Increases in the human life span over the course of the 20th century have contributed to marked shifts in demographic characteristics of the U.S. population. In 1900 only 39 percent of persons survived to age 65; in 2000, in contrast, 86 percent of individuals are expected to survive to age 65, and 58 percent are expected to survive to age 80 (
1).
The majority of these elderly individuals are expected to be women. Seventy-five percent of nursing home residents are women age 65 and older. Women constitute 72 percent of poor elderly people (
2). In addition to the psychosocial challenges of increased poverty, social isolation, and lack of adequate health insurance faced by a growing population of aging women (
3), it is believed that the physiological changes related to aging in women may have a profound effect on a variety of illnesses, including serious psychiatric disorders such as schizophrenia.
Although the number of elderly persons with schizophrenia is substantial and growing, little research has been conducted on schizophrenia in later life. Our understanding of the mental health care needs of this population is limited (
4) despite the substantial use of health care resources by older adults with serious mental illness (
5). Some investigators have reported a gradual lessening of severity of positive symptoms and a worsening of negative symptoms of schizophrenia in later life (
6,
7,
8,
9). None of these reports specifically addressed older women with schizophrenia. The literature on how aging affects illness among women with schizophrenia is particularly limited (
9,
10). Lindamer and associates (
9) reported that women over age 45 may develop more severe positive symptoms than older men.
The main age range of risk for developing schizophrenia for men is 20 to 35 years, and on average women develop the illness three to four years later than men. A second peak of onset of illness in women is seen at menopause (
11). The average age of menopause in the general population is around 51 years, and women who smoke undergo menopause about two years earlier on average than nonsmokers (
12). It has been suggested that estradiol functions as a dopamine antagonist (
13) and has a protective effect in schizophrenia (
14). The decrease in estrogen levels seen in menopause may be associated with increased dopaminergic activity and worsening of psychotic symptoms. Salokangas (
15), examining more than 300 new-onset cases of schizophrenia, reported that hospital admissions for psychotic disorders increased in women at menopause and in the postmenopausal years. Some clinical investigators have reported that postmenopausal women are less responsive to neuroleptic medications and less tolerant of their adverse effects (
16).
The available data on manifestations of schizophrenia among older women suggest that symptoms of illness for them may be worse than for younger women with schizophrenia. However, it is not clear how this difference affects other components of care and treatment outcomes such as global functional level and resource utilization.
This study is a comparative age-related analysis of length of hospital stay and pharmacological treatment of women with serious mental illness discharged from an acute care state mental health facility over a one-year period.
Methods
A computer search was undertaken of all patients discharged from a large urban state mental health facility over a one-year period from July l, 1997, to June 30, 1998. This facility treats about one-third of all patients who are hospitalized in the state system each year. Generally the patients admitted to the facility have serious mental illness and few financial resources. They are referred, frequently in crisis, by their local community mental health agency or local emergency department.
Data were obtained from the hospital database on patient characteristics, hospital discharge diagnosis, and length of stay. Pharmacy records were analyzed to determine prescription information at hospital discharge. Antipsychotic medication dosages were converted to chlorpromazine equivalents (
17).
First the female and male groups were compared. Mean length of stay was compared for the two groups using t test analysis, and the proportions of patients age 50 and older versus those under age 50 were compared using chi square analysis. The female sample was further assessed for demographic data, length of stay, comorbid substance abuse, and pharmacologic treatments. Length of stay was compared for older women (N=72) and younger women (N= 492) using t test analysis, and psychiatric diagnoses were evaluated as proportions using chi square analysis. Pharmacological treatment was assessed for the 72 older women and a computer-generated list of 72 randomly selected younger women. Comparisons of mean chlorpromazine equivalents were made using t test analysis, and of use of atypical antipsychotic medications using chi square analysis.
Results
Whole sample characteristics
A total of 1,358 persons were discharged from the facility over a one-year period. Of these, 564, or 41.5 percent, were women. Most of the patients were under age 50 (N=1,239, 91.2 percent), and 492 of these, or 39.7 percent, were women. Of the 119 patients age 50 and older, 72, or 60.5 percent, were women. The difference in proportions of older women and older men hospitalized was statistically significant (χ2=18.9, df=1, p=.001).
Once hospitalized, women patients had a greater length of stay on average (mean±SD=16.1±26.3 days) than male patients (10.2±14.2 days; t=5.2, df=1,362, p<.001). However, among patients age 50 and older, the difference in hospital length of stay between women and men was not statistically significant (23.2±23.7 days 20.5±33.2 days, respectively).
Women patients
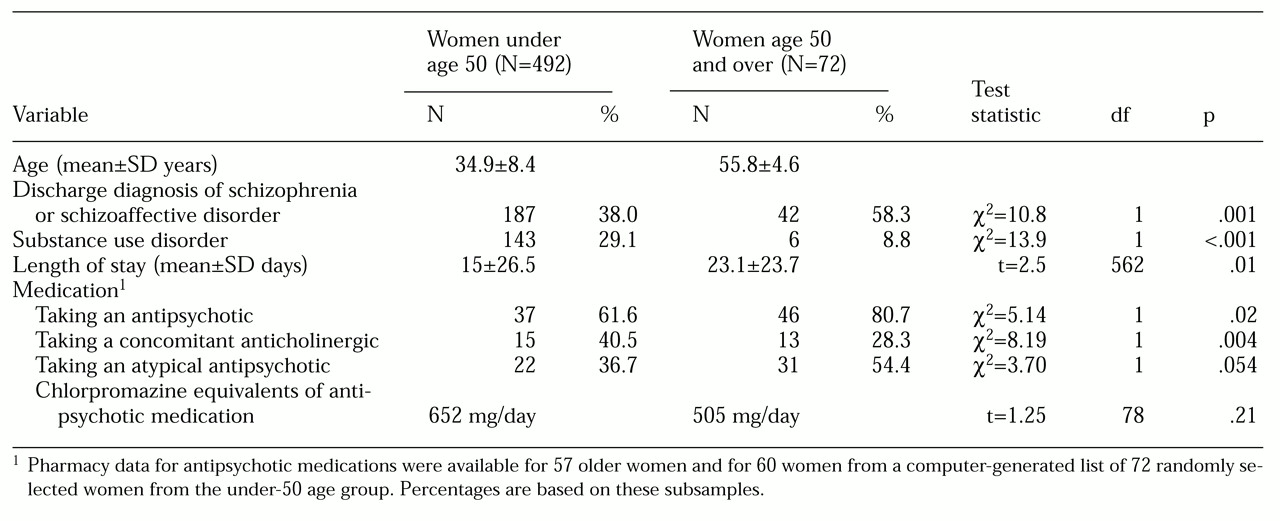
The clinical variables for hospitalized women are summarized in
Table 1. The mean±SD age of the women under 50 in our sample was 34.9±8.4 years, with a range of 17 to 49 years; the mean age of those 50 and older was 55.8±4.6 years, with a range of 50 to 71 years. Only two women were over age 65. Women in the older group had significantly longer hospital stays than their younger counterparts (mean of 23.1 days versus 15 days).
The proportion of women with a primary psychotic illness was significantly greater among the older women. In this group, 58.3 percent had a discharge diagnosis of schizophrenia or schizoaffective disorder, compared with only 38 percent of the younger women. Among other diagnoses in the older group, bipolar disorder figured prominently (N=21, 29.2 percent); one patient had a primary diagnosis of a substance use disorder, two of adjustment disorder, and six (8.3 percent) of other or unknown disorders. Among the younger women, a similar proportion had a diagnosis of bipolar disorder (N=148, 30.1 percent), 11.4 percent had a primary diagnosis of a substance use disorder (N=56), 11 percent had an adjustment disorder (N=54), and 9.5 percent had other or unknown disorders (N=47).
Substance abuse overall was fairly common among the younger women, with 29.1 percent having either a primary or secondary diagnosis of substance abuse (N=143), compared with only 8.8 percent of the older women (N=6).
Pharmacy records were available for 57 of the 72 older women and for 60 of the women in the computer-generated list of 72 younger women. A significantly greater proportion of the older women were receiving an antipsychotic medication compared with the younger women (80.7 percent versus 61.6 percent). The difference in the chlorpromazine-equivalent daily dosage between the two groups was not statistically significant.
The data suggest that atypical antipsychotic medications were more likely to be prescribed for older women than for younger women (54.4 percent versus 36.7 percent), although the difference was not statistically significant at the .05 level. Finally, concomitant anticholinergic medications were less likely to be prescribed for older women than for younger women.
Discussion
This study is limited by its retrospective nature, the small sample size, and the absence of any formal assessment of the severity of psychopathology. Hospital admission and length of stay were used as proxy measurements of severity of illness, but these factors may be influenced by a variety of nonclinical variables. Despite these limitations, cautious interpretation of the data is warranted, particularly given that the manifestations of serious mental illness in older women have been understudied.
Our data suggest that women under age 50 with serious mental illness have fewer psychiatric admissions than men of the same age group with serious mental illness. It has been reported that the global outcome of schizophrenia appears to be better for women than for men, and that women with schizophrenia generally have a better course of hospital treatment, shorter hospital stays, and less likelihood of relapse after hospital discharge (
17,
18,
19,
20,
21).
However, our data suggest that older women hospitalized in a state psychiatric facility were more seriously ill than younger women and men. Among persons age 50 years or older, older women constituted a significantly greater proportion of hospital admissions. Joseph and associates (
22), in a large Canadian study of health service use, reported that rates of hospitalization were highest in communities with a substantial relative concentration of elderly women. Both psychiatric diagnosis and comorbid medical disorder may affect length of stay. Although we did not obtain data on medical disorders, nearly 60 percent of the older women in our sample had schizophrenia.
It has been suggested that there is a gender bias in epidemiological studies of schizophrenia (
22) and that many studies, with an upper age limit of 44 years, exclude a greater proportion of female than of male schizophrenic patients. Thus many studies of schizophrenia tell us little about the manifestations and outcomes of illness among older women. Lindamer and associates (
9) have reported that a significantly greater proportion of women than men have late-onset schizophrenia. Unfortunately, our data do not include age of onset.
It is possible that these older women had more severe psychotic illness and that they were less responsive to drug treatments. Although significantly more older women than younger women in our sample received an antipsychotic medication, this pattern may have been due to the greater proportion of patients with schizophrenia in the older group. Both younger and older groups received substantial and similar doses of antipsychotic medication. More older women than younger women received atypical antipsychotic drugs, possibly because of intolerance of or suboptimal response to conventional antipsychotic agents. Pharmaceutical company marketing strategies also may have played a role in prescribing patterns. Antipsychotic therapy among older adults with primary psychotic illness has not been well studied, and the data available on chronically psychotic older women are particularly scarce.
Conclusions
Given the aging of the population in the United States, it will become increasingly important for clinicians and administrators to make provisions for the focused care of older women with serious mental illness. In this study, women constituted the majority of older seriously mentally ill persons hospitalized in a large state psychiatric facility. Their hospital stays were significantly longer than those of their younger counterparts, and the data suggested a trend for more use of atypical antipsychotic medications.
It is possible that medication interventions more specifically focused on older women could have led to shorter hospital stays—for example, more aggressive use of atypical antipsychotic medications in a population prone to extrapyramidal side effects. Some investigations have suggested that estrogen replacement therapy may be beneficial for treatment of schizophrenia among postmenopausal women (
23). Failure to address age-related issues in the treatment of seriously mentally ill women may have significant humanitarian and financial costs.