The cost of treating mentally ill persons in the Medicare population has increased considerably in recent years; however, costs vary substantially among beneficiaries receiving mental health care. For example, a recent study that included Arkansas adults covered by Medicare indicated that the annual per capita cost of treating depressed patients was $631, but that approximately 5 percent of treated patients consumed 45 percent of outpatient expenditures (
1). In part, this finding may reflect an association between increased treatment costs and increased severity of psychiatric problems (
2,
3). In this study we sought to determine other possible sources of variation in the costs of treating mentally ill persons covered by Medicare.
Methods
We obtained a 5 percent randomly selected sample of all Tennessee Medicare beneficiaries who received services between 1991 and 1993. The data were provided by the U.S. Health Care Financing Administration and consisted of administrative reimbursement files on frequency of services and reimbursements for physicians, inpatient and outpatient services, and payments for hospice, skilled nursing, and home health care. The files contained information pertaining to International Classification of Diseases (ICD-9) diagnoses, specialty of service providers, procedures performed, cost per visit, and the beneficiaries' gender, race, age, county of residence, and zip code.
Only beneficiaries age 65 years or older were included in our analyses. We classified these beneficiaries by the presence or absence of mental health diagnoses. Mental health diagnoses were taken to include both substance use disorders and organic brain disorders. This definition was chosen to capture comorbidity in the broadest terms while maintaining a focus on mental health issues—an approach similar to that of several other investigators (
4,
5,
6). The diagnoses included
ICD-9 codes 190.0 through 198.9 and 300.0 through 312.9.
Additionally, we compared individuals who had been assigned multiple mental health diagnoses with individuals with only one mental health diagnosis. Persons with more than one psychiatric diagnosis—excluding recurrence of the same diagnosis, such as 296.23 and 296.33 for depression and recurrent depression—were considered to have multiple mental health diagnoses. Finally, we classified costs as mental-health-related or non-mental-health-related on the basis of the ICD-9 code to which the costs were attached.
A total of 33,680 beneficiaries were included in our analyses. Almost all—30,278 (89.9 percent)—were white; 21,218 (63 percent) were female, and 21,218 (63 percent) were urban residents. The median age was 75 years; females were older than males (mean age of 75.6 years and 74 years, respectively); African Americans tended to be older than whites (mean age of 75.9 years and 74.9 years, respectively). On average, African-American females were the oldest among the beneficiaries (76.3 years), followed by white females (75.5 years), African-American males (75.2 years), and white males (73.2 years). The median education of both whites and African Americans was 12th grade. A larger proportion of whites lived in areas with zip codes indicating higher median incomes.
Results
According to our ICD-9 definition, a total of 5,339 of the 33,680 beneficiaries (15.9 percent) had a mental health diagnosis, and 1,343 (25 percent) were classified as having multiple mental health diagnoses. Patients who had a mental health diagnosis were three years older on average than those who did not (mean age of 77.2 versus 74.4 years), but other demographic factors were comparable. No statistically significant differences were found between beneficiaries with and without multiple mental health diagnoses in terms of gender, race, median income or educational level in the zip code of residence, or urban-rural distribution.
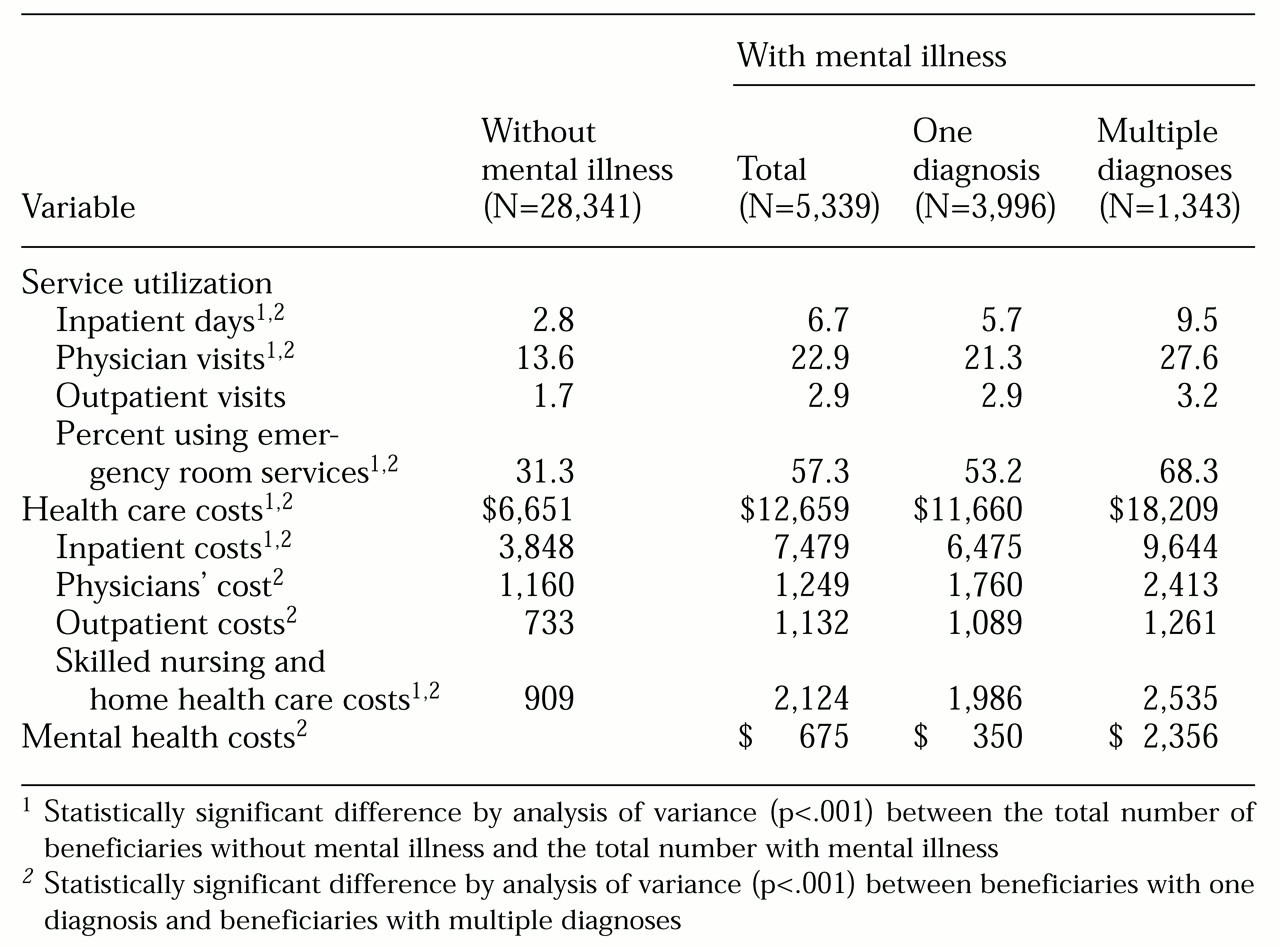
Mentally ill beneficiaries had significantly higher rates of service utilization and higher health care costs than beneficiaries with no mental health diagnoses, as shown in
Table 1. As expected, persons with multiple diagnoses had higher service utilization and higher health costs. Notably, however, most of the total costs for persons with mental illness was for health care rather than mental health care—97 percent of the costs for persons with one mental health diagnosis and 85 percent for those with multiple diagnoses.
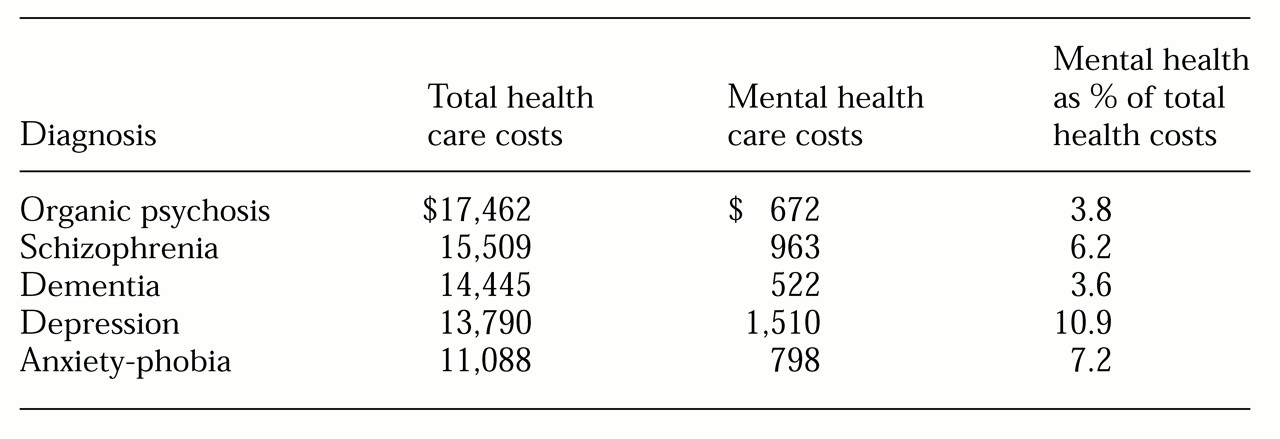
Overall treatment costs and the corresponding proportion of mental health costs for different diagnostic categories are shown in
Table 2. Although the highest overall cost was for patients diagnosed as having organic psychosis, the highest ratio of mental health to total health costs was for patients diagnosed with depression.
We also examined costs for multiple mental health diagnoses involving combinations of dementia, organic psychosis, schizophrenia, depression, and anxiety. Of the 1,343 patients with multiple diagnoses, 1,144 (85 percent) had at least two of these discrete diagnostic categories. Approximately half of the patients diagnosed as having dementia were also classified as having schizophrenia or organic psychosis, and half of those with mood disorders were also reported as having anxiety and phobias.
Although overall costs were not substantially different across the categories of multiple diagnoses, variation in average annual mental health costs was statistically significant (F=15.11, df=4, p<.000). The average annual cost was $4,197 for beneficiaries diagnosed as having both schizophrenia and depression (163 patients, or 12.1 percent); $2,817 for those with depression and anxiety (398 patients, or 29.6 percent); $2,071 for those with organic psychosis and schizophrenia (251 patients, or 18.7 percent); $1,884 for those with dementia and organic psychosis (339 patients, or 25.2 percent); $1,394 for those with dementia and schizophrenia (271 patients, or 20.2 percent).
Discussion
Although the data presented here refer to persons age 65 and older who received Medicare services, not only is the overall percentage of those with a psychiatric disorder, 15.9 percent, within the range of 9 percent to 20 percent reported by others (
7,
8), but the percentages of persons with specific diagnoses—dementia, organic psychosis, depression, and anxiety—are also consistent with previously reported rates. Moreover, the higher health care costs and higher rates of service utilization among elderly persons with mental illness are consistent with those reported by Ettner and Hermann (
8). The higher service utilization and costs of treatment among patients with multiple mental health diagnoses also support previous observations (
9,
10).
Several explanations may account for these observations. Liptzin and colleagues (
11) cited four factors—age, detection, labeling, and association—that might apply to any group of patients with mental illness. As noted above, patients with mental illness tended to be older. In part, higher health care costs might reflect the increased frequency of illness associated with aging. Detection refers to the increased likelihood that persons who encounter the health care system for one condition will be diagnosed as having others. Labeling refers to the hypothesis that people who are high users of services for any condition are considered hypochondriacs and are referred for psychiatric care. Association means that persons with physical disorders often have anxiety or depression or both.
An additional hypothesis is that poor access to or poor utilization of mental health services, particularly among persons with complex mental illness, may impair adherence to treatment plans, leading to poor symptom control, delays in seeking care for symptoms, or inappropriate utilization of high-cost services such as emergency rooms for physical illness. This hypothesis is supported in the data reported here in the proportionately high cost of non-mental-health care for persons with multiple diagnoses. The hypothesis might be tested through randomized trials offering aggressive, mental-health-oriented case management of persons with multiple diagnoses.
Conclusions
In summary, we observed several sources of variation in health care costs among Tennessee Medicare beneficiaries age 65 years and older. First, the three-year average annual health care costs of persons with mental illness were nearly twice the costs of persons without a mental health diagnosis. Second, considerable variation in costs for persons with different mental health diagnoses varied significantly: organic psychoses had the highest costs, while anxiety-phobias were about two-thirds less expensive to treat. Third, the cost for persons with multiple diagnoses was approximately 37 percent higher than the cost for persons with a single mental health diagnosis. However, most of the care received by persons with mental illness was for physical rather than mental health care—97 percent for those with one mental health diagnosis and 85 percent for those with more than one.
Because costs for care unrelated to mental health figured so prominently, we believe that policy makers should consider the hypothesis that among elderly Medicare beneficiaries, and possibly other populations, associations between mental illness and high health care costs might be partly due to too little rather than too much mental health care.
Acknowledgments
This study was supported by grants 20-C90705 and 20P-90889 from the Health Care Financing Administration, grant 2SO6-GM-08092-24 from the Minority Biomedical Research Support program, and grant R24-MH-59748-01 from the National Institute of Mental Health to Tennessee State University (Dr. Baqar Husaini, principal investigator).