff scores based on the prior literature on the K6 to define four groups of psychological distress: none, mild, moderate, and severe (
3).
The NHIS collects employment information from respondents on industry and occupation by using four-digit industry and occupation codes informed by the North American Industry Classification System (NAICS) and the Standard Occupation Classification (SOC) System. To protect respondent confidentiality, NHIS public files aggregate four-digit codes into two-digit codes that correspond with NAICS industry subsectors and SOC occupation subgroups.
To categorize a respondent’s employment industry as essential or nonessential, we followed Blau et al. (
2) and others, who built on essential infrastructure guidelines issued by the U.S. Department of Homeland Security (
6). We classified 194 of 311 NAICS four-digit industries as essential and aggregated them into two-digit NHIS industry codes. For NHIS industries that contained both essential and nonessential four-digit NAICS industries, we collected national employment data from the Occupational Employment Statistics provided by the U.S. Bureau of Labor Statistics and considered the two-digit NHIS industry essential if at least 50% of workers nationwide in the NHIS industry were employed in essential four-digit NAICS industries. Otherwise, we categorized the essential status of these NHIS industries as “undetermined.”
To categorize an individual’s occupation as feasible or not feasible for remote work, we drew on data from the Occupational Information Network. Following Dingel and Neiman (
1), we created a binary measure of remote work feasibility for six-digit SOC occupations and then collapsed the measure into detailed two-digit NHIS occupation codes. For NHIS occupations that were both remote-feasible and not remote-feasible six-digit SOC occupations, we considered the NHIS occupation as feasible for remote work if more than one-third of workers nationwide in the NHIS occupation were employed in remote-feasible six-digit SOC occupations. This approach followed the methodology of Blau et al. (
2) in identifying frontline workers (essential workers unable to work remotely). Otherwise, we categorized the occupation’s feasibility for remote work as “undetermined.”
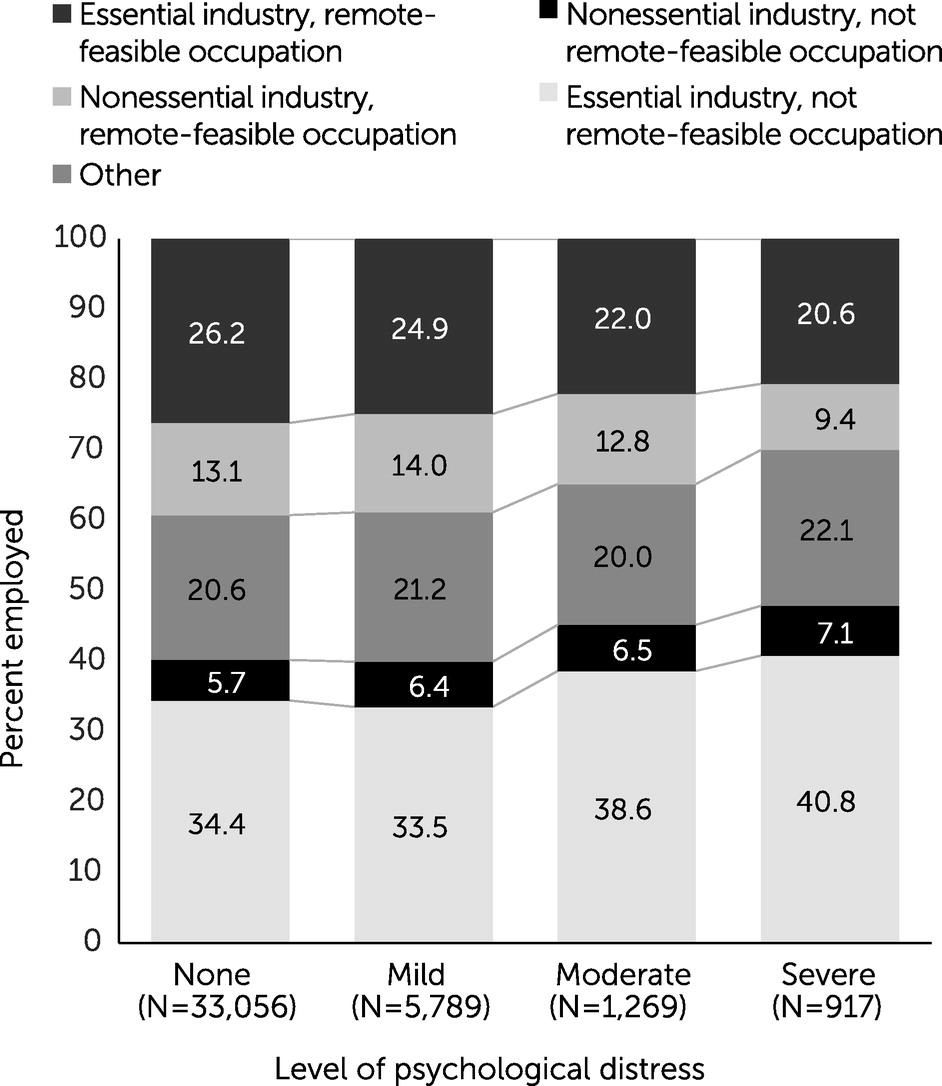
Our final sample included 41,031 civilian adults, ages 18–64, who reported K6 values and were working for pay within 2 weeks before the interview. Those with “undetermined” essential worker status or feasibility for remote work were retained in the sample. Figure
1 shows the distribution of workers in essential or nonessential industries and occupations that are feasible or not feasible for remote work, stratified by workers’ level of psychological distress.
Workers with severe psychological distress prepandemic were employed in an essential-industry occupation where remote work was feasible at rates almost 6 percentage points lower than workers without any psychological distress and were employed in a nonessential-industry occupation where remote work was feasible at rates almost 4 percentage points lower. Workers with severe psychological distress were also employed as frontline workers in an essential industry where remote work was not feasible at rates 6 percentage points higher than those with no psychological distress. In combination, these patterns suggest that workers with higher levels of psychological distress are both at higher risk of exposure to COVID-19 at work and at higher risk of becoming unemployed because of the pandemic. This pattern of results is not sensitive to the criteria we use to classify jobs as “remote feasible.” We found that the effects of psychological distress on occupational distribution are even stronger for respondents who identified as Black, compared with respondents of other races (see
online supplement). Black individuals at almost every level of psychological distress were employed at higher rates than their counterparts in frontline occupations, especially those with severe psychological distress (approximately 8 percentage points higher). Black workers across the spectrum of psychological distress were also employed at lower rates in occupations deemed nonessential and feasible for remote work.
The COVID-19 pandemic has presented a unique challenge to keep individuals with mental illnesses safely connected to the labor market while balancing the health risks of employment. A robust literature documents the negative impacts of unemployment on mental health and overall well-being. Work is an important way that individuals with mental illness are integrated in society and remain connected to others. Connectivity is especially important given the negative psychological impacts of disease-related quarantine, including posttraumatic stress symptoms, confusion, and anger (
7).
Our analysis was limited to examining the relationship between occupation and employment. However, the pandemic also increased rates of mental distress in the general population and among those with preexisting disorders. The prevalence of symptoms related to anxiety disorder increased from 8.1% in the second quarter of 2019 to 25.5% in June 2020, and the prevalence of symptoms related to depressive disorder increased from 6.5% to 24.3% over the same period (
8). People with anxiety-related and mood disorders were especially likely to exhibit higher levels of stress related to COVID-19, compared with those with no psychiatric disorder (
9). New onset or exacerbations of existing mental illness due to the pandemic could serve as a further barrier to employment for this population.
Given the unique challenges—and therapeutic benefits—of work among those with mental illness, policies, such as vaccination, that increase the safety of work by reducing risk of infection continue to be important. Although vaccine promotion is a mainstream solution, in that it benefits workers both with and without mental illnesses, targeted outreach and messaging for the population with mental illness may be warranted. Prior vaccination efforts have often had lower uptake among populations with serious mental illness. For example, a recent analysis found that only 25% of adults with severe mental illness receive the annual flu vaccine, compared with almost 50% of adults in the general population (
10).
Because access to mental health treatment has also been disrupted, even as levels of distress have increased, it is also important to continue engaging those with mental illness in treatment, which may help these individuals maintain a connection to the labor market. Finally, social safety net programs will be vital in providing financial support and health insurance coverage to people with mental illness throughout the pandemic.