Frequent users of the emergency department (ED) have long been the target of initiatives to improve care coordination and reduce costs in state Medicaid programs. These frequent ED users often have complex medical and social needs, including high rates of comorbid mental health and substance use disorders. Health information exchange (HIE) has been shown to improve the identification of frequent ED users (
1) and those at risk for a revisit shortly after ED discharge (
2). Yet, to date, few studies have examined the extent to which HIE can facilitate care coordination for frequent ED users, including linkage to follow-up mental health care (
3).
Beginning in 2008, hospitals in Washington State began adopting a novel ED-based HIE called the Emergency Department Information Exchange (EDIE; Collective Medical Technologies). EDIE assists hospitals with identifying frequent ED users and facilitates individualized care plans to address complex behavioral and physical health needs. Given early successes of the platform in the state, policy makers mandated that all hospitals begin using EDIE by July 2012 as part of a larger initiative called the ER Is for Emergencies program (for a further description of Washington’s program, see the
online supplement). Hospitals were required to write care plans and engage in activities that link frequent ED users to appropriate ambulatory care and community resources (
4).
Although a robust body of literature supports care plan development for high utilizers of medical services in ambulatory settings, care coordination by ED staff represents a novel strategy to try to effect change with a population of patients who may not be well captured in other settings. The state considers individuals with five or more visits in 12 months to be frequent users. Of these frequent users with Medicaid coverage, more than two-thirds (68.9%) have a mental health condition, and nearly half (44.5%) have a substance use disorder (
5).
In prior work, we found that EDIE was associated with an 8.2% reduction in ED use among frequent ED users in the first year after mandates were implemented (
5). Yet, it is unclear whether lower ED use occurred as a result of better care coordination and linkage to ambulatory care, a stated goal of the program. Moreover, since it was first launched in Washington State, EDIE (since renamed PreManage ED) has continued to expand throughout the United States and is now being used by hospitals in more than 30 states. The aim of the current study was to determine whether the adoption of EDIE in Washington State—an important natural experiment for HIE-facilitated care coordination in the ED setting—improved outpatient follow-up after ED discharge for Medicaid enrollees with mental health conditions.
Evaluation of a Statewide Intervention
We examined monthly cohorts of ED visits occurring between April 2010 and December 2015 among adult Washington State Medicaid beneficiaries who were identified as frequent ED users and had a co-occurring mental health condition. Individuals with mental health conditions were identified with state criteria for mental health service need, a broad definition that includes those with a mental health diagnosis, a mental health–specific service claim, or a psychotropic drug prescription within 1 year of their ED visit.
We analyzed outcomes that indicate better linkage to ambulatory and behavioral health care. To assess timeliness of care, we examined two measures, the proportion of frequent ED users with any physician follow-up within 30 days of an ED visit and the proportion of frequent ED users with mental health–specific follow-up within that same 30-day window. Short-term follow-up after an ED visit is arguably one of the most proximate outcomes that could be influenced by hospitals. To assess appropriateness of care, we examined changes in mental health service penetration at 1 year after an index ED visit, defined as the proportion of the population with a mental health condition who received mental health services during the year.
To account for the staggered adoption of EDIE, we used an event study design (
6) to examine changes in the outcomes of interest before and after the hospital-specific adoption of EDIE. This approach allowed for the analysis of dynamic treatment effects, providing aggregated estimates of the effect of EDIE relative to the time of adoption, as opposed to calendar time. Linear probability difference-in-differences (DiD) models with multiple time periods (
6) that adjusted for patient demographic characteristics (age, sex, race, ethnicity), clinical characteristics (number of ED visits, inpatient admissions, and primary care visits in the past year; Chronic Illness and Disability Payment System comorbidities, including substance abuse), hospital fixed effects, hospital rurality, and seasonal fixed effects were used to estimate the effects of EDIE adoption on the outcomes of interest. We report treatment effects of EDIE up to 2 years after adoption of the platform. We selected a 2-year follow-up because prior work suggested that any effects of EDIE would likely happen early on (
5).
Findings
We analyzed data from 254,718 ED visits among 52,437 Medicaid beneficiaries with frequent ED use and mental illness across 88 hospitals in the state. A majority of our study population was female (64.4%, N=164,101), White (70.7%, N=179,941), and non-Hispanic (92.2%, N=234,713), with a mean ±SD age of 39.8±11.7 years and 5.0±2.5 chronic conditions. Approximately 66.1% (N=168,368) had a substance use disorder. Enrollees had 4.9±6.5 primary care visits and 10.6±8.1 ED visits in the past year.
Around the time of the implementation of mandates for EDIE, when most hospitals were adopting the platform, we observed a slight increase in the proportion of frequent users who completed follow-up with any physician within 30 days of their ED visit (56.1%–58.2%). However, both 30-day mental health–specific follow-up (32.1%–28.4%) and receipt of mental health–specific services at 1 year (52.9%–49.4%) declined throughout the study period (see online supplement for a figure depicting trends).
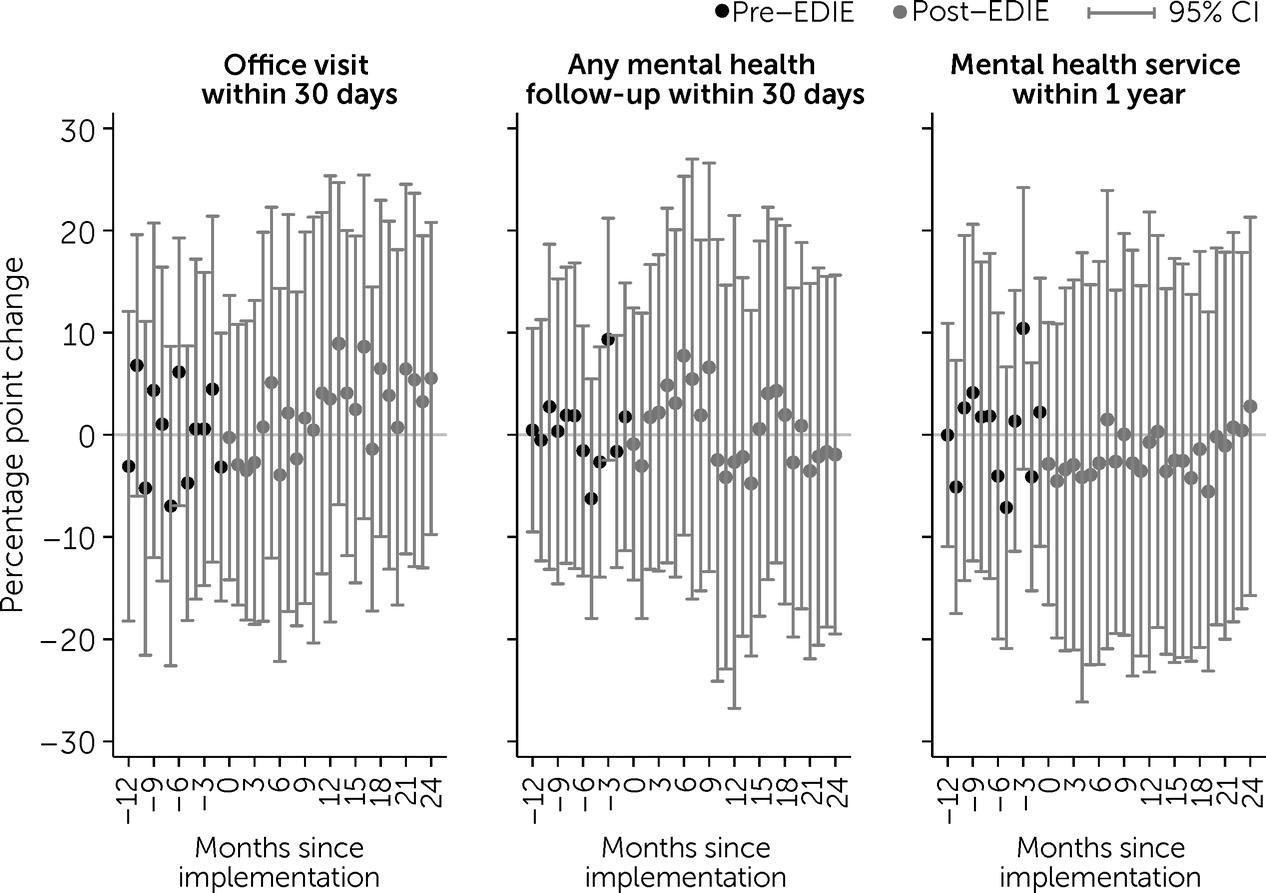
Adjusted DiD estimates revealed no statistically significant effect of EDIE on any of the three outcomes studied within 2 years of adoption (
Figure 1). Each point on the
y-axis reflects EDIE’s treatment effects, which correspond to the percentage point difference in the rate of follow-up care after an ED visit, comparing hospitals that had adopted EDIE with hospitals in the control group at time t relative to EDIE adoption. Confidence intervals around these monthly treatment effects all spanned an estimate of no effect and overlapped for nearly all periods studied.
DISCUSSION and Recommendations
We found no evidence to suggest that the implementation of an ED-based HIE improved primary care and mental health care follow-up among Washington State Medicaid enrollees with frequent ED use and a co-occurring mental illness. We did observe a slight increase in any office visit follow-up across the study period, particularly in the year after the implementation of EDIE mandates, although this increase did not rise to statistical significance in our DiD analysis. Rates of mental health–specific follow-up within 30 days of ED discharge as well as mental health service penetration at 1 year showed small declines over time, but these appeared to be unrelated to the implementation of EDIE.
Several systematic reviews have described the potential benefits of case management and individualized care plans through HIE platforms as strategies to improve care coordination for frequent ED users (
7,
8). Specifically, only case management—typically high-touch interventions that address medical, behavioral, and social determinants of health—has a strong evidence base for reducing ED use and improving ambulatory follow-up (
9). Although state policy makers had hoped that better identification of frequent ED users and care coordination for frequent ED users would catalyze local delivery system change, these efforts were ultimately insufficient to improve primary and mental health care follow-up after an ED visit. Hospitals likely continued to lack both the capacity to effectively meet the complex needs of their frequent user population and the accountability to reallocate limited resources, both of which could be improved by targeted policies. Without further resources for hospitals, such as technical assistance for developing effective care plans, funding to hire case managers or navigators, and financial accountability for patient outcomes, Washington’s experience suggests that EDIE adoption alone is unlikely to meaningfully change health care utilization.
Moreover, although data were universally shared between hospitals, care plans and other insights were variably shared with ambulatory providers. To be able to access patient data from EDIE, ambulatory providers also had to adopt a parallel platform and designate a prespecified treatment relationship with patients. A recent report from Virginia, which implemented EDIE statewide in 2018, suggests that states are still grappling with how to bridge the information divide and facilitate collaboration between the acute and chronic care systems with the use of EDIE (
10).
EDIE’s features have evolved over time to include Prescription Drug Monitoring Program data, event alerts (hospital admissions and ED visits) to primary providers and health plans, and integration with other state-specific data sets, among other features. In addition, there has been substantial expansion of enrollment in the platform by downstream providers (primary care physicians, federally qualified health centers, behavioral health providers, nursing homes, etc.) in Washington State and elsewhere. Although outcomes data from more recent implementation efforts remain limited, there are several examples in which regional coalitions (often consisting of Medicaid managed care organizations and providers) have formed and led to broad community adoption of EDIE (and its parallel platform for ambulatory providers). In most cases, EDIE has been used as an adjunct to other formalized care coordination activities (
7), with providers reporting significant value from the platform.
Linking frequent ED users to timely and appropriate general medical and behavioral health services remains a challenge that is unlikely to be bridged by adopting HIE and care plan development in the ED. Additional interventions, such as case management and pathways to increase bidirectional collaboration between hospital and ambulatory providers, are necessary to leverage EDIE’s full potential. Future studies should continue to investigate the value of care coordination activities centered in the emergency setting and the extent to which HIE can provide infrastructure for more intensive interventions to improve health care spending and utilization.