Antipsychotic drugs are an important component of the psychopharmacologic armamentarium. They are effective in reducing psychotic symptoms and controlling other manifestations of psychiatric illness. Use of antipsychotics increased during the two decades after their introduction in the early 1950s and then declined from the mid-1970s through the 1980s (
1,
2). Using data from a national audit, Wysowski and Baum (
1) found that the number of prescriptions for antipsychotic drugs dropped from 21 million in 1976 to 19 million in 1985. Another study, using data from the National Ambulatory Medical Care Survey (NAMCS), showed that the number of office visits during which antipsychotic drugs were prescribed dropped sharply between 1980 and 1989, from 6.01 million to 3.65 million (
2). These declines occurred amid a growing awareness of side effects (
3), concern about overuse (
1,
4,
5,
6,
7,
8,
9), and the implementation of federal regulations governing the use of these drugs in nursing homes (
10).
Use of antipsychotic medications has not been extensively studied in the 1990s—a period notable for the introduction of atypical antipsychotics and extensive changes to the organization, financing, and delivery of health care. Pincus and colleagues (
11) examined NAMCS data and reported that the number of office visits during which antipsychotic drugs were prescribed did not change significantly from 1985 to 1994, a period preceding much of the marked growth in sales of atypical antipsychotic drugs (
12).
In this study, we examined trends in overall prescription rates for antipsychotic drugs between 1989 and 1997 using data from the NAMCS. We also examined antipsychotic drug prescribing practices in demographic, organizational, and clinical subgroups in pooled samples, comparing the periods 1989-1991 and 1995-1997. Concerns have been expressed about the potential overuse of antipsychotic drugs among children (
13,
14), but studies of this population have been limited (
8,
15). There has also been concern about greater use of antipsychotics among racial and ethnic minority groups than among nonminority groups (
16,
17).
We compared the prescription of these drugs under prepaid care and nonprepaid care. Johnson and McFarland (
9) found that the rate of use of antipsychotics among enrollees in a large, commercial prepaid health plan in 1986-1987 was lower than national per capita estimates. It is not known whether similar differences exist in other plans or whether they have persisted into the 1990s, a period of expansion of prepaid care. We also examined per capita rates of prescription for evidence of geographic variation. Geographic variations in clinical practices have been examined as indicators of treatment access and appropriateness (
18,
19,
20,
21).
We examined trends in the prescription of the atypical antipsychotics clozapine, which was introduced in the U.S. in 1990, risperidone, introduced in 1994, olanzapine, introduced in 1996, and quetiapine, introduced in 1997. Controlled trials have shown that atypical agents are less likely than conventional antipsychotics to cause extrapyramidal symptoms (
22,
23,
24). In addition, clozapine has demonstrated superiority over conventional agents in reducing symptoms of schizophrenia (
24). These benefits, in conjunction with the higher costs of atypical agents—as much as 15 times the cost of conventional antipsychotic drugs (
22)—make trends in the adoption of atypical antipsychotics of interest to clinicians, payers, and policy makers. Longitudinal national trends have not been reported, but studies in individual clinical settings have described rapid adoption of risperidone after its introduction (
25,
26,
27). Because of cost concerns, some payers and plans have limited the use of atypical antipsychotics (
28,
29). We examine whether the use of atypicals under prepaid care is lower than under nonprepaid care.
Because use of antipsychotic drugs can lead to adverse cognitive and motor effects, patients must be periodically evaluated to monitor for adverse effects, to reevaluate the need for medication, or to adjust the medication to achieve the lowest effective dosage (
30,
31). We compared follow-up practices of psychiatrists and nonpsychiatrist physicians. We hypothesized that specialists would monitor patients more closely.
Methods
Source of data
The source of data was the NAMCS (
32,
33), conducted annually by the National Center for Health Statistics. The NAMCS samples a nationally representative group of visits to active physicians in nonfederal office-based clinical practice. The survey excluded hospital outpatient departments and emergency departments but included freestanding outpatient clinics.
The sample was selected through a three-stage sampling design. First, a set of primary sampling units was selected—a county, a group of adjacent counties, or a standard metropolitan statistical area. Within each unit, a probability sample of practicing physicians was drawn. Physicians were selected from the master files of the American Medical Association and the American Osteopathic Association of all U.S. physicians, regardless of their membership status. Finally, a random sample was drawn from the visits to these physicians during a one-week period. Altogether 115,648 visits were sampled between 1989 and 1991, and 91,395 visits were sampled between 1995 and 1997. Response rates ranged from 69 percent in 1997 to 74 percent in 1989.
Physicians were asked to complete a one-page patient record form for each selected patient visit. The patient record form included information about the patient (demographic characteristics, diagnosis, and type of payment), the clinician (specialty and geographic location), and the visit (type of treatment provided and type of follow-up planned). The question on follow-up was not included in the 1997 survey, so that year was excluded from the analysis of disposition practices. To examine regional variations in use of antipsychotics, visits to offices in urban locations were identified on the basis of whether the clinician was practicing within one of the 322 U.S. Census standard metropolitan statistical areas.
Definitions
We followed methods used in previous studies that examined NAMCS data to determine prescription rates for antipsychotic drugs (
2,
11,
34). An antipsychotic drug visit was defined as a patient visit in which an antipsychotic medication was administered, prescribed, or continued. Antipsychotic drugs were classified according to the 1997
Physicians' Desk Reference (
35). In the unweighted sample, there were 728 antipsychotic drug visits in the period 1989-1991 and 901 in the period 1995-1997. We classified clozapine, risperidone, olanzapine, and quetiapine as atypical antipsychotic drugs.
Physicians were asked to record up to three diagnoses associated with the current visit or otherwise significant. Antipsychotic drug visits were categorized according to the patient's diagnosis by use of coding from the International Classification of Disease, Ninth Revision, Clinical Modification. Because more than one diagnosis may have been recorded for a visit, we categorized patients according to a hierarchical ranking of diagnoses. Patients with a diagnosis of schizophrenia and other psychotic disorders (codes 293.81, 293.82, 295, 297, and 298) were assigned to that category. The other categories, in descending order, were affective disorders (293.83, 296, 300.4, 301.13, and 311), other psychiatric disorders (290, 293 [excluding 293.81 to 293.83], 294, 780.9, 291, 292, 299, 300 [excluding 300.4], and 301 to 319), and nonpsychiatric disorders (codes below 290 and above 319).
Statistical analysis
For analysis of change in overall prescription rates for antipsychotics before and after the introduction of the atypical agents, we compared the results from the 1989 and the 1997 surveys. Analyses of demographic, organizational, and clinical subgroups, for which greater statistical power was required, were based on surveys conducted in the periods 1989-1991 and 1995-1997. NAMCS was designed to allow data from consecutive years to be pooled to establish a larger sample from which to derive annual estimates (
33).
Sampling weights, developed by the National Center for Health Statistics for use with NAMCS data, were provided to allow extrapolation of the findings to produce national estimates. The weights adjust for the sampling design and account for nonresponse and for the representation of physician specialty. In addition, U.S. Census population estimates are used to inflate the weights to facilitate calculation of national estimates. An additional statistical adjustment was used to prepare the data for statistical testing. This adjustment involves reducing the effective sample size of the survey to simulate sampling from a simple random sample. The weights were multiplied by an adjustment factor calculated by dividing the sum of poststratification weights by the sum of the squared poststratification weights (
36). This procedure yields conservative estimates that tend to overcompensate for stratification artifacts (
37). All analyses were conducted with the adjusted weights in SAS Version 6.12 (
38).
Standard errors and corresponding confidence intervals of proportions were calculated with the usual formula for the normal approximation of the binomial distribution using the effective sample size. An annotated copy of the SAS programs used to calculate the estimates is available from the authors. We chose a conservative cutoff for type I error (corresponding to 99 percent confidence intervals [CIs]) to account for multiple comparisons. Differences between estimates were considered statistically insignificant if their confidence intervals did not overlap. The National Center for Health Statistics considers an estimate to be unreliable if it has either a relative standard error of more than 30 percent or a sample of fewer than 30 visits.
Results
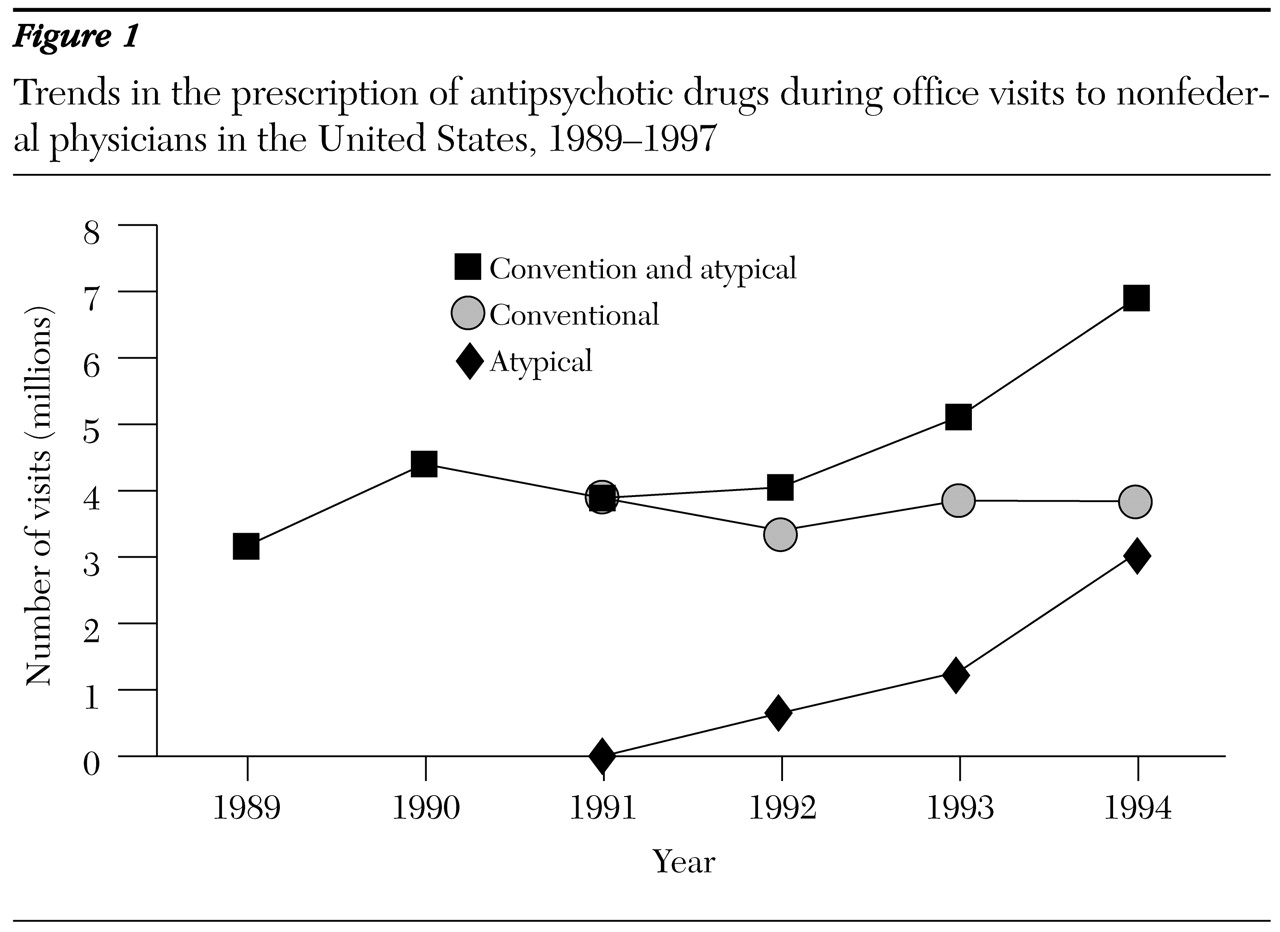
Prescription of antipsychotic drugs by physicians in nonfederal office-based practice in the United States increased significantly from an estimated 3.2 million visits in 1989 (CI=2.1 to 4.2) to 6.9 million visits in 1997 (CI=5.0 to 8.8, p<.01). The proportion of antipsychotic visits among all medical visits increased from .46 percent of all visits (CI=.35 to .57) to .88 percent (CI=.69 to 1.07, p<.01). In 1997 prescriptions for atypical antipsychotics constituted 44 percent of prescriptions for all antipsychotic drugs.
Two atypical agents were the most widely prescribed antipsychotic drugs in 1997. Risperidone was prescribed during 1.65 million visits, or 22.8 percent of all antipsychotic drug visits. Olanzapine was prescribed during 1.23 million visits, or 17.1 percent of such visits. Clozapine was prescribed during .1 million visits, or 1.4 percent of such visits. Trends in the use of typical and atypical antipsychotic drugs are depicted in
Figure 1.
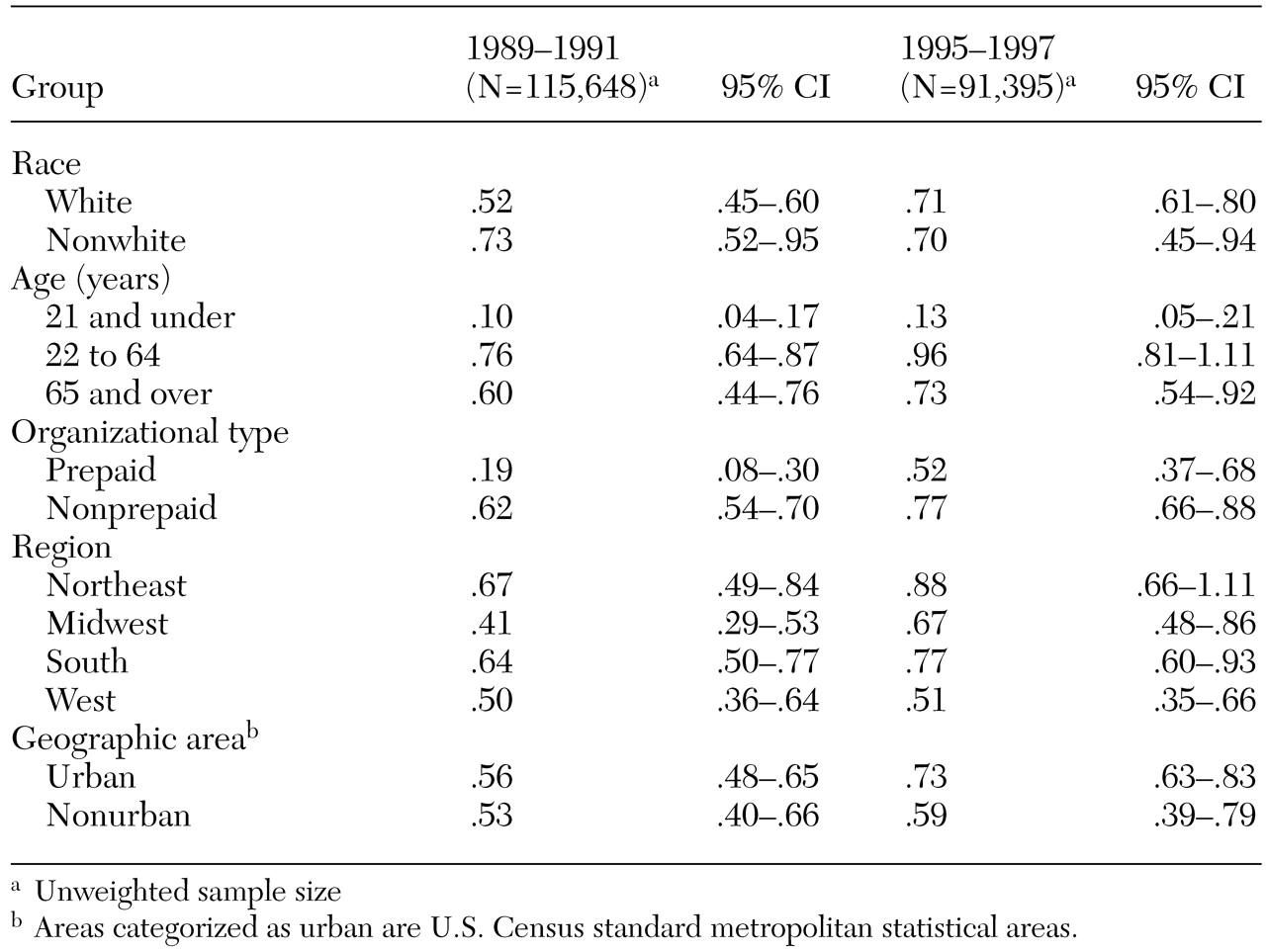
Table 1 shows the proportions of office visits during which antipsychotic drugs were prescribed for various groups. For persons aged 21 and under, the proportion in the period 1995-1997 was .13 percent, significantly lower than the proportions during the same period for adults aged 22 to 64—.96 percent (p<.01)—and adults aged 65 and over—.73 percent (p<.01). The proportion of antipsychotic drug visits for those aged 21 and under did not significantly change between the two periods examined, 1989-1991 and 1995-1997.
In the period 1989-1991, the proportion of antipsychotic drug visits was .52 percent for whites and .73 percent for nonwhites. The difference was not significant. This gap narrowed further in the period 1995-1997, when the rate of use among whites increased significantly to .71 percent (p<.01) and the rate among nonwhites remained essentially unchanged at .70 percent.
Between the two periods, the rate of prescription of antipsychotic drugs under prepaid care increased significantly, from .19 percent to .52 percent (p<.01), closing the gap with the 1989-1991 rate for nonprepaid care. Prescription rates did not differ significantly between urban and nonurban areas or by geographic region in either period.
As shown in
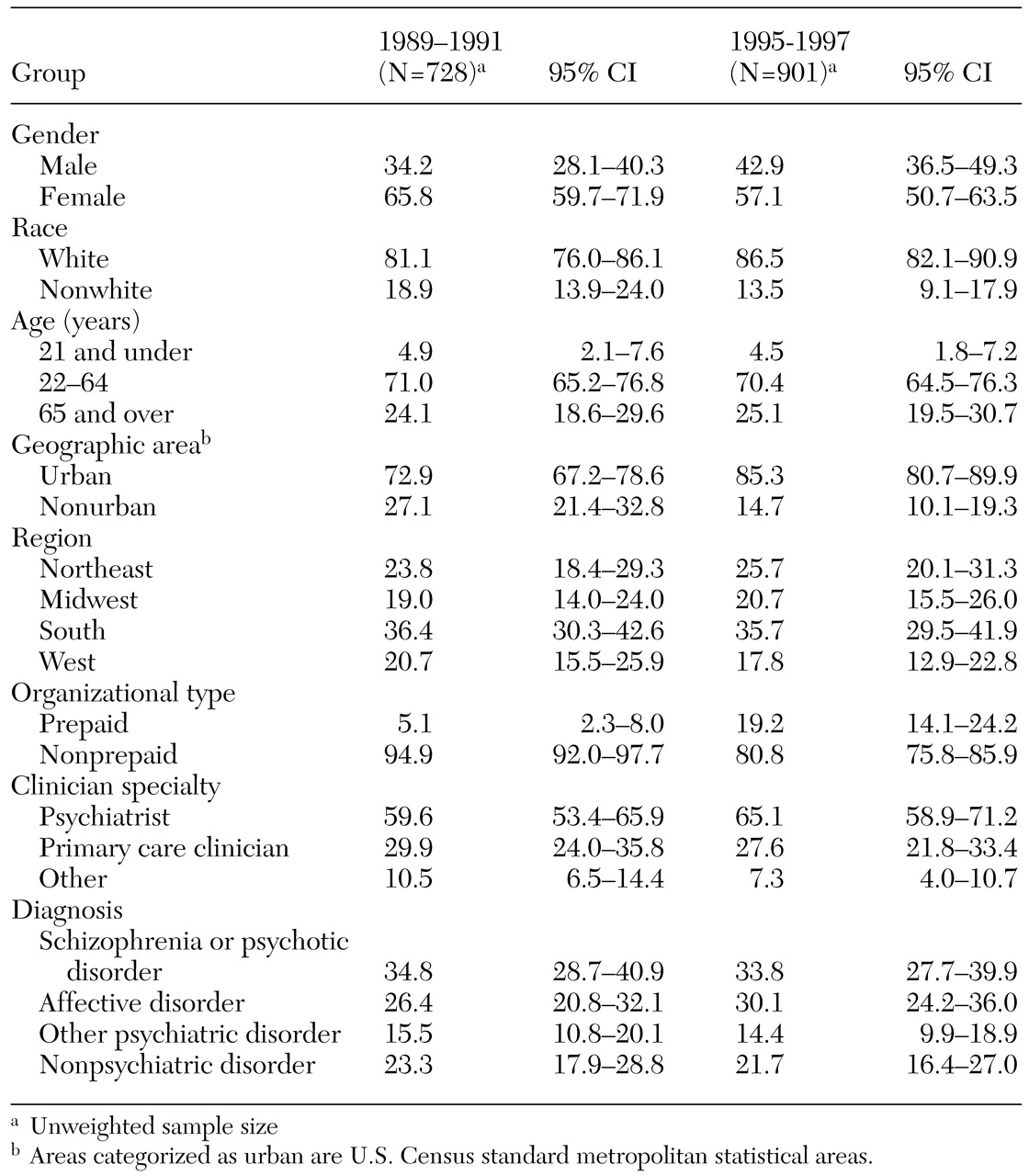
Table 2, the proportion of antipsychotic drug visits for 1995-1997 was 4.5 percent for persons aged 21 and under, significantly less than the proportions for persons aged 22 to 64 (70.4 percent, p<.01) and those aged 65 and over (25.1 percent, p<.01). The proportion of antipsychotic drug visits for women (57.1 percent) was higher than that for men (42.9 percent, p<.01). A greater proportion of such visits occurred in the South (35.7 percent) than in the Midwest (20.7 percent, p<.01) or the West (17.8 percent, p<.01). The difference between the South and the Northeast was not statistically significant.
Between the two periods, the proportion of antipsychotic drug visits in urban areas increased significantly, from 72.9 percent to 85.3 percent (p<.01), as did the proportion of use under prepaid health plans, from 5.1 percent to 19.2 percent (p<.01). There was no significant change between the two periods in the proportion of such visits for conditions other than schizophrenia and other psychotic disorders.
In the period 1995-1997, psychiatrists were significantly more likely to prescribe an atypical antipsychotic drug than other physicians—37.1 percent of antipsychotic drug visits to psychiatrists compared with 14.2 percent to physicians (p<.01). There was no significant difference between prepaid and nonprepaid groups in the proportion of antipsychotic drug visits during which an atypical agent was prescribed.
In the period 1995-1996, disposition plans for 87.8 percent of antipsychotic drug visits included a scheduled follow-up appointment. Psychiatrists were significantly more likely than other physicians to schedule a follow-up visit after a visit during which they prescribed an antipsychotic drug—96.6 percent compared with 73 percent (p<.01).
Discussion
The prescription of antipsychotic drugs in nonfederal, office-based physician practice in the United States increased sharply and significantly between 1989 and 1997, after a sustained decline from the mid-1970s though the 1980s (
1,
2). Visits to physicians during which an antipsychotic drug was prescribed increased both in absolute terms and as a proportion of all medical visits.
The increase in the prescription rate for antipsychotic drugs between 1989 and 1997 was accounted for entirely by the growth in the use of atypical antipsychotics, which were prescribed during more than three million visits to physicians in 1997. Within one year after the introduction of risperidone and three years after the introduction of olanzapine, they became the most widely prescribed antipsychotic drugs. Use of conventional antipsychotics as a group did not change between 1989 and 1997.
For visits during which an antipsychotic was prescribed, we found that psychiatrists were more likely than other physicians to prescribe an atypical antipsychotic. This finding may be related to the role of specialists as early adopters of new medications, to the effects of targeted promotion, or to differences in the patient populations treated. Even though it has been reported that some individual health plans and managed care organizations have restricted the use of atypical agents, we did not find that the prescription of atypical agents during antipsychotic drug visits under prepaid care was significantly less likely to occur than under nonprepaid care. Fewer than 2 percent of antipsychotic drug visits in 1997 involved prescription of atypical antipsychotics, which is consistent with other reports of low rates of use for these agents (
39). The low rates have been attributed to the risk of agranulocytosis, high costs, and the inconvenience associated with the need to closely monitor patients.
Our findings do not support concerns that the prescription rate for antipsychotic drugs is higher among racial minority groups than among whites. Use of antipsychotics among children and adolescents was much lower than use among adults and did not increase during the period studied. We found no evidence to suggest that diagnostic indications for antipsychotic drug use had changed over the period studied; the proportion of use for conditions other than schizophrenia and psychotic disorders remained constant. Nor was there evidence of geographic variation in prescription rates for antipsychotics among large U.S. Census regions. The results of Safer's study (
40) of prescribing practices at five Maryland community mental health centers suggested that use may vary among smaller geographic or service units. Further study using population-based samples may reveal variation and allow its determinants to be identified.
Between the periods 1989-1991 and 1995-1997, the rate of use of antipsychotics under prepaid care increased to the rate seen under nonprepaid care. This finding is consistent with the expansion of prepaid care to include individuals with severe and persistent mental illness. Many states have enrolled psychiatrically disabled Medicaid beneficiaries into prepaid managed care programs (
41).
Nearly 90 percent of antipsychotic drug visits had a disposition plan that included a scheduled follow-up visit; this finding is consistent with recommendations that patients taking these medications be monitored for side effects (
30,
31). Psychiatrists were significantly more likely to adhere to this practice than nonpsychiatrist physicians. Further analysis with more detailed data is needed to examine whether these differences are attributable to clinician practices or differences in patient presentations and needs. If the former, then further clinician education may be needed in the use of these drugs.
The NAMCS database does not include information from physicians who practice outside of nonfederal, office-based ambulatory practice settings. Thus it excludes treatment settings in which many individuals with chronic psychotic illnesses receive care, such as correctional facilities, Department of Veterans Affairs outpatient clinics, and hospital outpatient departments. The trends reported here may or may not reflect changes in physician practice in these settings. Nonetheless, information from the NAMCS survey is of value because it allows for comparisons with previously reported NAMCS data on antipsychotic use (
2) and because there are no other national surveys of recent trends in antipsychotic prescribing patterns. Further research should investigate whether the trends reported here are also seen in practice settings that we were unable to examine.
In addition, the NAMCS surveys office visits and not patients, and thus the data may overrepresent frequent users of medical services. Comparisons of antipsychotic drug use between sectors and groups may be influenced by case-mix differences that are not detectable in the available data. Some antipsychotic prescribing is done by nurse practitioners, who are not included in the NAMCS. Diagnoses in the survey were based on clinicians' judgment rather than independent or structured assessment, which may limit their validity and reliability. On the other hand, diagnostic information was not subject to reimbursement-based coding bias, which can affect the validity and reliability of many administrative data sets (
42). Despite its limitations, NAMCS is the most comprehensive national survey of office-based physician practice.
Conclusions
The prescription of antipsychotic drugs in office-based practice is rising, driven principally by the use of the newer, atypical agents. Within a few years after their introduction, olanzapine and risperidone became the most widely prescribed antipsychotic drugs in office-based practice. Psychiatrists were more likely than other physicians to prescribe an atypical agent and more likely to schedule follow-up visits after prescribing an antipsychotic.
The rise in antipsychotic drug use renews attention to whether these drugs are used principally for a narrow range of diagnostic indications or more broadly. We found no evidence of a broadening of diagnostic indications for use over time. As more becomes known about the long-term risks and benefits of atypical agents, detailed study of prescribing practices can shed light on access to atypical antipsychotics and their appropriate use.
Acknowledgments
This research was supported by the van Ameringen Foundation and by grant K08-MH-001477 to Dr. Hermann and grant R29-MH-53698 to Dr. Ettner from the National Institute of Mental Health.