The factors responsible for this transformation of loci of care and treatment are complex. One key element has been federal cost shifts accounted for by the Social Security Administration's policies on institutions for mental diseases (IMDs) over the past half century. An ostensibly simple effort by the federal government beginning in 1950 to require the states to maintain financial responsibility for their psychiatric state hospital populations turned out to fuel one of the most dramatic changes during the 20th century in the care and treatment of persons with serious mental illness.
This paper contrasts the intended effects of the IMD exclusion with its unintended consequences. It describes the foundation of the exclusion, beginning with Dorothea Dix's 19th-century campaign for better care of the mentally ill, and moves chronologically through the development of the exclusion and its outcomes. Highlighted throughout is the tension between fiscally driven policy and clinically desirable outcomes.
The 19th century
Dorothea Dix was an indefatigable reformer who campaigned state by state for improvements in the care and treatment of the "insane" (
6). She took her lobbying efforts to the federal level when she addressed the United States Congress on June 23, 1848 (
7).
In her address Ms. Dix said: "We have then 22,000 [insane or idiotic] to take charge of; a majority of whom are in needy or necessitous circumstances. … I have myself seen more than nine thousand idiots, epileptics, and insane, in these United States, destitute of appropriate care and protection; and of this vast and most miserable company, sought out in jails, in poorhouses, and in private dwellings, there have been hundreds, nay, rather thousands, bound with galling chains, bowed beneath fetters and heavy iron balls, attached to drag-chains, lacerated with ropes, scourged with rods, and terrified beneath storms of profane execrations and cruel blows; now subject to gibes, and scorn, and torturing tricks—now abandoned to the most loathsome necessities, or subject to the vilest and most outrageous violations."
Ms. Dix suggested a remedy: "No disease is more manageable or more easily cured than insanity; but to this end special appliances are necessary, which cannot be had in private families, nor in every town and city; hence the necessity for hospitals. … Under well directed hospital care, recovery is the rule, incurable permanent insanity the exception. … Humanity requires that every insane person should receive the care appropriate to his condition. … Hardly second to this consideration is the civil and social obligation to consult and secure the public welfare: first in affording protection against the frequently manifested dangerous propensities of the insane; and second, by assuring reasonable and skillful remedial care, procuring their restoration to usefulness as citizens of the republic, and as members of communities."
As for the source for her remedy, Ms. Dix said: "I ask, for the thirty States of the Union, 5,000,000 acres of land … [for all who] are wards of the nation, claimants on the sympathy and care of the public, through the miseries and disqualifications brought upon them by the sorest afflictions with which humanity can be visited."
Ms. Dix lobbied her land grants bill through the administrations of four presidents: James Polk, whose term ended in 1849; Zachary Taylor, who died in office in 1850; Millard Fillmore, whose term expired in 1853; and Franklin Pierce. The bill, with some modifications, such as increasing the acreage to 10,000,000, was passed by both houses of Congress during Pierce's term, in 1854. In a successful attempt to ensure that the states, not the federal government, would continue to pay for the care of seriously mentally ill citizens, President Pierce vetoed the bill.
President Pierce (
8) delivered a lengthy veto message on May 3, 1854. It first laid out the issues: "It cannot be questioned that if Congress has power to make provision for the indigent insane without the limits of this District it has the same power to provide for the indigent who are not insane, and thus to transfer to the Federal Government the charge of all the poor in all the States. It has the same power to provide hospitals and other local establishments for the care and cure of every species of human infirmity, and thus … the whole field of public beneficence is thrown open to the care and culture of the Federal Government."
The President then explained the basis for his veto: "If the several States, many of which have already laid the foundation of munificent establishments of local beneficence, and nearly all of which are proceeding to establish them, shall be led to suppose, as, should this bill become a law, they will be, that Congress is to make provisions for such objects, the fountains of charity will be dried up at home, and the several States, instead of bestowing their own means on the social wants of their own people, may themselves, through the strong temptation which appeals to states as to individuals, become humble supplicants for the bounty of the Federal Government, reversing their true relations to this Union."
President Pierce's predictions did come true, although it was 125 years before they did so.
1950 to 1989
The beginnings of what became the IMD exclusion can be found in the 1950 Amendments to the Social Security Act; in those amendments, patients in mental institutions were excluded from receiving federal payments for old-age assistance. The basis for this exclusion was clearly rooted in the states' historical provision of such care (
12).
This exclusion continued unchanged until the enactment of Medicaid under the 1965 Amendments to the Social Security Act. For the first time, states could use the formula for federal financial participation for a population in mental institutions—in this case those 65 years of age or older (
12). Other populations were not included because Congress again voiced its intention of leaving the care and treatment of those in psychiatric (mental) hospitals as the responsibility of the states (
12). Congress did, however, expand use of the federal financial participation formula to include services to the mentally ill in general hospitals.
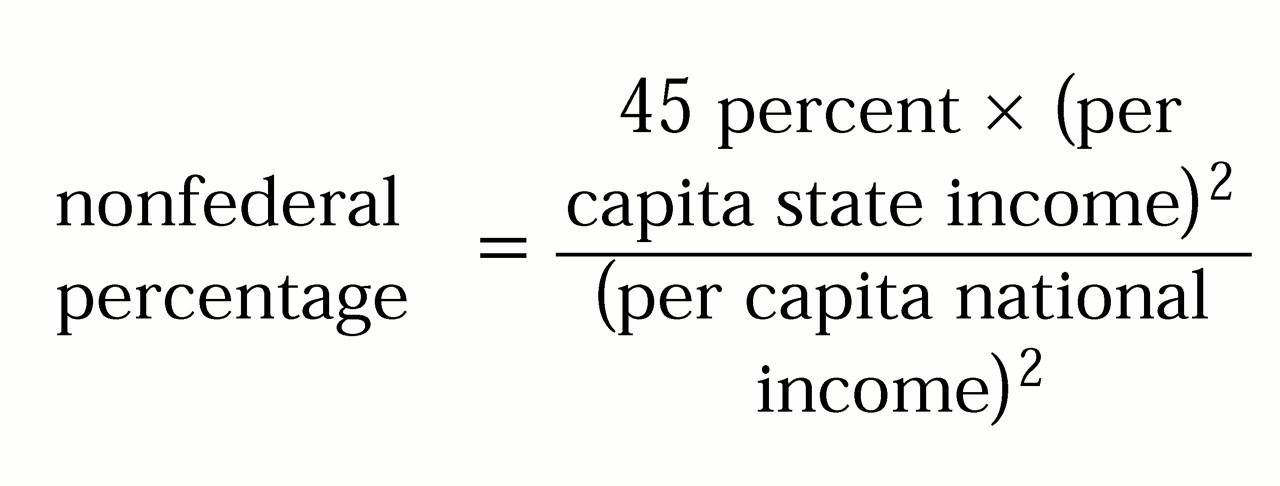
The 1965 changes to what became the IMD exclusion opened the first door for the states to begin to shift costs for the care and treatment of mentally ill persons to the federal government. In a state hospital, the state generally bears 100 percent of the cost of care and treatment. In any facility that is eligible for Medicaid reimbursement, each state pays considerably less than 100 percent, according to the federal financial participation formula:
As is clear from this formula, less-well-off states receive greater federal contributions. Historically, the range of federal participation in different states has been between 50 and 83 percent (
13).
Institutions for mental diseases were first officially defined in 1966, in the
Handbook of Public Assistance Administration (
12). This definition has been modified several times. According to the
State Medicaid Manual, a facility meets IMD criteria if its "overall character is that of a facility established and/or maintained for the care and treatment of individuals with mental diseases" (
14). Any one of the following criteria defines an IMD: the facility is licensed as a psychiatric facility, the facility is accredited as a psychiatric facility, the facility is under the jurisdiction of the state's mental health authority, the facility specializes in providing psychiatric-psychological care and treatment, or more than 50 percent of all the patients-residents in the facility require care because of mental diseases. One significant modification occurred in 1988, when Congress, as part of the Medicare Catastrophic Act (P.L. 100-360), indicated that a facility needed to have more than 16 beds to be defined as an IMD (
12,
15).
In 1971 Congress expanded Medicaid to include coverage of services rendered in intermediate care facilities through P.L. 92-223. In 1972 Congress, through P.L. 92-603, expanded federal financial participation for inpatient psychiatric treatment in facilities classified as IMDs to individuals under 21 years of age. Although a federal agency had defined IMDs in 1966, it was not until 1988 that Congress defined them, and not until the Omnibus Budget Reconciliation Act of 1990 (P.L. 101-508) that Congress expanded coverage for those under 21 years of age to facilities that were not hospitals.
A piece of legislation that might have altered the course of the IMD exclusion was the Mental Retardation Facilities and Community Mental Health Centers Construction Act (P.L. 88-164), signed into law by President Kennedy in 1963. The act was the result, according to some historians, of the propaganda about community-based care in the early 1960s, and it ignored much of the evidence that could refute the ideological bent of the time (
11). Some consider that the outcomes of this legislation make it one of Congress' more irresponsible social acts.
The statutory definition of IMD coverage remained largely unchanged between 1972 and the changes in 1988 noted above. However, the Department of Health and Human Services (HHS)—then the Department of Health, Education, and Welfare—was busy evaluating the proper application of the IMD exclusion by the states, disallowing certain states' practices and defending itself in court. The department's actions culminated in the Supreme Court's decision in
State of Connecticut Department of Income Maintenance v. Heckler (
16). The court unanimously found for HHS, holding that a hospital, a skilled nursing facility, or an intermediate care facility could be classified as an IMD. The court stated that the federal government's application of the IMD exclusion was consistent with congressional intent. To restate that intent: states, not the federal government, were responsible for citizens with chronic mental illness who were receiving long-term care and treatment in psychiatric facilities.
Thus by 1989 any residentially based program of more than 16 beds, no matter what its treatment modalities, its licensure, or the length of stay of its patients, could be classified as an IMD if it was engaged predominantly in delivering services to individuals with mental diseases. The states were given all the invitation they needed to serve as many individuals with mental diseases as possible in any facility that was not classified an IMD, thus providing incentives to move people out of state hospitals.
1990 to 2000
In the 1990s Congress continued to be curious about, if not befuddled by, the IMD exclusion. The Congressional Research Service's report on the
Medicaid Source Book (
15) reviewed the development and status of the IMD exclusion up to 1993. The report noted that the Omnibus Budget Reconciliation Act of 1987 (OBRA-87) (P.L. 100-203) authorized special waivers to allow demonstration projects funded by the Robert Wood Johnson Foundation, the results of which became widely available in 1990 (
17,
18).
Waivers that broaden the Medicaid population and redefine how they can be cared for, and hence give states further incentive to shift patients and costs to community-based care, have been granted to states through section 1915(b) program waivers and through section 1115 demonstration waivers (
19) under the Social Security Act. One of the few sections of a waiver that could have the opposite effect, and one rarely granted, allows states to receive Medicaid funds for the treatment of persons in state psychiatric hospitals. For example, Massachusetts received a waiver in 1997 allowing billing for 30 days per episode and 60 days per year of active treatment in its state hospitals (
20).
Another piece of legislation that had ripple effects on the IMD exclusion throughout the 1990s was the Medicaid law in OBRA-87. It requires states to make disproportionate-share payments to hospitals serving a disproportionate percentage of Medicaid and low-income patients (
15). Disproportionate-share payments have continued to irk Congress, particularly as they allow states to maximize their receipt of federal dollars through "creative financing" (
21,
22), and mostly through their recent use by states for IMDs (
22,
23).
The creative financing works like this: specialty hospitals can qualify as disproportionate-share facilities; state hospitals serve populations that meet criteria for disproportionate-share payments; thus states can apply for these payments—that is, federal dollars—even though patients do not qualify for federal dollars through Medicaid (
15,
23). States are thus able to increase their overall receipt of federal dollars by including state hospitals in their disproportionate-share hospitals.
One reaction by Congress has been a provision in the Balanced Budget Act of 1997 that creates a progressive deduction in disproportionate-share payments to facilities classified as IMDs between fiscal years 1998 and 2003. As of fiscal year 2003, states will be limited to using no more than 33 percent of their disproportionate-share payments for facilities meeting the IMD definition. This stipulation either will have no effects on states or will have major effects, depending on each state's current use of disproportionate-share payments for IMD-designated facilities. Such payments range across the states from 0 to 100 percent (
24).
This loss of revenue could be another derailment in rational treatment of persons with chronic mental illnesses who need long-term care. The financial incentives for the states to minimize the use of state hospitals for persons with chronic mental illness mounts as congressional interventions to thwart states' efforts to include the federal government as a payer in meeting the needs of this population increase.
One other legislative activity during the 1990s that is worth considering in relationship to the IMD exclusion is the quest for parity, the nondiscriminatory coverage of mental illnesses by third-party payers. Before President Clinton's health reform effort of 1993-1994, Senator Pete Domenici filed, on March 30, 1993, the Equitable Health Care for Severe Mental Illness Act of 1993. Stunned by the limits of coverage for a serious mental illness of a member of his immediate family, Senator Domenici has spent years in pursuit of improved coverage for mental illnesses. In 1993 his efforts were swallowed up by national health care reform.
In August 1993 the draft contents of President Clinton's Health Security Act were leaked. The material then appeared as a 239-page draft on September 7, as a 1,342-page draft on October 27, and as a 1,364-page bill on November 20. True parity was nowhere to be found. The mental illness benefit was a convoluted system of delimited benefits allowing for trade-offs of inpatient, residential, and outpatient days. Both the benefit itself and the copayment requirements worsened from the August draft through the November bill.
The Senate took the bill to two committees. The Labor and Human Resources Committee, the first to vote a bill out of committee, tinkered with the Clinton plan's mental illness and substance abuse coverage but made no fundamental movement toward true parity at that time. The Finance Committee, while not specifying any benefits, included full-parity language in its instruction about what the "benefits board" must provide. It was the first endorsement by a congressional committee of true parity, an event that occurred on Independence Day weekend in 1994.
While the Democrat-controlled 103rd Congress was busy with health reform, the minority party was not silent. Senate minority leader Robert Dole weighed in with his health bill on August 9, 1994. The Dole bill stated that the Secretary of Health and Human Services should give priority to providing coverage for mental health and substance abuse services that is equal to coverage for other medical services with respect to cost-sharing and duration of treatment. The Senate bills that followed—the Mitchell bill of August 12, 1994, melding the two Senate committee bills, and the Mainstream Proposal, the last-ditch effort of September 1994—also specified true parity.
Unfortunately, health care reform died, and parity at the federal level died with it.
Interested parties, such as the American Psychiatric Association, the Bazelon Center for Mental Health Law, the National Mental Health Association, and the National Alliance for the Mentally Ill, believed that even the provisions of the Clinton health care bill—and to a much greater extent the later bills with parity—would have had a profound impact on the IMD exclusion by extending benefits to all, independent of state hospital residential status (personal communications from representatives of these organizations, 1994).
The issue of a mental illness and substance abuse benefit was largely dormant in 1995 in the 104th Congress. The only bill to reintroduce the issue of true parity was put forward by Senate minority leader Tom Daschle. Senator Domenici again fought for benefits for those with serious mental illness, reintroducing on January 31 the Equitable Health Care for Severe Mental Health Act of 1995, cosponsored by Senator Paul Wellstone. Little was accomplished.
However, health care reform was not dormant. Senator Nancy Kassebaum, in a bill cosponsored by Senator Edward Kennedy, introduced first on July 13, and then by amendment on October 12, the Health Insurance Reform Act of 1995. This bill was aimed at addressing the issues of access to coverage and portability and renewability of coverage. The bill was amended in 1996 by a unanimous vote of the Senate to include a true parity provision, but the effort failed in conference committee. Insurance reform passed in late July 1996; parity had again disappeared.
Senators Domenici and Wellstone then introduced the Mental Health Parity Act of 1996. The contents of this bill became the basis for an amendment to H.R. 3666, the Veterans Affairs and Housing and Urban Development Appropriations Bill. This bill, signed into law by President Clinton on September 26, 1996, prohibits the imposition of annual and lifetime limits for mental illness coverage that are different from limits for other medical illness under private group insurance. The bill does not apply to individual policies, group policies of small businesses of 50 or fewer employees, Medicaid, Medicare, or substance abuse treatment. The bill does not require equal copayments, deductibles, utilization procedures, or even visit limits. It was a limited gain, and one that has had no impact on the IMD exclusion.
Pushing for more, Senators Domenici and Wellstone introduced the Mental Health Equitable Treatment Act of 1999 on April 4, 1999. This bill would have mandated full insurance parity for schizophrenia, bipolar and major depressive disorders, panic and obsessive-compulsive disorder, and other conditions considered to be severe and disabling. Full parity would have prohibited restrictions on annual and lifetime benefits, inpatient days, outpatient visits, and out-of-pocket expenses that were any different from those for other medical disorders. However, the legislation would have applied only to group health plans already providing mental illness benefits; small businesses with 25 or fewer employees would have been exempted. The legislation died.
Senators Domenici and Wellstone, now joined by Senator Kennedy, filed a bill on May 25, 2000, to modify the Public Health Services Act to involve the federal government in the betterment of services for persons with mental illnesses. This bill, entitled the Mental Health Early Intervention, Treatment, and Prevention Act of 2000, covers a remarkably wide range of needs and includes funds for both established and innovative programs. The bill addresses suicide prevention, stigma, emergency services, jail diversion, outreach, screening, integrated systems of care, and services for people with dual diagnoses of mental and substance use disorders. Research and training grants are funded, as are mental health courts, jail and prison services, and a compliance initiative.
On another front, at the White House Conference on Mental Health on June 7, 1999, President Clinton announced that the health insurance plan for federal employees—the Federal Employees Health Benefits Program—would be required to provide equal coverage for mental illnesses. This initiative represents a strong philosophical statement and a powerful model for other insurers, but it has a negligible effect on persons with chronic mental illnesses in IMD-designated facilities.
The parity fight has also progressed on the state level. Although more than half the states now have some form of legislation that advances toward parity, these initiatives have had little or no impact on citizens whose lives are significantly shaped by the IMD exclusion.
Another significant movement in health care reform during the 1990s was the progression of public-sector managed care. The effects of public-sector managed care have been confused with the effects of efforts to downsize or eliminate state hospitals in the context of the IMD exclusion. In states in which the movement to fewer or smaller state hospitals and the push to manage public-sector care have been largely concurrent, the interventions to accomplish downsizing have been thought to be causally linked to managed care (
25). In states far along toward depopulating state hospitals, it is clearer that public-sector managed care added little to the armamentarium to accomplish this goal (
26). The necessity of becoming innovative, creative, and sometimes manipulative in creating alternatives to state hospital care has been driven far more by the IMD exclusion than by public-sector managed care.
The consequencesof the IMD exclusion
The intended consequences of the IMD exclusion created by the federal government were—and apparently still are—that the states retain responsibility for their citizens with chronic mental illness who require long-term care in psychiatric settings. However, for too many individuals with chronic mental illness, the unintended consequences have been damaging.
The unintended consequences have contributed significantly to reshaping mental health policy since 1950. Since 1955 we have seen a massive transformation in the providers of psychiatric services and an equally massive translocation of the sites of psychiatric services. The movement has been from inpatient to outpatient settings and from public (state) providers to private providers (
27,
28,
29). If this is a first-level consequence, second-level consequences include the creation of an ideology, the development of an array of community-based services, and pronouncements about what "everybody knows" about care and treatment of persons with chronic mental illness.
Deinstitutionalization did not originate as a policy. Rather, it came about through a confluence of events, and thus it might better be referred to as a "happenstance" (
29). The cornerstone of this development may well be the identification after World War II of mental hospitals as "the devil to be exorcised" (
30). A fundamental motivation for deinstitutionalization was and is the fiscal incentive to provide care outside state hospitals—the IMD exclusion. But deinstitutionalization, even as a concept retrofitted for earlier events, has at best been poorly defined (
29). Even the concept of treatment "in the community" has had no agreed-on definition, unless it means "anyplace other than the state hospital" (
31).
Once the movement of deinstitutionalization was under way, there was a need for legal underpinnings. This situation gave birth to the right to treatment in the least restrictive alternative. Under this principle, federal courts became involved (
32), and entire systems of care and treatment were created (
33,
34). All these developments occurred even though "least restrictive alternative" didn't have—and doesn't have—a consistent definition, in either legal or lay terms (
35). The lack of definition of least restrictive alternative has not prevented progression to the more recent legal principle that individuals with chronic mental illness, under the penumbra of the Americans With Disabilities Act, have a right to services in "the most integrated setting appropriate to their needs" (
36). This concept, too, is without an operational definition.
The movement of individuals who needed mental health services from hospitals to other sites required the creation of a vast array of services. Although a discussion of these services is beyond the scope of this paper—they have been discussed elsewhere (
3,
29,
37,
38,
39,)—their outcomes have often been effective and humane. The question is whether they are appropriate for everyone (
40). What about persons whose level of violence might warrant institutional care (
41), or those who need the asylum functions of a traditional state hospital (
42,
43)? Again we encounter the states' financial disincentives to maintaining in a state hospital anyone they don't have to.
The federal government has been involved in the development of community services, even though it would appear to have little fiscal incentive to do so. Its involvement has been through agencies of the Department of Health and Human Services—first the National Institute of Mental Health; in 1973 the Alcohol, Drug Abuse, and Mental Health Administration; and in 1992 the Substance Abuse and Mental Health Services Administration (
44,
45,
46). This interest has been at the agency level, and Congress has expressed little direct interest in community services. It is unclear to what degree Congress' annual ambivalence about funding these agencies is attributable to Congress' perceptions of a progressive increase in federal participation in what should be the states' responsibilities.
Once community services were developed, they were linked to the philosophy or ideology of deinstitutionalization. Pronouncements were made about what "everybody knows" about community treatment; many of these pronouncements were subsequently called into question. Here are a few examples, each followed by a citation to a reference refuting it: patients' "institutionalized" behaviors such as poor motivation and blunted affect were entirely a function of exposure to institutional life (
47); individuals released from state hospitals would gradually gain competencies by moving through a graduated sequence of less intensive residential programs and then to independent and integrated living in the community (
48); treatment at local general hospitals and not at state hospitals would mean treatment closer to home and therefore treatment more integrated into local community resources (
49); and people outside of hospitals would receive care at least as humane as the care they received in hospitals (
50).
The translocation of care from state hospitals to alternatives was influenced by many factors. What evidence can be found of how powerful the IMD exclusion has been in this process? In almost all jurisdictions, the 16-bed rule has held. Hence the United States is dotted with small community residential programs and supported housing arrangements.
However, in the eighth judicial circuit—encompassing North Dakota, South Dakota, Nebraska, Minnesota, Iowa, Missouri, and Arkansas—as a result of the court case
Levings v. Califano (
51), IMD status is not determined by facility size. Rather, a person is not an IMD resident if the person resides in an institution voluntarily and pays all costs, or if the person who has insufficient funds pays all costs through Supplemental Security Income. As a result, community residential programs exceed the 16-bed limit. In Iowa, for example, residential care facilities for persons with mental illness have as many as 80 beds (personal communication, Templeman H, Iowa Division of Mental Health and Developmental Disabilities, Aug 4, 1998).