A total of 123 patients (61 percent) were male. The patients' mean±SD age was 36.7±14.2 years (range, 17 to 83 years). A majority of the patients (156, or 78 percent) were without a partner—single, separated, divorced, or widowed. One-hundred and twenty patients (60 percent) had a secondary school education, and 40 (20 percent) had some college or university education. A large proportion—154 patients, or 77 percent—were unemployed; 22 patients (11 percent) were either employed full-time or self-employed. Sixty-six patients (33 percent) had a primary diagnosis of schizophrenia at the index discharge, 56 (28 percent) had a primary diagnosis of mood disorder, 25 (13 percent) of schizoaffective disorder, and 21 (10 percent) of personality disorder.
Reasons for index admission
Many charts listed more than one reason for a patient's 1991 (index) admission. From the clinicians' perspective, the most commonly reported reason was worsening of symptoms, which was listed in 168 (84 percent) of the patients' records. Other reasons were aggression (60 patients, or 30 percent), concerns about risk of suicide (58 patients, or 29 percent), alcohol or drug abuse (44 patients, or 22 percent), psychosocial stress (40 patients, or 20 percent), court-ordered assessment (28 patients, or 14 percent), medication adjustment or destabilization (14 patients, or 7 percent), and medication noncompliance (8 patients, or 4 percent).
The reason for admission that patients cited most frequently was difficulty coping, which appeared in 146 (73 percent) of the patients' records. The next most common reason was persistence of symptoms (128 patients, or 64 percent), which closely paralleled clinicians' reporting of worsening of symptoms. However, although clinicians tended to report the worsening of symptoms as being recent, patients described long-standing problems with intractable symptoms. Other reasons cited were difficulties with relationships (80 patients, or 40 percent), medication noncompliance (60 patients, or 30 percent), drug or alcohol abuse (56 patients, or 28 percent), medical problems (28 patients, or 14 percent), and aggression (22 patients, or 11 percent).
Readmissions after the index discharge
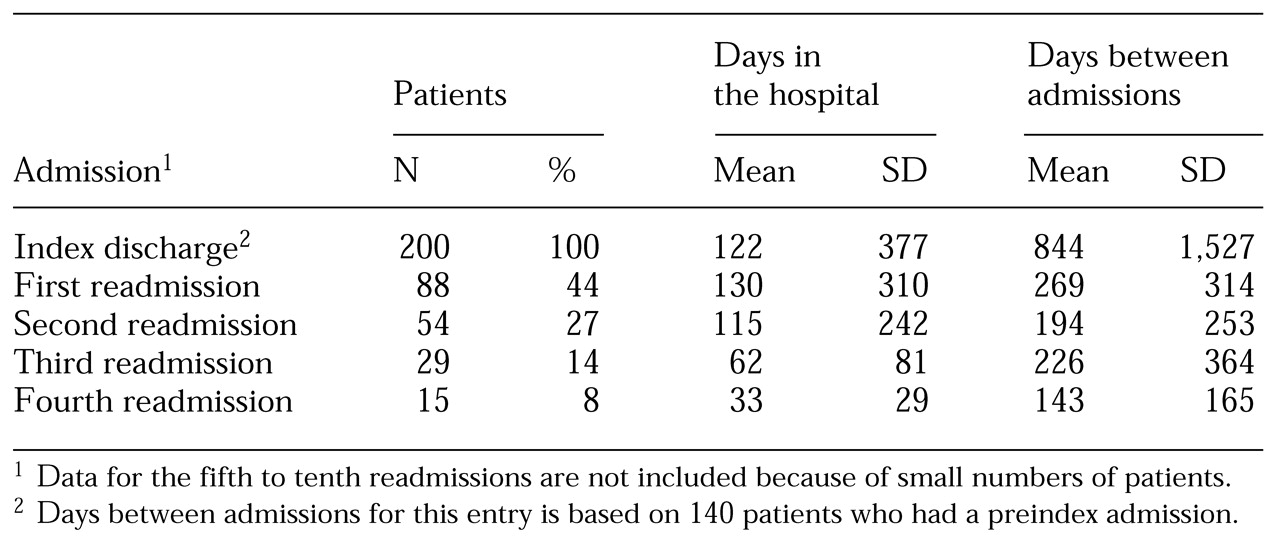
During the three years after the index discharge the mean±SD number of readmissions was 1.04±1.67 (range, zero to ten). Eighty-eight patients (44 percent) were readmitted at least once. The numbers of patients who had second, third, or fourth readmissions became increasingly smaller with the number of readmissions, as shown in
Table 1. The mean length of stay and the mean time between admissions also declined with the number of readmissions. Patients who were readmitted had significantly more admissions to the study hospital before the index admission—their mean±SD number of admissions was 3.3±3.6, compared with 1.3±2.6 for those who were not readmitted. Similarly, the total number of admissions to any psychiatric facility was higher among patients who were readmitted (mean±SD, 7.3±6.4) than among those who were not readmitted (3.2±5.5).
More of the readmitted patients were male (52 patients, or 59 percent) than female (36 patients, or 41 percent). At the index admission, the readmitted patients were slightly younger than those who were not readmitted: the mean±SD ages were 34.2±11.6 years and 38.2±15.7 years, respectively. A significantly larger proportion of patients who were readmitted were divorced. The readmitted patients were significantly more likely to have had a secondary school education, whereas those who were not readmitted had only a primary education or had attended vocational or technical school. In addition, the group of patients who were readmitted contained a significantly higher proportion of individuals who were unemployed or were employed only part-time or who received social assistance.
Although more than one reason for the first readmission was often listed, physicians cited worsening symptoms for 83 (94 percent) of the readmitted patients, followed by aggression (30 patients, or 34 percent) and alcohol or drug abuse (22 patients, or 25 percent). Persistence of symptoms and difficulty coping were each cited by 81 patients (92 percent) as the predominant reasons for readmission, followed by difficulties with relationships (52 patients, or 59 percent) and medication noncompliance (40 patients, or 46 percent).
Diagnosis was significantly associated with readmission. Although some patients had more than one diagnosis, schizophrenia was the primary diagnosis for 36 (41 percent) of the readmitted patients, followed by personality disorder (29 patients, or 33 percent), mood disorder (24 patients, or 27 percent), and schizoaffective disorder (14 patients, or 16 percent).
A history of aggression was also significantly related to readmission. Of the patients who were readmitted, 20 (23 percent) had a history of aggression, compared with 12 (11 percent) of the patients who were not readmitted. A history of behavioral problems was also significantly associated with readmission: 27 (31 percent) of the patients who were readmitted had such problems, compared with 20 (18 percent) of the patients who were not readmitted. The two groups were not significantly different in terms of history of suicide attempts or physical, sexual, or emotional abuse.
When a correlational analysis was used to predict the frequency of readmission, a strong positive correlation was observed between readmission and history of admission (Pearson's r=.54). Weaker inverse correlations of readmission with age at first diagnosis (r=-.20) and of readmission with current age (r=-.17) were also observed. However, when multiple regression analysis was used, the only significant factor to emerge was history of psychiatric hospitalization.