The terrorist attacks on the United States on September 11, 2001, were without precedent, as was the immediate national need for mental health interventions that followed. Pre-September 11 literature on posttraumatic interventions examined the effects of such services on veterans, police, burn victims, and victims of rape, assault, shootings, and auto accidents. Local studies focusing on large groups have examined natural disasters and the Oklahoma City bombing.
Research on grief and grieving has shown that recovery is more difficult when a loss is sudden and unexpected. Unlike traumatic events associated with terrorism, natural disasters tend to have a clear beginning and end and are characterized by a rapid return to a more familiar sense of predictability and control of the environment and a diminishment of feelings of vulnerability and insecurity.
Recent events highlighted unanticipated widespread psychosocial dislocation and demand for services. Calls for help to a national managed behavioral health organization (MBHO) poured in: "I witnessed people jumping out of the World Trade Center. I can't sleep and can't stop shaking and worrying." "I am embarrassed that I leave work when other people stay and keep working. Today we had two bomb scares at our temporary job location. The bomb scares put me over the edge, and I had to leave work. I just need to talk to someone about whether I am going crazy or not." "I work for one of the national airlines as a flight attendant. I don't want to return to work. I am having nightmares, not eating well; I am nervous and afraid. I don't feel like I can get on an airplane." "My husband is a firefighter who is missing in the disaster. I don't know what I am going to tell our children." "I lost two coworkers who were on one of the planes that crashed. I am too depressed to get out of bed, and yet I can't sleep." "I keep thinking and seeing the World Trade Center collapsing again and again and again. I had to run for my life!"
The extraordinary catastrophic events of September 11 have focused attention on the unprecedented need for rapid access to education about trauma and grief and to psychological services. The attacks also underscored the absence of a national system for emergency care of large dispersed populations. In this column I illustrate how organized specialty mental health systems could mobilize resources in the service of furthering the design and operation of a single, integrated, national emergency disaster response system.
Historically, disaster response efforts have emerged in parallel fashion. The most familiar effort is the attempt to coordinate federal agencies with state and local government resources, along with spontaneous local volunteer services, which may or may not be coordinated and which have varying degrees of visibility. A third, newly emerging type of disaster response reflects the potential role of private-sector national MBHOs. Most working Americans and some Medicaid and Medicare recipients have mental health benefits that are managed by MBHOs.
The three largest of the national MBHOs—Magellan, Value Options, and United Behavioral Health (UBH) —cover more than 120 million employees and their families. For years, the MBHOs have provided crisis intervention services on request to employers across the country. In a typical crisis intervention, a mental health specialist responds rapidly and provides on-site care for local trauma. This type of response is called critical incident stress debriefing. However, September 11 was different, and the way that MBHOs responded illustrates how they may contribute to a national disaster response system, one that can be expanded and improved to complement other systems. Public health can be best served by moving toward a single national system that incorporates and integrates all available resources from both the public and private sectors. UBH's experiences after the events of September 11 should contribute to policy makers' understanding of best-practice responses to these situations.
The United Behavioral Health intake line
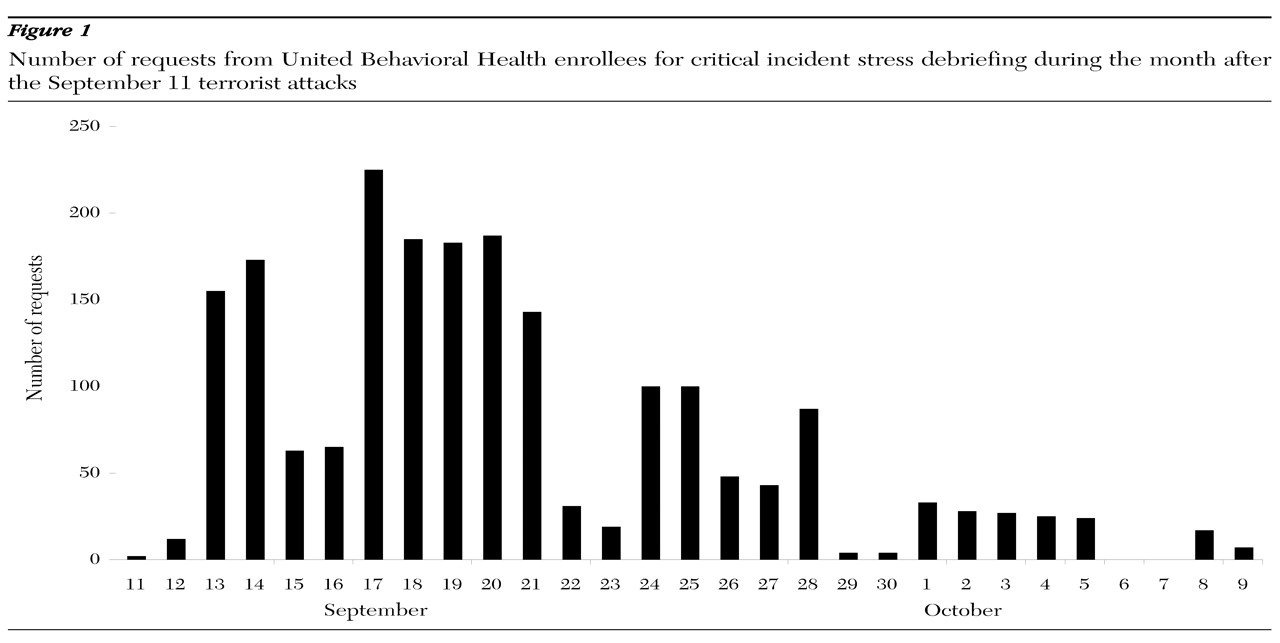
Data were gathered from UBH in October 2001 to capture the first month's requests for professional services and the response to a disaster that took place at three sites—at the World Trade Center, at the Pentagon, and on planes. Requests for critical incident services came mainly from large employers who had been based in or near the Twin Towers or who had been affected by the plane crashes. UBH's first line of response for its employer customers was its office located less than a mile from Ground Zero. The second line of response was a national toll-free number, which provided immediate access to the critical incident stress debriefing coordinators. In response to every request, a UBH network clinician was present at the employment site within 24 to 48 hours. The pattern of response is illustrated in
Figure 1.
As would be expected, the first day was mainly one of shock. The calls for help began to peak by the third day, slackened somewhat on the weekend, and jumped the following Monday. The second week was the major peak period for requests. Requests gradually diminished over the next three weeks. Not reflected in
Figure 1 are an additional 1,000 calls that were received by the employee assistance program of UBH's Working Solutions Division in the two weeks after September 11. These callers received telephone counseling on the employee assistance program's advice lines or were referred for face-to-face clinical care.
Because several employers based in the World Trade Center were UBH customers, the number of requests for critical incident stress debriefing was very high. Some of these companies had other offices throughout the country that also required on-site services. Thirteen companies had employees who died in the tragedy, either on the ground or in the plane crashes. Large numbers of initial requests for individual assistance came from people who were currently in treatment or who had previously used mental health services. Employers and employees also called with concerns about coverage and eligibility for services. Unexpected risk groups appeared, such as grandparents who were feeling overwhelmed by loss coupled with new, unanticipated responsibilities. All limits and restrictions were removed. In October, requests for disability status steadily increased.
Caregiving responses
New York City and Washington, D.C., are rich in mental health resources. Individual clinicians and local professional mental health organizations rapidly volunteered pro bono assistance. In New York City, the human resource and benefit managers of affected employers immediately contacted their MBHOs or employee assistance programs to request on-site assistance. Continuous group meetings were provided wherever employees were located or relocated, including at work sites dispersed throughout the nation. Initial group critical incident stress debriefings, which are mainly educational, frequently led to requests for individual appointments with the debriefers (50 to 65 percent of those debriefed), often on an urgent basis. Such appointments were granted regardless of eligibility or individual coverage. Critical incident stress debriefing services do not incur copayments.
Internal employee assistance programs or those that were contracted to local organizations were frequently overwhelmed early, and assistance was requested from the MBHO. Flexible responses included placing network clinicians in lower Manhattan walk-in clinics. Seven UBH care managers (mental health professionals) were placed at the new temporary sites of the largest employer from the World Trade Center for the first week, in addition to 40 local network specialists in critical incident stress debriefing. During this first week, 80 percent of network clinicians who were polled in test calls in one state agreed to make crisis appointments available immediately.
In the month after the terrorist attacks, only a slight increase was observed in the number of requests for individual or family mental health or substance abuse treatment (data not shown). However, preliminary data inform us that there was a major increase in the prescribing of antianxiety medications, mainly by nonpsychiatric physicians. Anecdotally, the delay in seeking specialty professional help or the substitution of nonpsychiatric care may have been due to individuals' seeking religious solace coupled with the immediate outpouring of support and universal expression of grief and trauma. Shared openness about posttraumatic experiences provided a new and unexpected "normalization" process that encouraged the articulation of anxiety, fear, and sadness.
From previous experience it was understood in advance that helpers also need help. Critical incident stress debriefing specialists and other mental health specialists can become overwhelmed. Even specialist debriefers need debriefing. A hotline for clinicians was set up and was being used by the beginning of the second week.
Discussion and policy implications
Rapid access to appropriate clinical resources is to psychological trauma what vaccines and antibiotics are to infectious diseases and bioterrorism. However, psychological trauma is quintessentially subjective and individualistic. The volume and intensity of the response were correlated with the proximity to the destruction. Studies show a strong sympathetic response to local community trauma and loss, referred to as communal bereavement. Additional responses are often produced by secondary reinforcers, such as bomb threats, repeated exposure to shocking televised images, the threat of hostility, and incidents of bioterrorism. In addition to the people directly affected, former trauma victims often experience significant, intense early responses. Trauma contagion appears to intensify when children are involved (
1,
2,
3,
4,
5,
6,
7).
The events of September 11 produced a public health emergency that necessitated unprecedented responses in both the public and the private sector. This brief and early descriptive study has shown the enormity of the immediate need felt by employers. It has also illustrated the heretofore unrecognized role of one care system—the private-sector employer-based MBHOs—in large-scale crisis management. This sector has important contributions to make, having resources in place, available, and accessible for more than 160 million employees and their families.
The national delivery systems have depth and redundancy. They are accountable and data driven. They could be integrated and coordinated with public services to enhance the rapidity and intensity of the most appropriate response, avoid redundancy, and provide focused care locally and nationwide. MBHOs' electronic information system data banks are massive and stable. They can track individual and group response and service use over time, facilitating the delivery of care to individuals, families, or special populations. The Federal Emergency Preparedness initiative faces enormous time pressure. Both the Federal Emergency Management Agency (FEMA) and the Substance Abuse and Mental Health Services Administration (SAMHSA) could usefully incorporate both the experiences and infrastructure capabilities of the MBHOs to support their mission.
In widespread disasters, spontaneous volunteers can be maximally effective if they can be rapidly attached to functioning structures and focused on emerging needs. In addition, tens of thousands of mental health clinicians who are already in managed care networks are available, operating from their private offices nationwide. They are differentiated by skills in central databases and could be electronically connected in real time. This nacent system is not bound by the natural boundaries of state and local government and federal agencies. Psychiatrists in solo practice, who are often affiliated with clinics, hospitals, and academic institutions, can enhance the relevance of their volunteer efforts by attending now to how they can attach themselves to local organized disaster response efforts. Psychiatrists need to be current on the latest perspectives on critical incident interventions. The U.S. government should take advantage of the potential synergies of these national resources and use them in a coordinated manner with local, state, and national government organizations.
Acknowledgment
The author acknowledges the important contributions of Kris Luckin, Ph.D., and Loren McCarter, Ph.D.