Substance use disorders are one of the most significant public health issues facing the United States (
1), costing taxpayers up to $276 billion a year (
2). More than 11 percent of American adults are affected by these disorders annually (
3), and an estimated five million Americans need drug and alcohol treatment (
4).
For many individuals with severe alcohol and drug problems, detoxification is the beginning phase of treatment. Without follow-up to an appropriate level of care, however, detoxification alone is an inadequate use of limited resources (
5). Detoxification is associated with lasting improvements only when patients receive continued rehabilitative care (
6,
7). As the Institute of Medicine reports, "Consistently, without subsequent treatment, researchers have found no effects from detoxification that are discernibly superior to those achieved by untreated withdrawal"(
7). Despite the importance of the issue, few studies have examined the rate and patterns of substance abuse treatment after detoxification. Existing studies focus primarily on the delivery of public services (
8,
9), yet the majority of illicit drug users and alcoholics are employed (
10). The private sector now accounts for as much as 41 percent of substance abuse treatment expenditures (
7,
11). These facts, coinciding with the dramatic growth of managed behavioral health care, have raised concerns about the potential impact of managed care on the quality of care for individuals with substance use disorders (
12,
13). More empirical evidence about drug and alcohol treatment in the private sector is needed to inform the discussion of these issues.
The goal of our research is to contribute to the understanding of care for substance use disorders in the private sector. We describe the rate of subsequent drug and alcohol treatment, as well as the duration and intensity of treatment once initiated, for inpatient detoxification patients in behavioral health care carve-out plans. We then explore how these outcomes are affected by benefit structure—copayment amount—after controlling for other variables that previous research suggests may be relevant (
5,
8,
14,
16).
Methods
We studied claims data from 14 employer groups whose behavioral health care benefits are managed by United Behavioral Health (UBH), the third largest managed behavioral health care organization in the country. More information about the full database and benefit design was provided by Sturm and McCulloch (
17). Patients were selected if they had received inpatient detoxification services between 1991 and 1997, their coverage continued for at least three months following the inpatient stay, and their employer plans covered a full range of behavioral health services, including detoxification, substance abuse, and mental health treatment.
Patients with alcohol-related problems were authorized for detoxification if they had a Clinical Institute Withdrawal Assessment (CIWA) score of 15 or greater (
18) or were otherwise at significant risk for withdrawal. Patients with problems not related to alcohol were not assessed using a specific scale. Instead, they were authorized for detoxification if they were clinically judged to be at a similar risk for physiologic withdrawal, or if their cases were complicated by other factors or comorbid conditions.
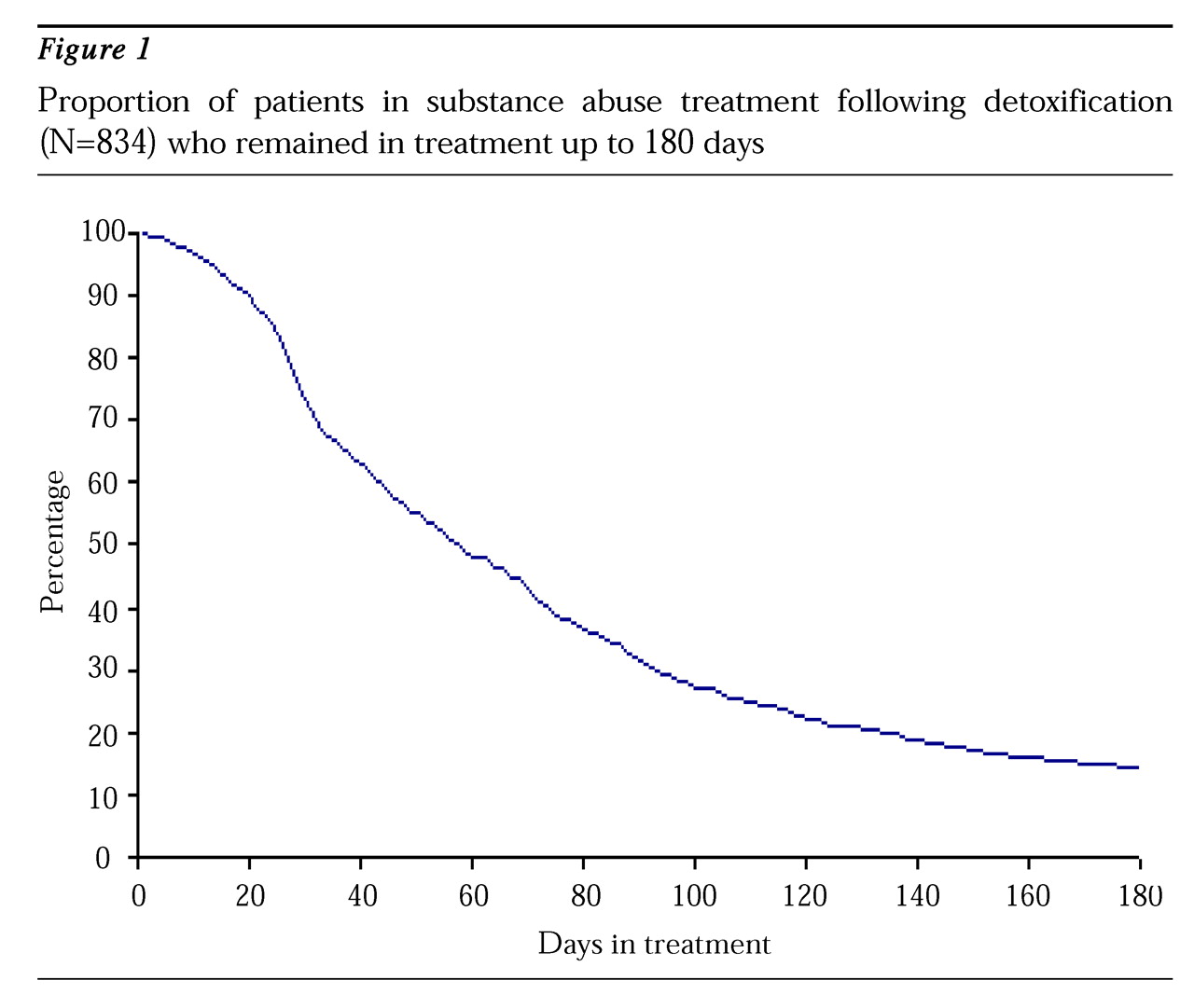
We calculated rates, duration, and intensity of follow-up treatment and used logistic regression to predict whether follow-up treatment was received within 30 days of hospital discharge. We also used survival curve analysis to characterize the duration of follow-up care for 180 days following inpatient discharge. Patients whose coverage ended before that time were treated as censored. Outpatient treatment was considered continuous as long as there were no more than 30 days between consecutive outpatient visits. Intensity of follow-up treatment was calculated as the average number of days between sessions during the first month and from months two to six after discharge. Patients who received only one outpatient session were not included in these calculations so that our estimate of treatment intensity would not be inflated. All sessions occurring within the first 30 days following discharge were incorporated into the calculation of one-month treatment intensity. Only subjects who remained in outpatient treatment for at least 31 days were included in the two- to six-month calculation.
In addition to copayments for follow-up care (in dollars per visit), variables controlled for in the modeling of follow-up rates included age, gender, type of member (distinguishing employees from child and adult dependents), type of diagnosis, year of treatment, and duration of inpatient stay. Robust standard errors (
19,
20) were used to correct for clustering of patients within employers.
Results
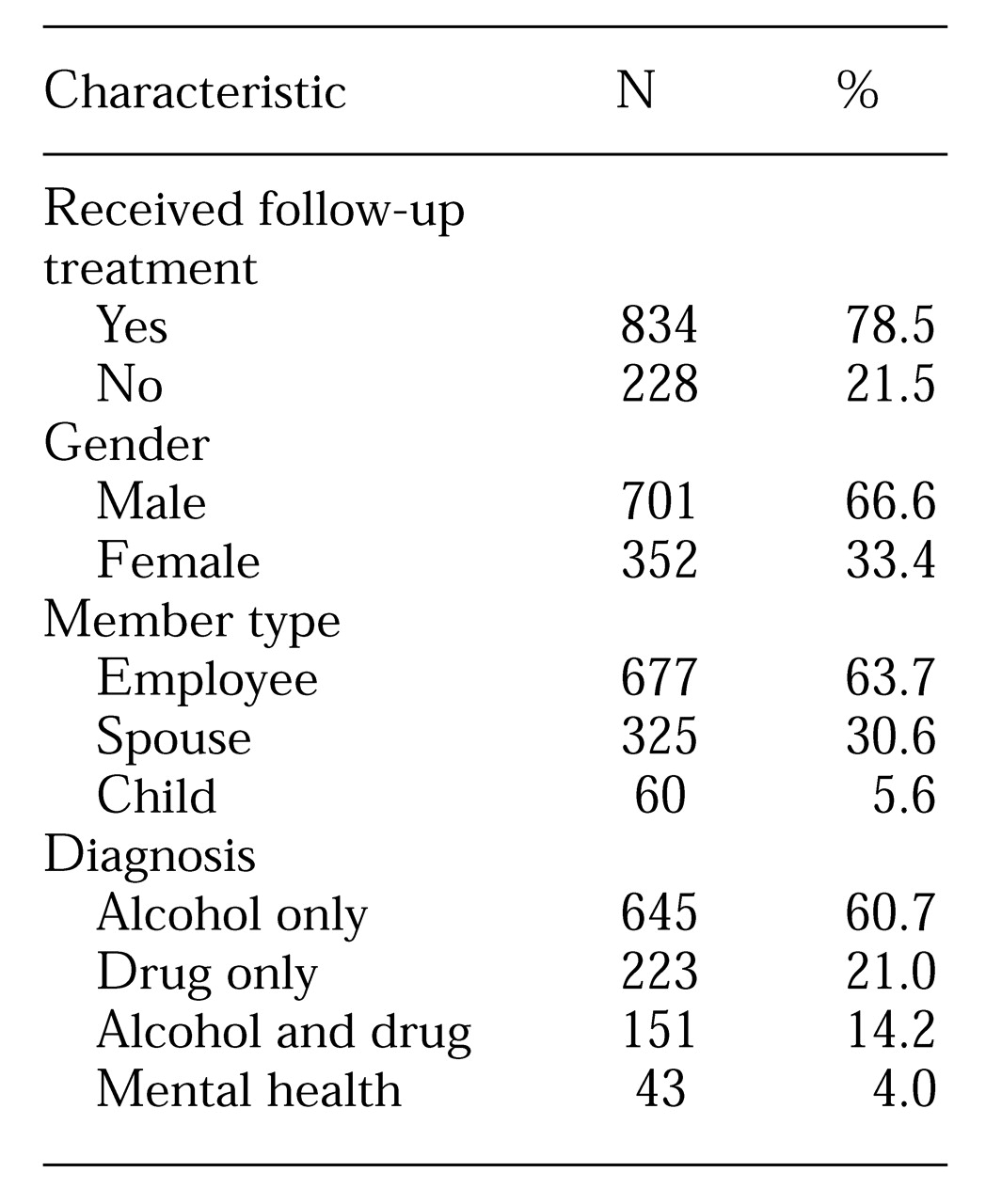
A total of 1,062 patients from 14 employer groups met the inclusion criteria. Their mean±SD age was 40.5± 11.1 years, and their inpatient detoxification hospitalization had been for a mean±SD of 4.2±6.4 days. Their mean±SD outpatient copayment was $12.3±$7.3. Other demographic and clinical characteristics of the sample are shown in
Table 1. The majority of patients, 79 percent, received follow-up treatment within 30 days of hospital discharge.
Among the 834 patients who received follow-up care, 74.3 percent (N=620) were seen within a week, and 92 percent (N=768) received care within two weeks. Outpatient treatment lasted a mean±SD of 75± 112 days; 55.5 percent (N=463) of patients initially received intensive outpatient therapy, which consists of more frequent visits, often for greater duration, than occurs in traditional outpatient therapy. A total of 29.9 percent of patients (N=249) received residential care, and 14.6 percent (N=122) received traditional outpatient therapy. The 561 patients who received more than one outpatient session averaged one session every 4.7±3.6 days in their first month and one session every 11.9±9.9 days in the second through sixth months of outpatient treatment.
The logistic modeling of follow-up care revealed that the likelihood of follow-up decreased significantly with increasing outpatient copayment (OR=.97, p<.05). To get a clearer picture of the copayment effect, we estimated the change in follow-up rates among patients not receiving follow-up with copayments of $30, $20, $10, and $0. Controlling for the effects of other variables, we would predict a 43-percent increase in the number of subjects not receiving follow-up if copayments were held constant at $30, and a 19-percent increase if the copayment were $20. Conversely, a 24-percent decrease could be expected in the number of people not receiving follow-up if no copayment were required, and a 5-percent decrease if the copayment were $10.
Figure 1 presents a survival analysis curve for the duration of care. Half the sample of patients who received follow-up care remained in outpatient treatment after 60 days, and 25 percent were still in formal treatment after three months.
Discussion and conclusions
The results of this study indicate that in one of the largest national behavioral health care carve-out organizations, the proportion of individuals receiving formal substance abuse treatment following inpatient detoxification is relatively high (79 percent). Although we are not aware of any similar studies that would permit a direct comparison, this rate of follow-up care after inpatient detoxification is substantially higher than that seen in populations that are not insured privately (
8,
9). The rate of follow-up in this study is also substantially higher than the national average of follow-up care after hospitalization for depression reported in the National Committee for Quality Assurance Health Plan Employer Data and Information Set (67 percent in 1997) (
21).
Statistics for patients who did receive treatment were also somewhat encouraging. The length of time between discharge and follow-up care was relatively brief, with most initial sessions occurring within one week and more than 90 percent within two weeks. This result is substantially better than that seen in a Veterans Affairs population (40 percent of patients seen within four weeks) (
8). For more than 85 percent of patients, initial treatment after detoxification was at an intermediate level of care, such as residential treatment or intensive outpatient, rather than at a less intensive level of care, such as outpatient treatment. This pattern is consistent with the treatment philosophy of the American Society of Addiction Medicine, whose set of Patient Placement Criteria envisions patients moving along a continuum of care to the least restrictive setting that meets their needs (
22).
The intensity and duration of treatment results are also encouraging, since they indicate that the majority of patients participated in more than a few treatment sessions following their discharge. In the first month after discharge, nonresidential patients who received at least two sessions averaged more than one treatment session a week. Not surprisingly, the frequency declined over time, but even in the second through sixth months of treatment, patients averaged more than one session every other week. Fifty percent of individuals participated in subsequent treatment for at least two months following discharge, and more than a quarter for three months or longer. It thus appears that many patients received more than cursory treatment, although in this sample the treatment often appeared to be less intensive than what many addiction therapists believe is necessary to achieve an optimal outcome (
23,
24).
Despite these generally encouraging findings, room for improvement remains. The fact that more than 20 percent of the subjects did not receive any treatment is cause for concern, given the severity of illness in most patients requiring detoxification, the tremendous personal and societal costs associated with severe drug and alcohol abuse, and the poor outcomes associated with patients who do not receive treatment following detoxification.
Our results suggest that outpatient copayment levels may significantly influence the rate at which discharged detoxification patients enter subsequent treatment. In our sample, after controlling for several other variables likely to affect participation in outpatient treatment, the waiving of all outpatient copayments would have resulted in a predicted decrease of 24 percent in the number of patients not receiving subsequent treatment. This result is particularly striking since the plans included in our study generally had quite low copayments compared with the typical substance abuse copayment of 50 percent (
17). If generalizable, our estimates imply that, by waiving the more typical copayment amount of $30, the rate of nonparticipation in substance abuse treatment among detoxification patients could be cut by almost 50 percent.
The carve-out plans in our sample had relatively generous detoxification and substance abuse benefits, and our findings may not generalize to more restrictive plans or to plans with different management styles. We are also unable to comment on the quality or appropriateness of the treatment provided. Limitations related to the use of claims data include the possibility that some treatment, such as out-of-plan treatment or treatment sessions affected by a deductible, might not be observed. Claims data also do not contain the rich clinical and outcomes data that would permit us to answer many of the other important questions about the treatment of substance use disorders; examples of such data are the primary drug of addiction, rate of relapse, participation in Alcoholics Anonymous or Narcotics Anonymous, and patient satisfaction.
Despite these limitations, this study provides important information about treatment of severe substance use disorders under the most common type of managed behavioral health care. Contrary to the concerns of many, a substantial number of patients appear to have participated in a reasonable number of treatment sessions subsequent to their discharge from inpatient detoxification.
An equally important finding, however, is the substantial effect copayments appear to have on the rate of participation in subsequent treatment. We do not know whether increasing the number of patients who receive treatment through the reduction of copayments would improve outcomes. But evidence is sufficient to conclude that without subsequent treatment, substance abuse patients are no more likely to have a successful outcome than if they had not undergone detoxification.
Federal policy makers at the Office of National Drug Control Policy have acknowledged that we cannot afford not to treat those with severe substance abuse problems (
25). Our study suggests that improved coverage, such as that proposed in the recently introduced substance abuse parity bill, may improve treatment participation following detoxification among this population. Further research is needed to determine whether increased treatment participation is associated with improved outcomes following detoxification, however. By implementing and evaluating programs that waive outpatient copayments for patients completing an inpatient detoxification program, managed behavioral health care organizations can contribute to efforts to improve the treatment of drug and alcohol disorders.
Acknowledgments
The authors thank Robert Brook, M.D., Kenneth Wells, M.D., Joyce McCulloch, M.S., William Goldman, M.D., Elisabeth Merrick, Ph.D., Katherine Watkins, M.D., and Wesley Sowers, M.D., for comments on earlier drafts of this paper. Financial support was provided by grants MH-54147 and MH-54623 from the National Institute of Mental Health, grant DA-11832 from the National Institute on Drug Abuse, and the Robert Wood Johnson UCLA Clinical Scholars Program.