Diagnostic criteria for a
DSM psychiatric diagnosis are typically met by within-criterion symptom counts. Simple symptom counts treat each symptom as though it has equal priority (or “weight”) in reflecting underlying disorder severity. In clinical practice, many practitioners understand that “some symptoms matter more than others” (
1). Two patients who have the same number of symptoms, but a different pattern of those symptoms, will likely have different underlying disorder severities (
2). Thus, a simple total count of symptoms can give a distorted picture of a patient’s disorder severity and changes in severity following treatment (
2,
3).
Factor analysis (FA) and item response theory (IRT) methods incorporate differences in the clinical weights of symptoms in relation to underlying disorder severity (
2). Severity scores are weighted by factor loadings in FA or equivalently by discrimination parameters in IRT. In contrast, symptom counting assumes equal weights, which often fail to fit psychiatric symptom data when these data are formally tested (
2,
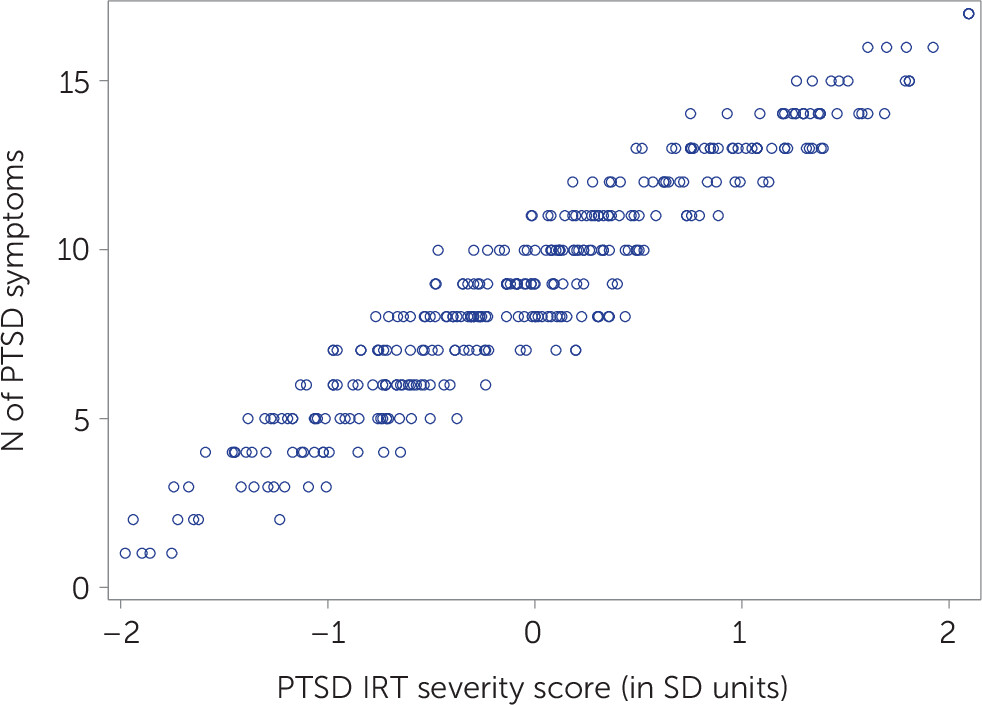
3). FA- and IRT-based scores may be highly correlated with symptom counts (r>0.90). However, as
Figure 1 shows, high correlations between these scores do not represent equivalence (
2).
Figure 1 presents data reported by Morgan-López et al. (
4) that were collected with the Clinician-Administered PTSD Scale for DSM-IV (CAPS-IV). Patients (N=353) were grouped by CAPS-IV diagnosis (full or subthreshold posttraumatic stress disorder [PTSD]) and by an empirical diagnosis based on the weighted midpoint of the IRT score distributions between the full and subthreshold diagnostic groups. The correlation between symptom counts and IRT scores was 0.95; high correlations between symptom counts and FA- or IRT-based scores are often cited as justification for using symptom counts (
2). However, patients with the same number of symptoms (y-axis) can vary appreciably (i.e., by >1 standard deviation in each horizontal band of data) in underlying PTSD severity (x-axis) because the combination of symptoms varies (
2,
3).
Equal weighting of symptoms in the
DSM contrasts with weighting methods that assume variability in the importance of symptoms. However, cross-population measurement studies are necessary for assessing whether the relative weights of each PTSD symptom can be universally applied; the weights of some symptoms are expected to vary in certain populations (
5). Given the importance of precise measurement of underlying psychiatric severity and classification, patients would benefit from greater use of symptom-weighting approaches for
DSM-based psychiatric assessments and a potential path forward for including symptom weighting in clinical practice.