In response to the demonstrated health hazards of tobacco smoking, health care facilities are increasingly implementing policies that ban smoking on their premises. Persons with psychiatric illnesses are about twice as likely to smoke cigarettes as the general population (
1), and the prevalence of smoking among persons with schizophrenia is reported to be three or four times higher than in the general population (
2,
3). Alcohol and drug abuse are also strongly associated with a high rate of smoking, with prevalence estimates ranging from 71 percent to 100 percent (
4,
5,
6). Thus persons with psychiatric or substance use disorders are particularly affected by smoking bans. A concern has been raised that policies that address the risks of smoking in the general population may deter smokers who are mentally ill or substance dependent from obtaining services.
Methods
We conducted a critical review of the literature to assess the strength of the empirical evidence supporting this concern about smoking bans in psychiatric populations. We reviewed the literature on the association between smoking and psychiatric disorders. We then focused on the studies of the impact of smoking bans and attempted to draw policy implications.
We used major health care databases to conduct the search: MEDLINE (1997 to 2001), CINAHL (1990 to 2001), PsycINFO (1990 to 2001), Best Evidence/EBM Reviews (1991 to 2002), Healthstar (1996 to 2001), the Cochrane Database of Systematic Reviews (2001), and EMBASE (1990 to 2002). In addition, Legal Trac (1990 to 2002), Bioethicsline (1973 to 2001), Philosopher's Index (1980 to 2002), and Dissertation Abstracts (1990 to 2002) were searched. Some articles were drawn from the reference lists of previous articles, and unpublished empirical studies were located through a Web search. Major search terms included smoking, smoking cessation, nicotine, health policy, hospital policy, smoke-free policy, psychiatric disorders, mental disorders, and substance use disorders.
Several of the articles on the impact of nonsmoking policies in psychiatric settings and the treatment of smoking in this population were reviews or discussion papers or were based on anecdotal evidence. These papers (a total of 17) were excluded.
Results
Smoking and psychiatric disorders
Investigations of the association between tobacco smoking and psychiatric disorders can be categorized into four areas of interest: smoking as self-medication, nicotine and vulnerability to mental illness, smoking and medication, and the impact of forced nicotine withdrawal.
Smoking as self-medication
Both neurobiological and psychosocial factors reinforce the use of nicotine in psychiatric populations. Nicotine is thought to interact with a number of neurotransmitter systems: serotonin, dopamine, glutamate, acetylcholine, and norepinephrine (
3,
7). There is growing evidence that nicotine functions to normalize two different physiological dysfunctions in schizophrenia, auditory sensory gating (
8,
9) and abnormal smooth-pursuit eye movements (
7). In addition, the dopaminergic and glutaminic alterations created by nicotine are thought to improve negative symptoms (
10). The link between smoking and depression has been attributed to the use of nicotine for alleviating dysphoric moods (
11,
12). Smokers who have a history of depression are more vulnerable to developing depression during nicotine withdrawal, and the withdrawal syndrome is more severe among these persons (
7,
13).
A strong correlation between nicotine use and other substance abuse also exists. Among all persons with a psychiatric diagnosis, those who abuse alcohol have the highest rates of smoking, in terms of having ever smoked (
13). In a study of nicotine dependence and abstinence in schizophrenia, Ziedonis and colleagues (
10) found that smokers had significantly higher rates of alcohol and drug abuse than nonsmokers and that heavy smokers had the highest rates of both alcohol and drug use disorders.
The subjective calming effect of nicotine is also thought to be particularly reinforcing for persons with psychiatric illness (
14). It has been suggested that smoking reduces social inhibition and isolation and that it may provide an outlet for the expression of dependency needs among persons with schizophrenia (
10,
14). Van Dongen (
14) found that for many people with persistent mental illness, smoking is a major part of their daily routine and is considered to provide some structure to a day with few activities. Moreover, smoking has long been considered an integral part of the psychiatric culture, and there exists an ingrained belief that persons with mental illness are not able or willing to quit smoking. As a result, this population has been largely excluded from the greater societal movement toward minimizing smoking, and health professionals who work with persons who have mental illness have taken a passive stance in talking to their patients about quitting smoking.
Nicotine and vulnerability to mental illness
A few studies suggest that nicotine may increase one's vulnerability to mental illness. Ziedonis and colleagues (
10) found that the onset of schizophrenia is significantly earlier among those who smoke. Another study reported that persons who smoke daily have an elevated risk of first-time occurrence of panic attack (
15). Smoking has also been found to increase the risk of certain anxiety disorders during late adolescence and early adulthood (
16). Other evidence suggests that smoking is associated with an elevated risk of depression (
1,
17,
18). Finally, there is evidence that smokers are more vulnerable to other forms of substance abuse, with nicotine acting as a "gateway" drug (
4,
19).
Smoking and medication
Smoking cigarettes can reduce the blood concentrations of a number of psychiatric medications (
3,
20,
21,
22). Plasma neuroleptic concentrations can be up to 50 percent lower among heavy smokers, because smoking induces higher enzymatic activity, which accelerates the metabolism of these medications (
3,
21,
22). Thus patients who smoke tend to receive significantly higher doses of neuroleptics (
10,
23,
24,
25). There is no evidence that specifically links the metabolism of neuroleptic medications to nicotine; rather, it is believed that the effect is produced by the tar in cigarettes (
10). It is interesting that patients who are taking conventional antipsychotics are likely to smoke more, whereas patients who are taking atypical antipsychotics, such as clozapine, tend to smoke less (
3).
Some studies have found that patients with schizophrenia who smoke have fewer parkinsonian symptoms than those who do not smoke (
23,
26), which suggests that smoking has a protective effect on dopamine systems (
25). Other research has shown higher rates of tardive dyskinesia among patients with schizophrenia who smoke (
1,
27). However, the findings related to both parkinsonism and tardive dyskinesia are mixed and inconclusive. In a study by Linnoila and associates (
20), smoking was associated with low plasma amitriptyline and nortriptyline concentrations, although there have been contradictory findings.
Impact of forced nicotine withdrawal
Forced nicotine withdrawal is associated with significant risks for psychiatric patients. Nicotine withdrawal produces physiological, behavioral, and subjective changes that present similarly to positive and negative psychiatric symptoms, side effects of medications, and alcohol or drug withdrawal (
28). Thus there is a risk of misinterpretation and exacerbation of symptoms when psychiatric patients cease smoking (
25,
29,
30). People with schizophrenia or a history of depression or anxiety report more severe withdrawal symptoms than do persons without these disorders (
31). Smoking cessation can also precipitate a relapse of depression among smokers who have a history of depression and can increase anxiety for some patients (
28).
Because smoking increases the metabolism of neuroleptic medications, forced smoking cessation may alter the blood concentrations of various psychiatric medications and may result in dangerously high drug concentrations and problematic side effects (
32).
Empirical studies of smoking ban policies
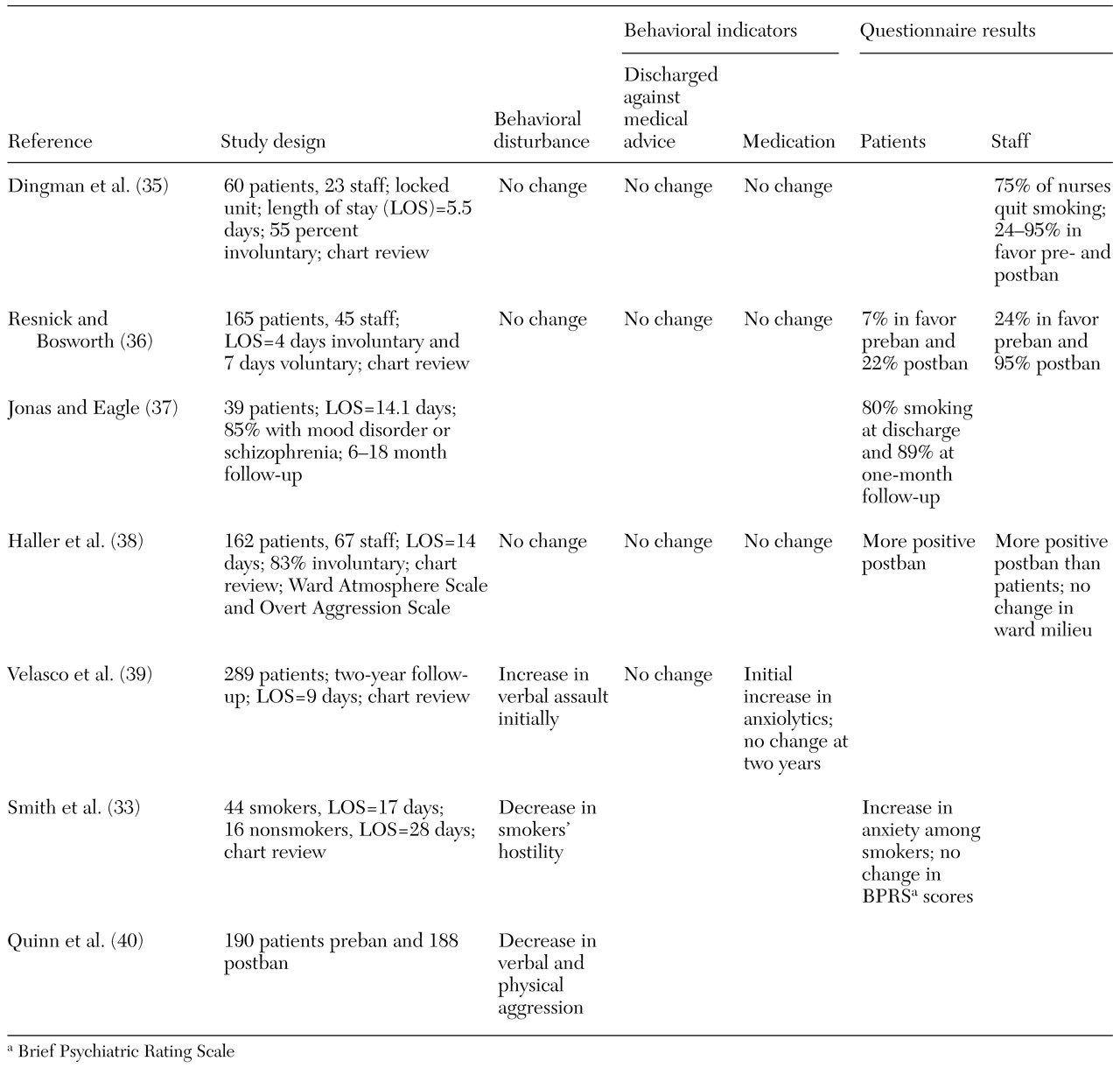
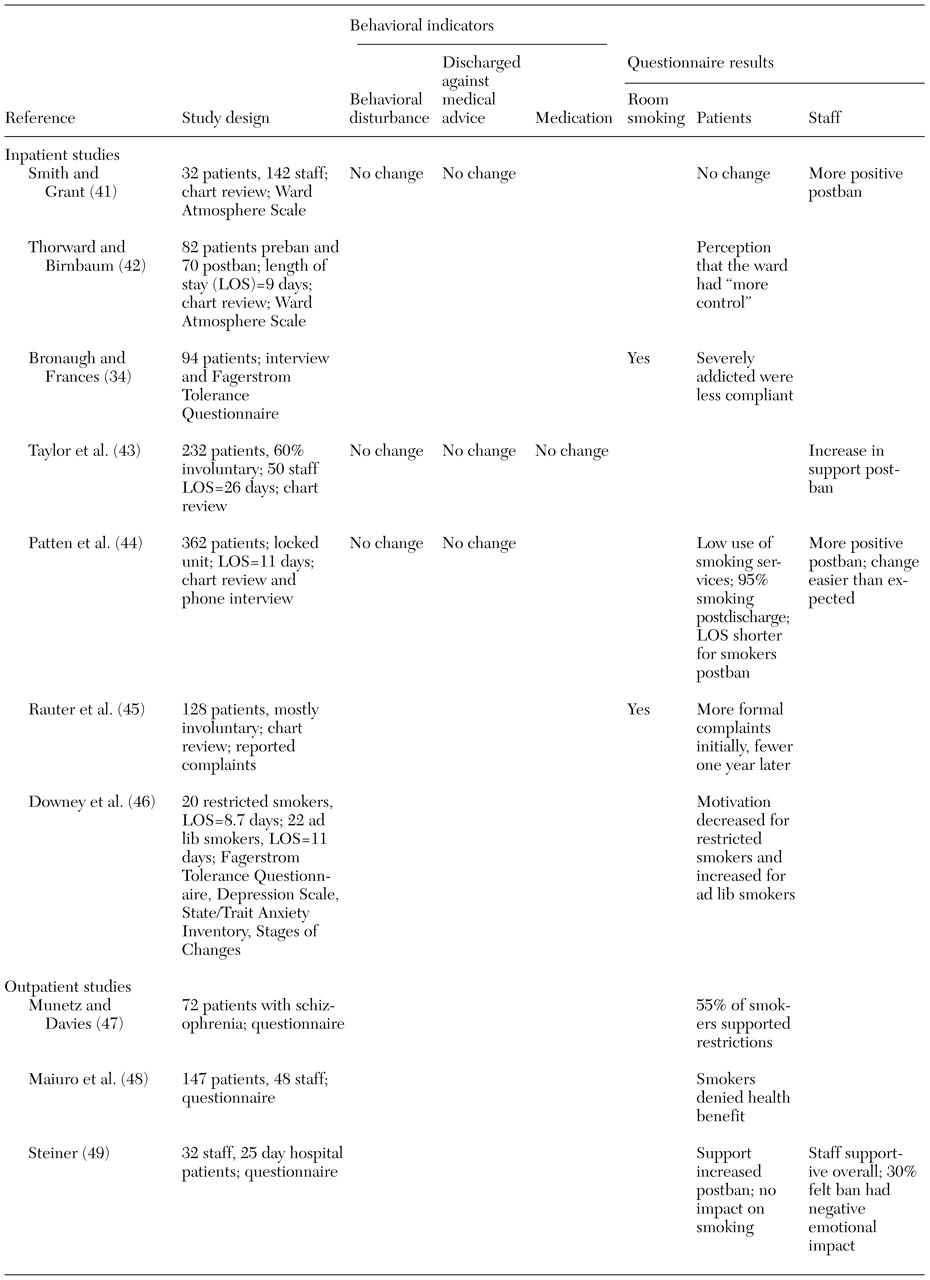
Policies that ban smoking in inpatient psychiatric or addiction settings are either "total," which means that no smoking is allowed within the facility or on passes, or "partial," which means that smoking is allowed in the facility or on passes. Our literature search yielded seven investigations of the impact of total bans in inpatient psychiatric settings, listed in
Table 1, and seven on the impact of partial bans, which are listed in
Table 2 (
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49). In addition, three investigations examined the impact of bans in outpatient waiting rooms or day hospital programs; these studies are also listed in
Table 2. We retrieved two studies of total bans and three of partial bans in addiction settings. The impact was assessed either through chart reviews or through structured questionnaires, and the behavioral indicators included the use of restraints or seclusion, the occurrence of assault or injury, the number of calls to security, discharges against medical advice or elopements, medication changes, and records of illicit smoking in patients' rooms. The Ward Atmosphere Scale and the Overt Aggression Scale were the most common instruments used. However, published studies have not been consistent in the use of behavioral indicators, and some studies collected no objective data. Thus the use of meta-analytic methods was precluded by the lack of uniform dependent variables across studies. The number of studies that used similar outcome measures was too small for their effect sizes to be reliably estimated.
In contrast with studies in psychiatric settings, the five studies on the impact of smoking bans in addiction settings focused mostly on the smokers' interest in quitting before and after the ban rather than on behavioral disorders and management issues arising from the policy. Joseph and colleagues (
50), in two consecutive studies of total bans in residential programs, found an increase in the proportion of smokers who were interested in quitting after the ban (from 24 percent to 61 percent) and in the proportion of those who actually abstained from smoking (41 percent after the ban compared with 9 percent before the ban). No adverse effect on drug or alcohol treatment was noted (
51).
Regarding partial bans, a survey of 19 program directors reported fewer complaints than anticipated, but nicotine treatment was not fully integrated into most programs (
52). In another study, staff support for an emphasis on smoking cessation declined after the policy was implemented (
53). Kempf and Stanley (
54) compared two adolescent residential units, one with a total ban on smoking and one with a partial ban, and found no difference between the two units in rates of in initial rejection of the program or in dropout rates, with heavy smokers more likely to drop out from either unit.
The preponderance of evidence from the reviewed literature suggests that policies that ban smoking have no major long-standing untoward effects in terms of the behavioral indicators of unrest or noncompliance. One study found no association between scores on the Fagerstrom Tolerance Questionnaire (FTQ) or the Nicotine Withdrawal Checklist (NWC) and subjective anxiety (
33), whereas another study found a negative association between FTQ scores and compliance with a nonsmoking policy (
34). Indeed, the amount of support for the policies among patients and staff may actually be higher after the ban. However, these self-reports contrast with the results of three studies that showed that smoking resumed immediately after discharge or that motivation to quit was lower among patients whose smoking was restricted.
Discussion and conclusions
We found a discrepancy between studies that showed a significant interaction between smoking and psychiatric disorders and the fact that only four of the 17 studies reported behavioral consequences of smoking bans. Explanations may be found in the relatively crude indicators of behavioral unrest or noncompliance that have been used to study the impact of nonsmoking policies. Forced nicotine withdrawal may not always translate into aggressive behavior, need for restraint, or other forms of noncompliance. Also, administrative bias in favor of a nonsmoking policy may mean that fewer untoward effects are reported.
Although policies that ban smoking satisfy a public health agenda during residential treatment, they appear to have little or no effect on the goal of smoking cessation. Despite self-reported increases in support for smoking bans after implementation of the policy, resumption of smoking after discharge is highly prevalent and immediate. Motivation for quitting smoking may even decline if a restrictive smoking policy is insensitive to the progression of the stages of change that are required before a person can quit smoking.
A growing body of literature shows that, in general, smoking cessation strategies result in outcomes among psychiatric patients that are not very different from those in the general population (
55,
56). Relatively brief interventions can increase the number of persons who quit smoking. Minimal training that can encourage health professionals to be sensitive and to be prepared to address patients' concerns about quitting is a cost-effective investment. Smoking cessation strategies, which can range from supportive counseling to pharmacotherapy, should be an inherent component of nonsmoking policies.
Total bans and outdoor bans raise ethical issues in terms of balancing the rights of nonsmokers against those of smokers. Arguments center around the extent of the threat presented by outdoor, second-hand smoke. Although chronic and cumulative exposure to indoor smoking—for example, living with a smoker or working in a smoking environment—creates a definite hazard, the risk associated with fleeting outdoor exposure is much more controversial and does not justify a lack of flexibility. The support for outdoor bans may be based more on the demand for an aesthetically pleasing environment for nonsmokers and the need for health care facilities to model healthier lifestyle practices for their clients (
57,
58).
This study was limited in that a meta-analysis could not be conducted. Our conclusions about the impact of smoking bans on patients' behavior are largely qualitative given that a majority of studies did not show large untoward reactions. The lack of uniform measures of outcome is not surprising given that most studies used retrospective designs. More studies with prospective designs are needed to verify our conclusions.
As nonsmoking policies evolve with changes in social awareness and acceptance of tobacco smoking, flexibility is recommended in order to protect nonsmokers while promoting a therapeutic agenda for smokers. The significant interactive effects between smoking and psychiatric disorders pose particular challenges to smoking cessation that must be addressed.