A growing body of literature suggests that individuals who have experienced trauma or who exhibit symptoms of posttraumatic stress disorder (PTSD) may have an elevated risk of medical illness. People who have experienced trauma are more likely to seek treatment from primary care or specialist medical practitioners than from mental health clinicians (
1,
2).
However, most of the research on medical complaints co-occurring with PTSD has not examined a primary care population. Typically such research has focused on veteran populations and has found that veterans with PTSD report more physical symptoms or perceptions of worse health than veterans of the same war who do not have PTSD (
3,
4,
5,
6,
7,
8,
9). Similar results have been found in a few nonveteran samples. For example, women who experienced a sexual assault reported more somatic complaints than did matched controls (
10,
11). Also, persons who had been hostages in a terrorist hijacking reported higher rates of a number of medical problems than their family members (
12).
In these studies the authors did not report on the psychiatric status of the participants who did not have PTSD or a history of trauma or on coexisting psychiatric disorders in the group with PTSD or a trauma history. It is possible that the higher reported rates of medical problems among participants with PTSD or a trauma history are in fact due to greater overall psychiatric difficulties in these groups.
The study by Andreski and associates (
13)—unlike the other studies reviewed here, which compared individuals who had PTSD or a history of trauma with control subjects—also compared persons who had PTSD or a history of trauma with persons who had other psychiatric disorders. In a study of 1,007 members of a health maintenance organization, they organized participants into three groups: those with PTSD; those with psychiatric disorders other than PTSD, including generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, phobia, and substance use disorders; and those with no history of a psychiatric disorder. Participants with PTSD and with other psychiatric disorders endorsed a greater number of somatic symptoms than those with no psychiatric disorder. Furthermore, participants with PTSD had significantly more somatic complaints than those with other psychiatric disorders.
The study we report here was conducted to compare reports of medical problems by primary care patients who have PTSD or a history of trauma and by patients who have other anxiety disorders. We were interested in the relationship between PTSD and somatic complaints in a sample of patients who had experienced a range of trauma, mostly in civilian contexts.
We hypothesized that, as in the study by Andreski and associates (
13), patients with PTSD would endorse a greater number of medical problems than patients with other anxiety disorders. The few studies that have examined the relationship between noncombat trauma and medical problems have typically reported on individuals with a history of trauma, rather than specifically examining the impact of PTSD. Thus we were also interested in whether a greater number of reports of medical problems could be attributed to PTSD specifically, or only to a trauma history in general.
Furthermore, individuals who have PTSD may differ from those who do not in lifestyle factors that may affect general health. For example, Solomon and colleagues (
6,
8) found that combat veterans with PTSD reported an increase in alcohol consumption and smoking after their war service. Thus in our study we also examined whether lifestyle factors such as exercise, use of tobacco, and substance abuse could account for any difference in reported medical problems.
Finally, we addressed another shortcoming of the research to date. In the studies reviewed, it was unclear whether the elevated rates of reported medical problems among persons with a trauma history were due primarily to physical injury that this group suffered as part of the trauma. Thus we examined whether any increase in medical problems reported by participants with PTSD might be associated with having suffered a physical injury.
Methods
Participants
This study was part of the larger Primary Care Anxiety Research Project, a naturalistic, longitudinal study of anxiety disorders among primary care patients. Participants were recruited from 15 internal medicine and family medicine practices in New Hampshire, Massachusetts, Rhode Island, and Vermont. Five sites were located in rural areas and ten in urban or suburban areas. Four of the sites were small, private practices, four were freestanding clinics with a university affiliation, and seven were large university teaching hospital-based clinics.
Recruitment began in July 1997. Inclusion criteria were that participants be English speakers, be at least 18 years of age, and have a general medical appointment scheduled on the day of recruitment. Exclusion criteria were active psychosis, no current address and phone number, and pregnancy.
Participants were recruited at the time they made a visit to the medical practice. A research assistant approached eligible clinic patients in the practice waiting room. Of a total of 11,909 eligible patients who were approached, 3,801 (32 percent) completed a questionnaire screening for symptoms of anxiety; the remainder declined to complete the screening form.
Of those who completed the questionnaire, 2,575 (68 percent) screened positive for anxiety symptoms and were scheduled for an assessment with the Structured Clinical Interview for DSM-IV (SCID) (
14). Of these, 398 declined to participate in the interview, and 677 repeatedly cancelled or failed to show up for their SCID appointments. The SCID was administered to 1,500 patients. Current anxiety disorders, current major depression, and lifetime substance abuse and dependence were assessed with the SCID.
Of the 1,500 patients who completed the SCID, 502 met diagnostic criteria for one or more of the following index disorders and were enrolled in the study: panic disorder with or without agoraphobia, agoraphobia without a history of panic disorder, generalized anxiety disorder, social phobia, PTSD, mixed anxiety-depressive disorder, and generalized anxiety disorder features occurring exclusively during the course of a mood disorder. This last category was created to include individuals who met the DSM-IV criteria for generalized anxiety disorder, with the exception that their symptoms occurred exclusively during the course of a mood disorder.
Measures
The screening questionnaire, developed for the Primary Care Anxiety Project, is a self-report measure inquiring about the presence of essential features of DSM-IV anxiety disorders. The form was designed to be highly sensitive to the presence of an anxiety disorder. In a separate validation study of the questionnaire, 64 primary care patients completed both the screening form and the SCID. The interviewers administering the SCID were blind to the results of the screening measure. Thirty-eight of the 64 patients screened negative, and none of the 38 met criteria for an anxiety disorder according to the SCID; there were no false negatives. Twenty-six of the 64 patients screened positive. Eight (31 percent) of them were true positives—that is, they also met criteria for an anxiety disorder according to the SCID—and 18 (69 percent) were false positives—that is, they did not meet SCID criteria for an anxiety disorder. One patient who screened negative was excluded at the time of the SCID for psychotic symptoms.
Trauma history was assessed with a revised version of the Trauma Assessment for Adults (TAA) (
15). This structured interview is designed to assess exposure to extreme events such as military combat, motor vehicle accidents, physical or sexual assault, and witnessing the severe injury or assault of another person. The TAA is a brief version of the Potential Stressful Events Interview (
16), which was developed for use in the
DSM-IV field trial.
A medical history form designed for the study was used to assess health status. The medical history form is an interviewer-administered questionnaire in which participants are asked whether they have ever had, or currently have, any of 18 illnesses or medical problems, and they are asked to report any medical problems that are not on the list. Interviewees are also asked about lifetime use of tobacco and current regular exercise.
Analyses were conducted with SAS version 8.0, using PROC FREQ, PROC ANOVA, PROC NPAR1WAY, and PROC LOGISTIC. Between-group differences were examined with analysis of variance (ANOVA) and chi square analyses. Listwise linear regression was used to identify predictors of the number of medical conditions. Logistical regression analysis was used to examine predictors of specific medical conditions.
Results
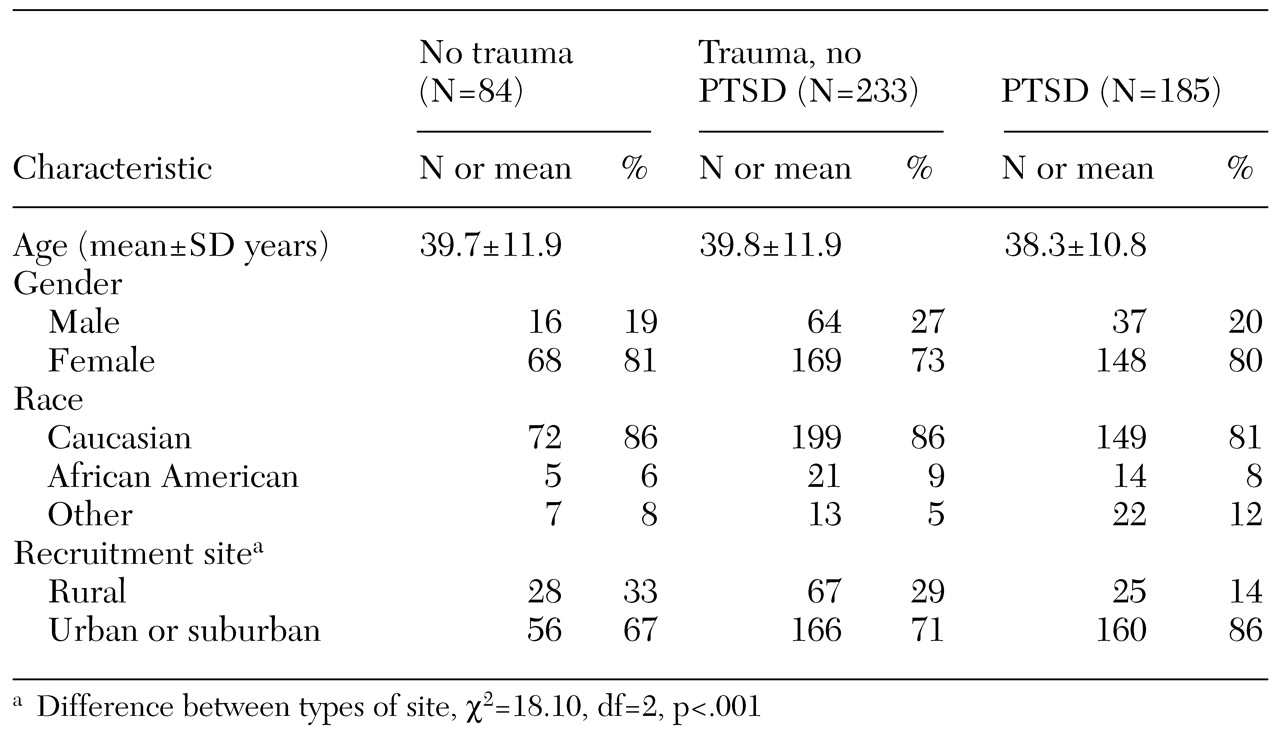
The demographic characteristics of the sample are presented by trauma status in
Table 1. Of the 502 participants who met criteria for at least one anxiety disorder, 84 (17 percent) reported no history of trauma, 233 (46 percent) reported a history of trauma but did not meet criteria for a current episode of PTSD, and 185 (37 percent) were diagnosed as having PTSD. Participants with PTSD were more likely to have been recruited from an urban or suburban site than from a rural one.
The most commonly reported traumas were forced sexual contact or rape (endorsed by 45 percent of the total sample), accident (38 percent), witnessing someone being injured or killed (37 percent), and an attack without a weapon (32 percent). Military trauma was the least common, endorsed by only 3 percent of the sample.
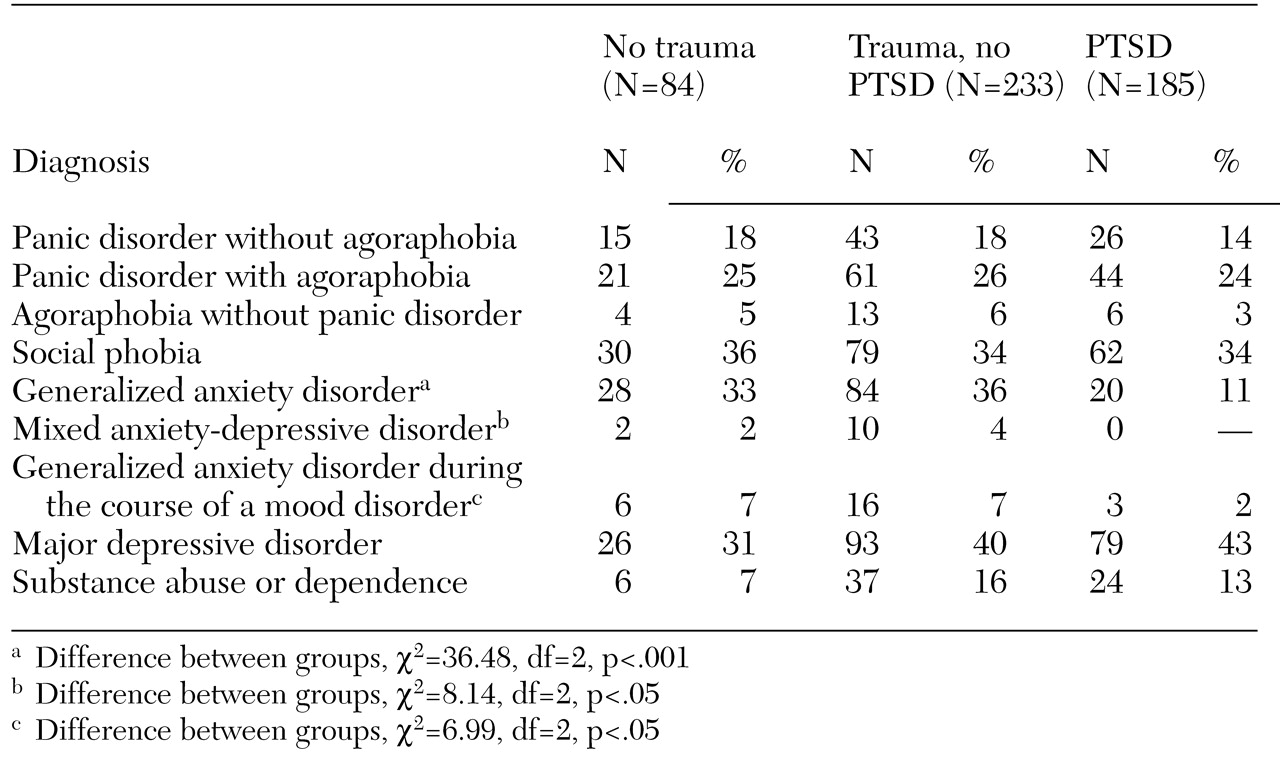
Table 2 details the diagnostic categorization of the sample. Rates of most anxiety disorders and comorbid major depressive disorder and substance use disorder did not differ between participants with no history of trauma, those with a history of trauma, and those with PTSD.
Differences in the number of medical conditions
The total number of nonpsychiatric illnesses or medical problems reported on the medical history form was compared for the three groups. ANOVA revealed a significant group effect on the lifetime number of medical problems (F=22.61, df=2, 498, p<.001). Follow-up analysis with Duncan's multiple range test indicated that all groups differed from one another. Participants who had PTSD reported significantly more lifetime medical problems (mean± SD=4.46±2.69) than either of the two groups of participants who did not have PTSD. Participants who had a history of trauma reported a greater lifetime number of medical problems (mean±SD=3.28±2.13) than those without a trauma history (mean±SD= 2.65±1.64).
Similarly, a significant between-group difference was found for the number of current medical problems (F=16.44, df=2, 497, p<.001). Duncan's test again revealed significant differences between the three groups; the mean±SD number of current medical problems for participants with PTSD was 3.18±2.2; for those with a history of trauma, 2.40±1.8; and for those with no trauma history, 1.86±1.34.
Predictors of the number of medical conditions
History of physical injury, lifetime use of tobacco, current regular exercise, lifetime substance use disorders, PTSD, and trauma history were explored as potential predictors of the number of medical illnesses. Age, gender, recruitment site, current major depression, and current diagnosis of each of the other anxiety disorders were also included as potential predictors in the analyses described below.
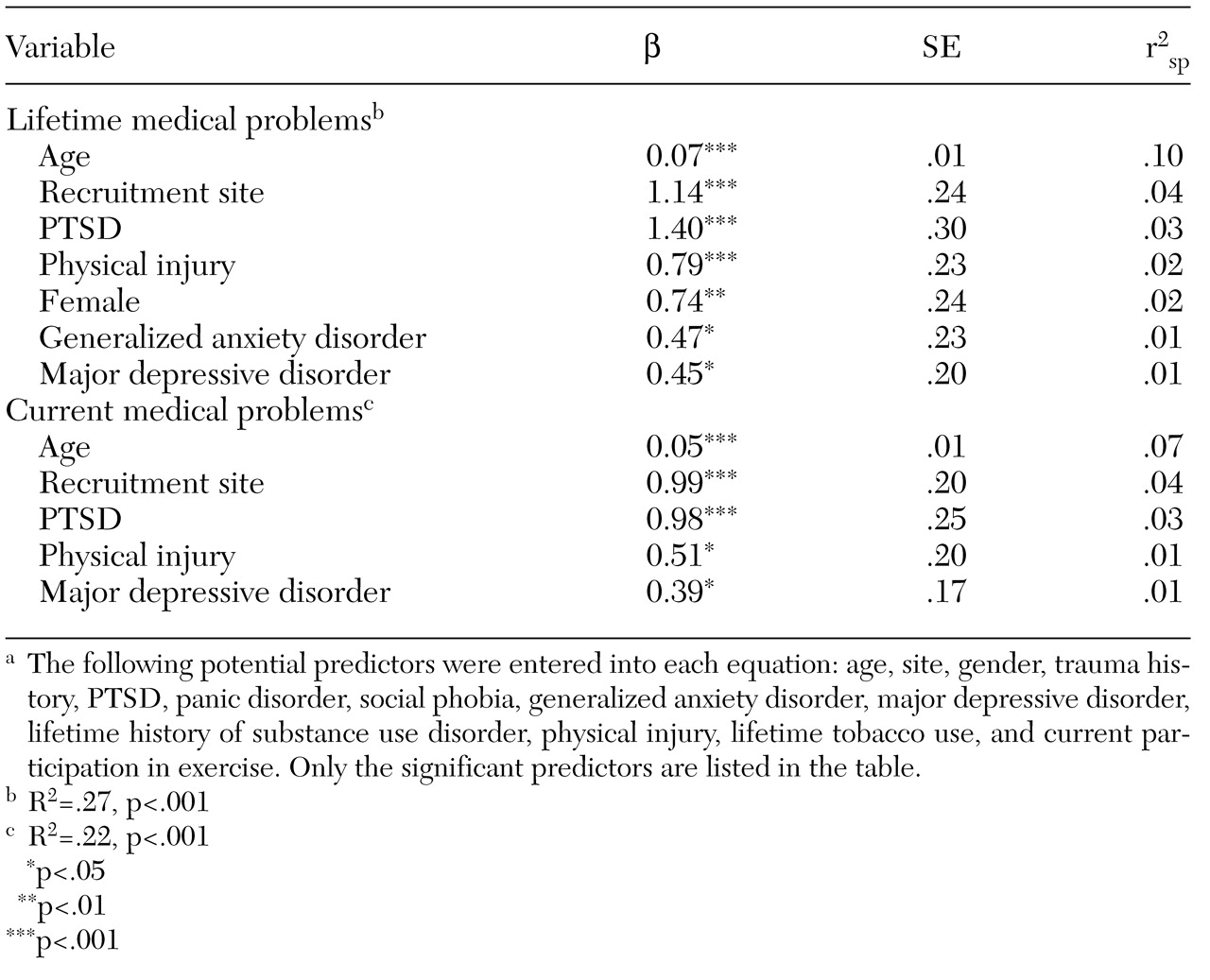
Listwise multiple regression analyses were used to examine the relative contribution of each of these variables to the number of medical conditions reported. The first regression equation examined predictors of the lifetime number of medical problems. The results are summarized in
Table 3. PTSD was a significant predictor of the lifetime number of medical problems and accounted for 3 percent of the variance. Age, location of recruitment site (urban or suburban versus rural), a history of physical injury, being female, having generalized anxiety disorder, and having major depressive disorder were also significantly associated with the lifetime number of medical conditions reported. No anxiety disorder other than PTSD and generalized anxiety disorder was a significant predictor of the number of lifetime medical problems. Lifestyle factors were not significant predictors of the lifetime number of medical conditions.
A similar analysis was conducted in which the number of current medical conditions was used as the criterion. The results are summarized in
Table 3. In this equation, too, PTSD was a significant predictor. Age, site location, physical injury, and major depressive disorder were the only other significant predictors of the number of current medical conditions reported.
Differences in rates of medical conditions
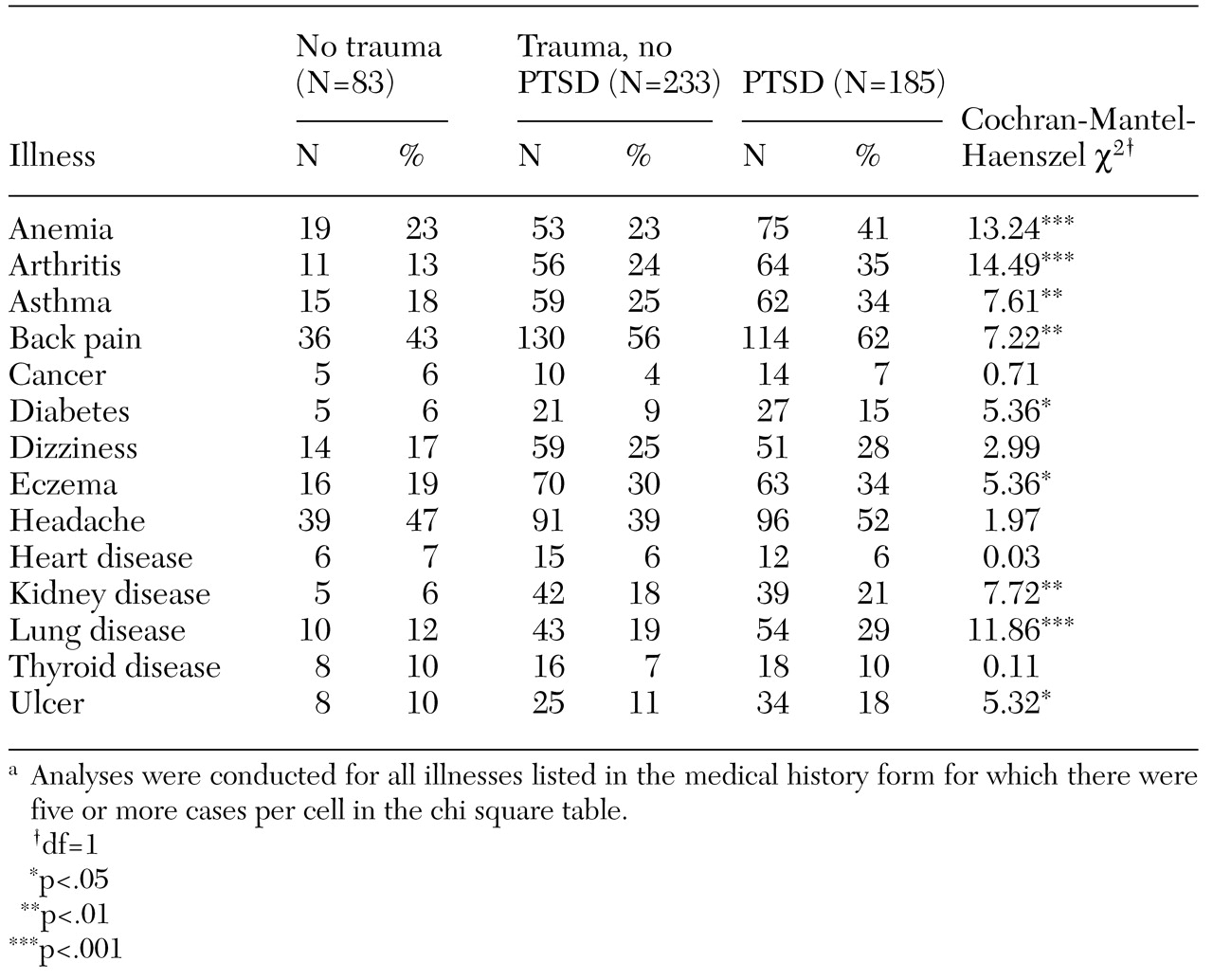
Rates of endorsement of each of the 18 somatic problems were examined between participants with no trauma history, those with a history of trauma but without PTSD, and those with PTSD. Four of the 18 problems—epilepsy, liver disease, phlebitis, and stroke—were endorsed so infrequently that comparisons could not be conducted with adequate statistical power, and so these variables were excluded.
Table 4 lists the rates of the remaining medical conditions and the results of between-group comparisons made with the Cochran-Mantel-Haenszel chi square test. Reported rates of anemia, arthritis, asthma, back pain, diabetes, eczema, kidney disease, lung disease, and ulcer differed significantly between groups. Examination of the means showed that the highest rates of these medical illnesses were reported by the PTSD group, and the lowest rates by participants with no trauma history. No differences between groups were found for cancer, dizziness, headache, heart disease, and thyroid disease.
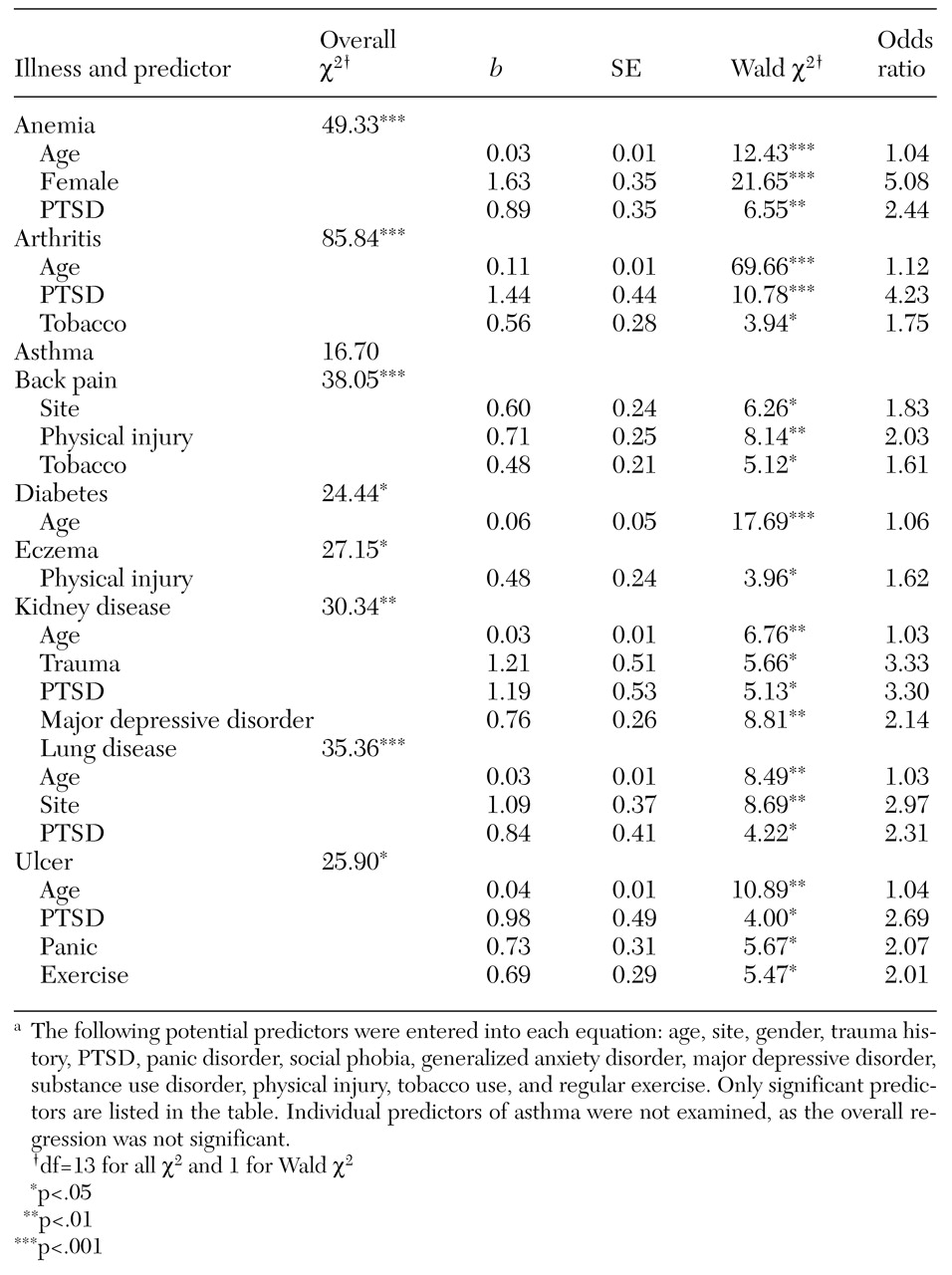
Predictors of medical conditions
Each of the nine medical conditions for which a between-group difference was found served as the outcome variable in a logistical regression analysis. PTSD, age, gender, recruitment site, trauma history, history of physical injury, current use of regular exercise, lifetime tobacco use, lifetime substance use disorder, current major depression, and each of the other current anxiety disorders were examined as potential predictors. The results are presented in
Table 5. Significant associations were found for the likelihood of ever having had anemia, arthritis, back pain, diabetes, eczema, kidney disease, lung disease, and ulcer. With all other variables in the equation controlled for, participants with PTSD were more than twice as likely as those without PTSD to report anemia, lung disease, or an ulcer; more than three times as likely to report kidney disease; and more than four times as likely to report arthritis.
Discussion
In a sample of individuals seeking help in a primary care setting for general medical problems, PTSD was associated with a higher rate of medical complaints. Study participants with PTSD reported more current and lifetime medical conditions and were more likely to endorse a number of specific medical problems.
To our knowledge, this is the first study to examine unique contributions to the relationship between PTSD and medical problems in a primary care sample. Interestingly, the higher rate of reported medical conditions among participants with PTSD could not be explained by a current mood or anxiety disorder other than PTSD, lifestyle factors, a history of physical injury, or a history of trauma. When these factors were accounted for in the linear regression models, PTSD still predicted a significant though small proportion of the variance in the somatic problems reported by participants.
Substance use disorders, regular exercise, and the use of tobacco did not significantly predict the number of reported medical problems. Furthermore, when these lifestyle factors were controlled for, PTSD remained significantly associated with a greater likelihood of ever having had anemia, arthritis, kidney disease, lung disease, or ulcer. Aside from the relationship between lifetime tobacco use and arthritis and back pain, the lifestyle factors generally were not found to be significantly associated with a greater likelihood of having the specific illnesses. Although in this sample lifetime tobacco use was not significantly associated with the likelihood of having lung disease, the data showed a trend toward significance (p<.07).
The lack of a relationship between the lifestyle factors and the number of medical problems reported was surprising, although the item about tobacco use simply assessed whether or not participants had ever smoked or used tobacco. The frequency and duration of tobacco use and the number of cigarettes smoked per day were not assessed. It may be that our study participants, with a mean age of 39 years, were too young to have suffered the effects of these lifestyle factors yet.
A history of physical injury was associated with the reported lifetime number of illnesses, although this variable accounted for less of the variance than did PTSD. Furthermore, trauma history itself was not associated with a higher reported number of medical problems. The impact of PTSD was greater than that of trauma alone.
A possible explanation for this finding is that individuals with PTSD may be more likely than individuals with other anxiety disorders to overreport medical complaints. Such overreporting may be common among patients with PTSD (
17,
18) and with trauma histories (
19,
20,
21,
22,
23). Our study's reliance on self-report of medical conditions is a limitation in this regard; we do not know whether participants who reported more medical problems would actually exhibit signs and symptoms of these problems on examination.
Our findings may depict a difference in the perception of medical illness or in somatization. However, the three groups—participants with PTSD, those with a history of trauma only, and those with no trauma history—did not differ in their reporting of medical conditions that might most commonly be associated with somatization disorder. No differences were found between the groups in reports of dizziness or headache, for example. Rather, the groups differed in their reporting of problems such as lung disease, diabetes, and anemia.
It is also possible that patients with PTSD differed as a group from those without PTSD on individual variables that predated their trauma. These variables may have led to both a greater likelihood of PTSD and a greater likelihood of medical illness or a greater tendency to overreport medical complaints. One such variable might be personality traits. For example, individuals with a high degree of histrionic, borderline, or antisocial personality traits may be more likely to take risks and thus be more susceptible to trauma. By virtue of their personality, they may also be more likely to present with numerous physical complaints. However, axis II personality traits were not assessed in this study.
Preexisting medical or psychiatric illness might also be a factor. For example, a preexisting illness might increase vulnerability to trauma or to PTSD. However, we tested this hypothesis by examining whether medical and psychiatric illnesses predated the first trauma among participants in the different groups (data not shown) and found that participants with PTSD did not have a higher rate of medical or psychiatric illness before their trauma experience than those without PTSD.
Another possible explanation for our findings is that PTSD is associated with biological changes that may lead to a higher rate of medical problems. Ironson and associates (
24) found that a greater severity of PTSD symptoms among survivors of Hurricane Andrew was associated with lower immune functioning. Wolfe and colleagues (
9) suggested that PTSD symptoms such as hyperarousal and numbing may lead to a greater risk of cardiovascular and gastrointestinal disturbances. Solomon (
6) suggested that PTSD itself constitutes a highly stressful situation and that this chronic stress may lead to greater vulnerability to physical disorders. In our study, however, all participants met
DSM-IV criteria for at least one anxiety disorder. Thus, those who did not suffer from PTSD had problems characterized by some degree of hyperarousal symptoms and chronic stress.
Another limitation of our study was the lack of a control group of participants who did not have a psychiatric disorder. Thus, although the primary care patients in our sample who had PTSD reported significantly more medical problems than those who had anxiety disorders but not PTSD, we do not know how they would have compared with primary care patients without mental disorders.
Conclusions
It is of particular interest that PTSD was related to a higher rate of reported medical problems. Further research is needed to better understand factors that account for the higher rates of medical complaints by individuals who have been traumatized or who have PTSD. The Primary Care Anxiety Research Project will follow the course of PTSD and medical problems in our sample. Through this longitudinal research, we will be able to examine whether alleviation of PTSD symptoms coincides with a reduction in reported medical problems. Research is also needed to learn whether treatment of PTSD symptoms would serve to alleviate somatic complaints.
If is important to bear in mind that individuals who have been traumatized are more likely to seek treatment at a general medical center than in a mental health setting (
1). Given the greater rate of medical complaints accounted for by PTSD and trauma, our data suggest that traumatized individuals are likely to present with multiple nonpsychiatric medical concerns.
Acknowledgments
The Primary Care Anxiety Research Project is supported by an unrestricted grant from Pfizer Pharmaceuticals, Inc. The authors thank Jenifer Allsworth, Ph.D., for her statistical assistance with early drafts of this article.