Editor's Note: In this article, which was first published in the March 1998 issue of Psychiatric Services, Dr. Geller and his coauthors describe how Massachusetts contracted with a private vendor in 1992 to manage behavioral health care for Medicaid beneficiaries. The vendor had a state network of 57 hospitals that agreed to accept a lower daily rate. Patients needing hospitalization could be sent up to 50 miles to an available bed. Data from 1992 to 1995 indicated that patients who were admitted to many different hospitals had longer lengths of stay than those admitted to hospitals where they were known. The authors describe the subset of patients who experienced discontinuity in treatment as a result of the managed care program.
Objective: The study examined the characteristics of frequent users of inpatient treatment under public-sector managed care in Massachusetts between 1992 and 1995 and explored whether their pattern of inpatient utilization affected their overall use of hospital days. Methods: Individuals with five or more admissions in any of four fiscal years (1992 to 1995) were identified using the Massachusetts Department of Mental Health client tracking system. The demographic and clinical characteristics of these patients and the types of hospitals they used were compared with those of all patients in case management programs who had a hospital admission but who did not meet study criteria for multiple admissions. Results: Compared with other patients, patients with multiple admissions were more likely to be young Caucasian females with personality disorder and a history of substance abuse but not a current substance use disorder. They tended to be lower functioning as measured by the Georgia Role Functioning Scale (GRFS) and to have higher levels of distress, as measured by the global personal distress portion of the GRFS. They made up 6 to 8 percent of all clients with a psychiatric admission who were enrolled in a case management program, but they accounted for 21 to 27 percent of all admissions in the four fiscal years. Patients with multiple admissions had significantly longer lengths of stay when admitted to a hospital where they had not been previously admitted in the past 12 months. Conclusions: States setting up public-sector managed care or revising existing public-sector managed care contracts should ensure that subpopulations of persons at high risk for multiple admissions receive special attention. They should also create networks of inpatient providers to enable frequent users of acute care facilities to return to the same facility that previously discharged them.
The last 50 years have witnessed major efforts to transform the organization and financing of inpatient services for persons with severe and persistent mental disorders. The first of these efforts, deinstitutionalization, resulted in dramatic reductions in the use of institutional care. More recently the locus of treatment has been shifted from institutional settings to privately operated general hospitals. This trend toward the privatization of inpatient mental health services has been driven chiefly by the desire of state mental health authorities to shift more of the cost of treatment to the federal government through the Medicaid program (
1). But the need to control increases in Medicaid expenditures beyond such cost shifting has brought about yet another reform in the organization and financing of mental health services—public managed care.
Attempts to reform the mental health system often solve certain existing problems, while other problems remain and new ones emerge (
2). Common to all the systemic reforms mentioned is the failure to solve basic problems posed by the chronicity of severe mental disorders. Another common sequela to system changes is the unintended but often highly problematic alteration in patterns of use of inpatient services by persons with severe and persistent mental illnesses. This paper draws on data from Massachusetts' experience with public-sector managed care to examine the nature of changes in utilization of inpatient psychiatric care and their implications for the use of managed care principles in systems delivering managed, Medicaid-funded services to persons with severe mental illness.
Background
Before the 1950s, state hospitals housed a significant number of patients who had been hospitalized for a decade or more, and stays of several years were not uncommon (
3). Beginning in the 1960s and 1970s, reforms of statutes governing the involuntary detention of patients in state hospitals, the advent of community-based care, and the development of more effective psychotropic medications all facilitated the process that has come to be called deinstitutionalization. One facet of this process was a significant reduction in the average length of stay in psychiatric facilities (
4).
Despite changes in mental health laws and policies, as well as improved treatments for mental disorders, the persistent course of many major mental disorders remained constant. But what did change was how this chronicity manifested itself in patterns of use of inpatient treatment. In the 1980s, researchers observed that in the aftermath of deinstitutionalization, state hospital patients could be assigned to three categories based on length of stay: old long-stay patients, new long-stay patients, and short-stay patients (
5).
One of these groups included patients who had never stayed long in psychiatric hospitals and who became part of a new and problematic subpopulation of persons with severe mental illness, categorized variously as "young adult chronic patients" (
6) and "rapid recidivists" (
7). In essence, the interventions and policies associated with deinstitutionalization had exchanged the excessively long hospitalizations of a previous generation for what many saw as an equally undesirable pattern of multiple short admissions amid cycles of decompensation and remission.
Concurrent with reductions in state hospital use was an attempt to shift greater proportions of inpatient episodes to local general hospitals. The attractiveness of such a shift was based largely on the potential cost savings from the Medicaid reimbursement obtainable for treatment in these facilities but not available for treatment provided in state hospitals. In addition, general hospitals were seen as clinically superior, less institutional, more community oriented, and less stigmatizing than the state hospital (
8).
The result of this effort was yet a further fragmenting of care, generating multiple treatment episodes at multiple sites. The treatment career of the pseudonymous Sylvia Frumkin has been the focus of Susan Sheehan's journalistic account (
9), a later economic analysis by Moran and colleagues (
10), and an extension of that work by Nicholson and colleagues (
11). Each of these publications describes chronic careers as spanning a patchwork of inpatient settings, including state mental hospitals, private psychiatric facilities, and local general hospitals. In a more recent study of psychiatric admissions in Massachusetts, Geller (
7) showed that the ideological imperative to admit persons "anywhere but the state hospital" often led to referrals of patients in crisis to hospitals several counties and many miles away from their homes, and further away than the state hospital.
The potential for intensifying this fragmentation and discontinuity of care was increased by the structural approach adopted in implementing Medicaid managed mental health care in Massachusetts. In 1992, in an effort to simultaneously increase the use of private settings for inpatient care and curb the explosion in Medicaid expenditures that would accrue from such a shift, Massachusetts contracted with a proprietary managed care vendor, Mental Health Management of America (MHMA), to manage its Medicaid behavioral health accounts. Among the strategies MHMA used to achieve cost containment was the development, through a competitive bidding process, of a statewide selective contracting network of hospitals for serving Medicaid beneficiaries.
The 57 hospitals that won these contracts each agreed to a negotiated daily rate and to acceptance of all patients approved for inpatient services by the MHMA precertification process. In return, the hospitals in the network obtained exclusive access to the Medicaid psychiatric market. Under the regulations established by MHMA, a Medicaid beneficiary precertified for inpatient services could be referred to any network hospital within a 50-mile radius of the screening site that had an available bed.
In essence, then, the selective contracting network behaved as a single-provider entity with multiple sites scattered across the state (
12). The question we address in this paper is whether, in its pursuit of controlling utilization and costs, managed care, like earlier reforms, has created new and problematic utilization patterns for the most intensive users of inpatient treatment.
Methods
We used data from the Massachusetts Department of Mental Health client tracking system, which includes demographic, clinical, and service use data for all department case-managed clients statewide. These data contain records of state hospital admissions as well as information on general, private, and other psychiatric admissions. Through the use of patient identifier codes, the system can support longitudinal, client-level analyses of service use. The data used in the analyses reported here reflect admissions that occurred in Massachusetts during fiscal years 1992 through 1995 (July 1, 1991, to June 30, 1995).
The focus of this study is the heavy user of inpatient services. Using data from the client tracking system, we identified a population with five or more admissions in any one of the four fiscal years (1992 to 1995). To be included in the study, a patient had to have five or more admissions in any year, but once the patient was in the observed sample, the patient remained so for the duration of the study regardless of the number of admissions in subsequent fiscal years.
We compared the clients with multiple admissions with other case-managed clients who had an admission but did not meet our criterion of multiple admissions. We examined patients' characteristics as well as the types of hospitals to which they were admitted across the four years.
For each admission, we identified whether the hospital was one to which the patient had been admitted within the past 12 months or whether it was a new site of treatment for that patient. For each fiscal year we then compared length of stay for same-site readmissions with length of stay for admissions to new treatment sites using, first, only admissions in the first year the patient had five or more admissions, and, second, all admissions during or after the year the patient had five or more admissions.
Results
Characteristics of patients with multiple admissions
A total of 652 patients (8.9 percent of the 7,293 adults with admissions in the study period) had five or more admissions in at least one of the four fiscal years and thus met criteria for inclusion in the analysis.
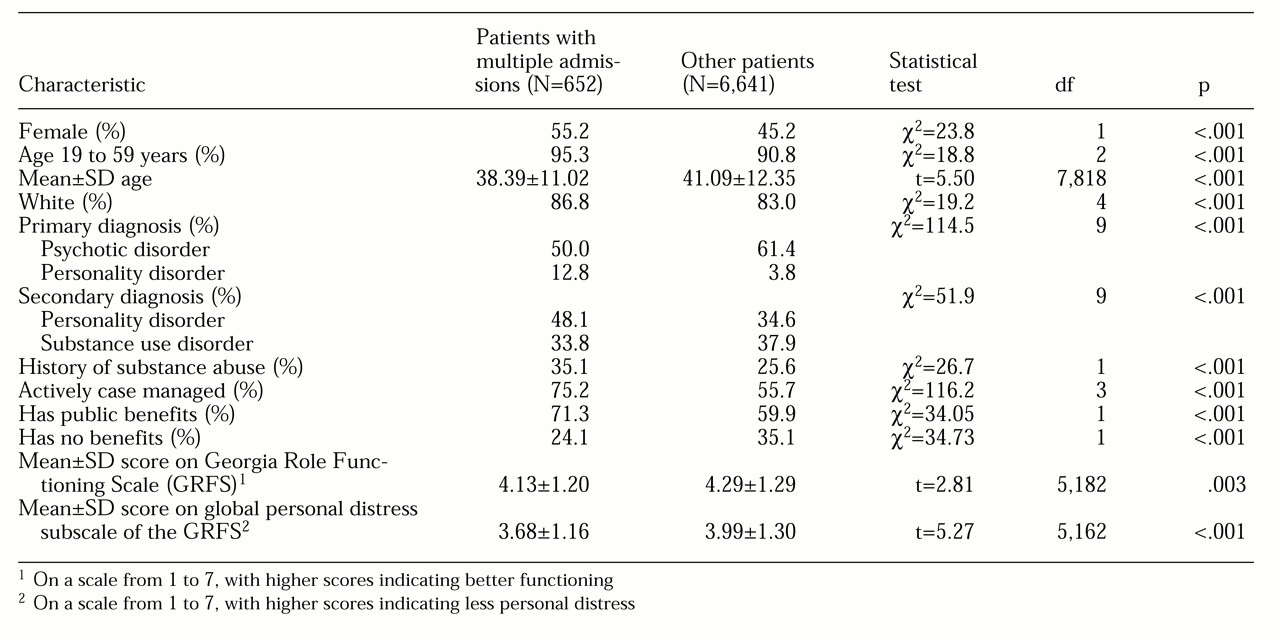
Table 1 shows the statistically significant comparisons of characteristics of patients meeting these criteria and those of patients without enough admissions to be included in this group. Frequent users and their counterparts were compared on more than 20 factors. Most comparisons between groups were not statistically significant, including marital status, frequency of patient-family contact, and whether an individual had a history of fire setting or sexual offenses, was on parole or probation, had a dependent child, or had serious co-occurring medical conditions. Because the large number of comparisons undertaken increases the likelihood of a type I error (that is, rejecting the null hypothesis when it is correct), we set the alpha level at .01 instead of the conventional .05 for identifying significant differences between groups. Only comparisons meeting the criterion of p<.01 are reported in
Table 1.
Patients with multiple admissions tended to be younger and were more likely to be Caucasian and female and have a diagnosis of personality disorder. Patients with multiple admissions were also more likely to have a history of substance abuse but less likely to have an active diagnosis of a substance use disorder. They also were more likely to have public benefits and less likely to have no benefits. The two groups were equally likely to have private benefits.
Patients' functioning was measured using the Georgia Role Functioning Scale (GRFS) (
13). The GRFS is a functional assessment instrument consisting of four scales and a subjective measure of personal distress. The scores on the four scales of functioning are summed to give a GRFS index. The global personal distress scale is reported separately. The GRFS was administered to the population annually.
Patients with multiple admissions tended to be lower functioning, as measured by their scores on the GRFS, and to have higher levels of distress, as measured by their scores at last assessment with the global personal distress portion of the GRFS. The two groups did not differ in education or mental status.
Patients with multiple admissions had a total of 7,911 admissions over the observation period. Just under half of these admissions (3,511, or 44.4 percent) were to facilities that were new to the patient in the past year, that is, to sites where the patient had not been admitted for at least one year.
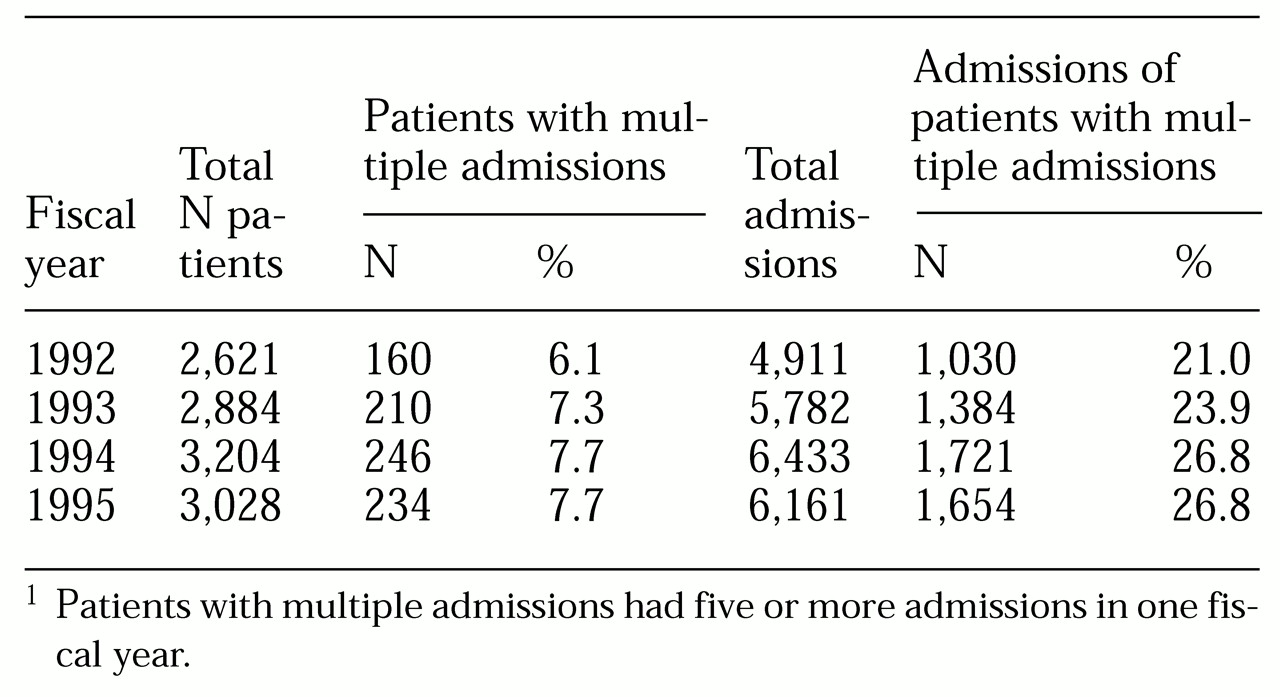
The percentage of all case-managed clients having five or more admissions in each fiscal year is shown in
Table 2.
Table 2 also shows the percentage of all admissions accounted for by these patients. Several patients had five or more admissions in more than one year, and thus they are represented in the data from more than one year.
As expected, the patients with five or more admissions constituted a small percentage of the total number of patients seen in any given year (6.1 to 7.7 percent), but they accounted for almost one-quarter of all admissions in those years (21 to 26.8 percent). Analysis of utilization trends showed an increase in the actual number of patients and in the percentage of patients admitted in fiscal year 1993. These increases continued in fiscal year 1994 but leveled off in fiscal year 1995. The number of admissions increased as well.
Continuity of treatment sites
The data also show differences in hospitalization sites between patients with multiple admissions and other patients in case management programs. Compared with patients who did not have multiple admissions, those with multiple admissions were less likely to have been hospitalized in a state hospital, were more likely to have gone to a general hospital (with a psychiatric unit or scattered beds for psychiatric patients), and were about equally likely to have gone to a private psychiatric hospital or other psychiatric hospital.
For patients with multiple admissions, state hospital admissions decreased rather dramatically over time. However, admissions to state hospital replacement units increased, although this increase was not equivalent to the drop in state hospital admissions. (The replacement units consisted of general hospital psychiatric beds with funding guaranteed by the Department of Mental Health. They provided the acute inpatient services formerly provided in state hospitals that have been closed.)
Patients having had multiple admissions started out in fiscal year 1992 with a much lower percentage of admissions to state hospitals than did patients without multiple admissions. This percentage decreased in the next three fiscal years by about 20 percent—virtually the same decrease in state hospital admissions experienced by patients without multiple admissions. Admissions to replacement units by patients without multiple admissions increased for two years before leveling off in fiscal year 1995, while admissions of this type for patients with multiple admissions continued to increase in 1995. For patients with multiple admissions, the level of general hospital use started higher in fiscal year 1992 than for patients without multiple admissions (34.8 percent, compared with 31.4 percent) and increased each year (to 40.1 percent), while admissions for patients without multiple admissions remained basically stable across the four years. (Differences in levels across years were not tested for significance because we compared the two groups' use of each hospital type for each year.) The two groups differed significantly on admissions to these hospital types in all four years.
For private hospitals and other types of hospitals, the proportion of admissions by patients with multiple admissions increased rapidly between fiscal year 1992 and 1993—from 11 to 22.1 percent in private hospitals and from 3.9 to 6.7 percent in other types of hospitals—and then gradually declined to 16.6 percent in private hospitals and 3.8 percent in other hospitals. For patients without multiple admissions, the proportion of admissions to private hospitals increased from 11.1 to 19 percent in the first fiscal year and then remained stable over the next three years. The proportion of admissions to other types of hospitals for patients without multiple admissions remained basically stable over all four years, ranging from 3.8 to 4.2 percent.
Length of stay and type of admission
The mean number of days per admission for patients with multiple admissions decreased over time, from 33.4 days in fiscal year 1992 to 18.8 days in fiscal year 1995. The mean number of hospitals used per year by patients with multiple admissions remained stable over the four years, ranging from 3.1 to 3.4.
A total of 3,511 admissions were to sites that were new to the patient, that is, sites where the patient had not been admitted within the preceding 12 months. Nearly 90 percent of the admissions to new sites were to hospitals where patients had never before been treated. The remaining admissions to new sites were actually readmissions, but more than 12 months had passed since the patient's last admission.
It should be noted that readmissions in the first fiscal year of the study (1992) were probably undercounted due to the absence of data for fiscal year 1991. Thus if a patient had been discharged from a hospital in fiscal year 1991 and readmitted in fiscal year 1992, the admission was coded as "new" in the 1992 data.
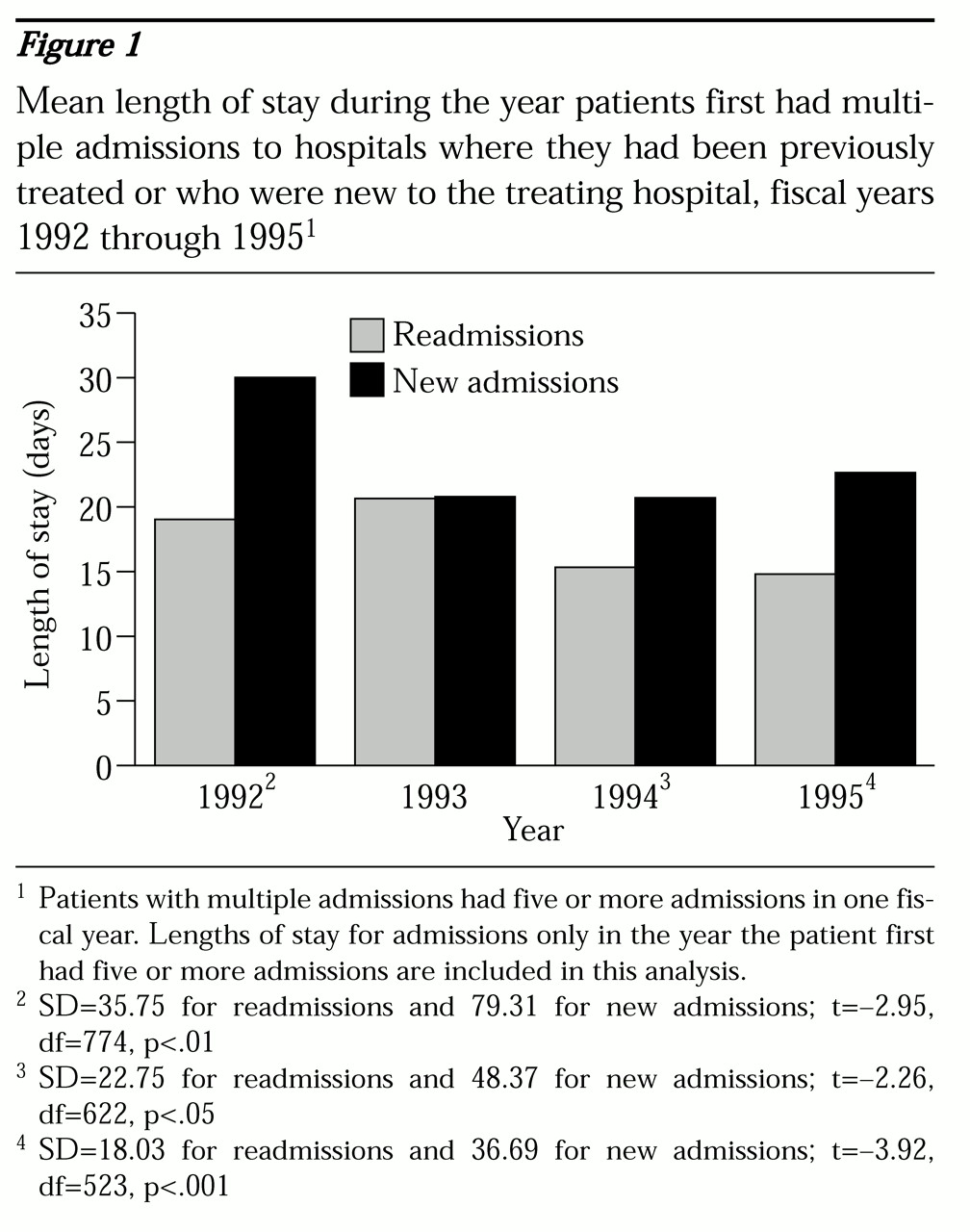
For each fiscal year, we compared the mean length of stay for patients with new admissions with the mean length of stay for patients who were readmitted. The initial analysis used patients' length-of-stay data from only the first fiscal year in which they had five or more admissions.
As
Figure 1 shows, mean length of stay for new admissions and readmissions in 1992 differed by more than ten days. However, as noted, most admissions in fiscal year 1992 were labeled "new" because data for fiscal year 1991 were not available. In fiscal year 1993, this difference no longer existed, due primarily to a reduction in length of stay for admissions to new hospitals. This reduction, in turn, is undoubtedly the result of proper identification of new admissions and readmissions made possible because data for 1992 were available for comparison with those for 1993.
The difference between new admissions and readmissions had grown to 5.5 days in fiscal year 1994 and to more than a week (eight days) by fiscal year 1995. Thus after the implementation of public managed care in 1992, readmissions to the same hospital resulted in increasingly shorter lengths of stay, while admissions to new facilities, where patients were unknown, resulted in increasingly longer lengths of stay.
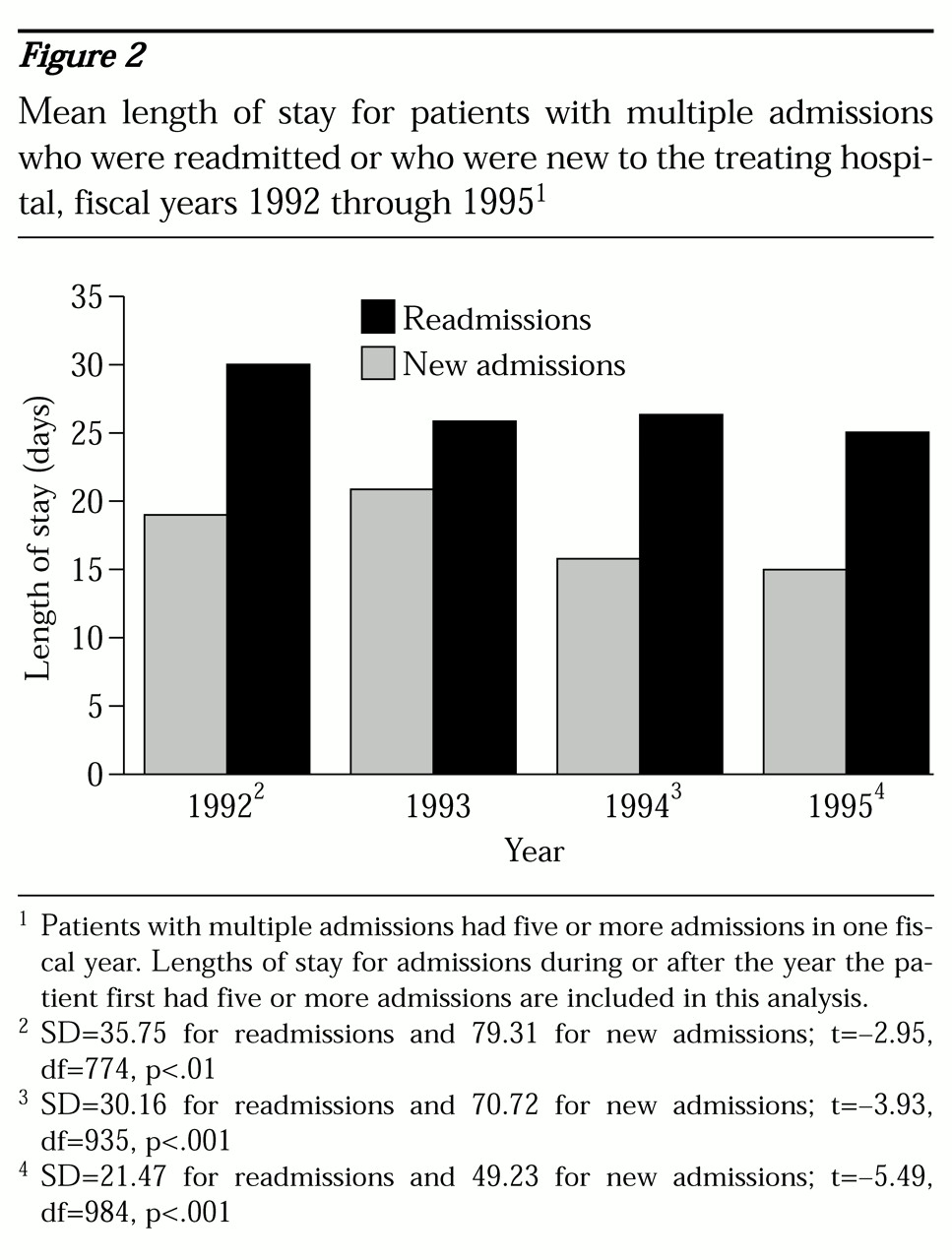
If we add to this analysis admissions for patients in the years following the first year in which they had five or more admissions, the difference between admissions to new sites and readmissions is even more pronounced in each year (see
Figure 2). A comparison of
Figures 1 and
2 suggests that the statistically significantly longer lengths of stay of patients with admissions to new facilities are due primarily to sustained increases in length of stay associated with this group, rather than to the readmission group's decreases in length of stay, which are influenced by managed care.
Trends in multisite admissions
The number of patients with five or more admissions increased over time, and their number of admissions likewise increased. The number of hospitals visited by this group declined, but only slightly. The continuity of admission site for this group increased, as measured by the number of patients who were admitted to hospitals where they had previously been treated. This increased continuity may well be due to the fact that the pool of hospitals to which any individual is likely to be admitted is finite and ultimately will be exhausted by persons who are frequently hospitalized. Furthermore, emergency prescreening teams made some effort to provide continuity on successive admissions. Whatever the cause of this increased continuity, however, readmission resulted in a decline in length of stay.
Discussion and conclusions
The results indicate that in the era of public-sector managed care, frequent users of inpatient psychiatric treatment tend to be younger Caucasian females with personality disorder and a history of substance abuse, but not an active substance use disorder. This profile does not differentiate them from public-sector inpatient recidivists before the advent of public-sector managed care (
14,
15), and the similarity suggests that managed care has not significantly affected this population's use of inpatient beds.
The results also show that patients with multiple admissions represent only 6 to 8 percent of all patients in case management programs who have a psychiatric admission within a given year, but they account for 21 to 27 percent of all psychiatric admissions by hospitalized case-managed patients in each year. Patients with multiple admissions who are admitted to many different hospitals have longer lengths of stay than those who are admitted to hospitals where they are known. Although these relationships may have seemed intuitively true, they are clearly demonstrated by our data.
These findings indicate that a subset of Medicaid beneficiaries whose mental health care was managed by a vendor contracting with Massachusetts exhibited a service use pattern that clearly ran counter to the goals of public managed care. For patients with multiple admissions, gaining access to the vendor's selective contracting network of hospitals often led to extreme discontinuity of treatment site. Because of this discontinuity, inpatient clinical staff had to become acquainted with the needs of patients whom they had not previously seen, and case managers, family members, and others involved in the discharge process had to learn the practices and procedures of new inpatient settings.
The result of this discontinuity was that the subpopulation of frequent users of inpatient services, long the bane of the public mental health system, presented new challenges and experienced a paradoxical managed care outcome: extended lengths of stay. The trends observed in these data suggest that for individual patients this effect might be transitory, as frequently admitted patients exhaust the range of hospitals to which they can be admitted. Nevertheless, as new frequent users enter the system, the phenomenon described may become a persistent feature of a system in which selective contracting with general hospitals that have limited bed capacity is the model for implementing public managed care.
In assessing the data presented here, we must be careful in the way we ascribe causal relationships. First, it is important to emphasize that it is not the generic practice of managed care that is directly responsible for the patterns of hospital use we describe. Rather, these patterns would appear to be attributable to the use of a selective contracting network as a means for operationalizing managed care.
It must also be noted that the mental health policy and services environment in Massachusetts was marked by considerable foment at the time our data were collected. Coincident with the introduction of public managed care, a number of state hospitals were closed, and large numbers of individuals were added to the Medicaid roles. Many such individuals thus became patients in the general hospital system for the first time. Any of these factors could have contributed to or intensified the discontinuities observed here, although none would seem to have been able to play as direct a role in generating the observed patterns as did the selective contracting network itself.
The evaluation of any policy intervention obviously requires examination of the extent to which the intervention succeeds in meeting its stated goals. However, thorough investigation requires that we look for unintended consequences or "externalities," both favorable and deleterious (
16). Evaluation of the Massachusetts experience with public managed care has revealed externalities of both kinds. The explicit goal of reducing Medicaid expenditures for behavioral health services was met early in the contract period, largely through reducing the use of inpatient treatment for substance abuse and through increased substitution of outpatient for inpatient treatment across the spectrum of Medicaid reimbursed services (
17).
As we noted at the outset, efforts at system reform often succeed at least partly in addressing the problems to which they are directed, but at the cost of creating or exacerbating other problems. The aggregate success of public managed care in Massachusetts as shown by the cost savings reported in earlier studies, together with the data reported here on the generation of a more expensive service use pattern for frequent users of inpatient care, is consistent with the "mixed-benefits" model of reform described by Morrissey and Goldman (
2).
The data reported here have important implications for planning. Two consequences arising from the use of selective contracting networks are the continuation of high hospital usage patterns by the most problematic subset of inpatient recidivists and discontinuity of treatment site leading to increased length of stays. These effects have important clinical and service system implications that must be addressed. For example, programs must be specifically tailored for female patients with borderline personality disorder who are identified as frequent users of inpatient services. Network hospitals should be assigned a specific cohort of frequent users who are their responsibility at all times.
Addressing such potential problems as high levels of hospital usage and discontinuity of treatment at the outset of public managed care should become part of any planning agenda for states implementing managed Medicaid psychiatric care and treatment. Such problems should also be addressed at contract renewal times for any states advancing their agenda of psychiatric coverage through managed public care.