The term "pervasive developmental disorders" (PDD) refers to a group of heterogeneous conditions that share a core triad of disturbances consisting of qualitative impairments in social interaction and verbal and nonverbal communication as well as repetitive and stereotyped patterns of interests and behavior (
1,
2,
3,
4,
5,
6). The diagnostic category is hypothesized as being a continuum or spectrum of autistic disorders (
1,
2,
3,
4,
5,
6).
The prevalence of autism has long been believed to be from two to four per 10,000 children, and it has been generally accepted that about 20 percent of children with the disorder are high functioning (
7,
8). Studies that have used broader definitions of autism and that have considered individuals within the entire autism spectrum have suggested that the prevalence of autistic disturbance may be as high as 90 per 10,000 children and that the proportion of children with IQs above 70 is far greater among children with PDD than among children with autism (
8,
9,
10,
11,
12).
In recent years, clinicians and researchers have commented on an apparent increase in the prevalence of PDD and have offered a number of explanations, including better recognition and diagnosis of the disorders, wider awareness of the existence of an autism spectrum of disorders, and an actual increase in the frequency of PDD. Although firm evidence for or against a real increase in the frequency of autistic disturbance does not exist, there is consensus that PDD is not rare (
1,
3,
7,
8,
9,
10,
11,
12,
13,
14).
Individuals with PDD may experience significant additional psychiatric disturbances (
1,
15). Among the disturbances that have been reported are schizophrenia, mania, depression, suicidal behavior, anxiety disorders, obsessive-compulsive disorder, substance use disorders, catatonia, paranoid ideation, Tourette's disorder, attention-deficit hyperactivity disorder (ADHD), aggressivity, temper outbursts, bizarre criminal behavior, preoccupation with weapons and violent themes, firesetting, inappropriate sexual behavior, school refusal, encopresis, enuresis, elective mutism, and eating and sleep disturbance (
1,
2,
3,
4,
5,
6,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37). Studies in which standardized assessment instruments and comparison samples were used have shown that children and adolescents with PDD are at increased risk of emotional and behavioral disturbance and are similar to youths in clinical comparison samples in a number of areas of psychiatric dysfunction (
1,
4,
19,
20,
21,
22,
31,
34,
35,
36).
Cases of co-occurrence of PDD and affective disorder and the results of family studies have suggested that a significant relationship may exist among autism-spectrum disorders, affective disturbance, social phobia, anxiety disorders, and substance use disorders (
1,
4,
15,
17,
38,
39,
40). Cases of co-occurrence of schizophrenia and PDD have been described, and a number of studies have reported a history of PDD among some children and adolescents who developed schizophrenia (
1,
4,
6,
17,
26,
28,
29,
30).
Research on the co-occurrence of Tourette's disorder and PDD has suggested that tic disorder and PDD are significantly related; cases of concordance of Tourette's disorder, PDD, and schizophrenia and cases of Tourette's disorder, PDD, and bipolar disorder have suggested that Tourette's disorder and PDD share etiologic factors with bipolar disorder and schizophrenia (
1,
24,
26,
31,
32). Of additional interest is the hypothesis that the Tourette's disorder spectrum of disorders is identical to the family of disorders that constitute the affective spectrum, obsessive-compulsive spectrum, and attention-deficit spectrum disorders (
41,
42,
43).
Despite the high prevalence of comorbid psychiatric disturbances among children and adolescents with PDD, few studies have examined the prevalence of PDD in samples of psychiatric patients. What little research exists suggests that children and adolescents with PDD represent a significant subgroup of severely ill patients referred for psychiatric treatment (
1,
23,
27,
33).
In this study we sought to determine the prevalence of PDD in a sample of children and adolescents admitted to a state hospital psychiatric day treatment service and to characterize the pattern of psychiatric disturbances experienced by these patients.
Methods
Sagamore Children's Psychiatric Center is a psychiatric facility operated under the auspices of the New York State Office of Mental Health. The center serves children and adolescents up to the age of 18 years who reside in the Long Island counties of Nassau and Suffolk. The day treatment programs are structured, nonresidential mental health programs with integrated public school educational services designed to provide alternative levels of treatment for children and adolescents with serious emotional disturbance who otherwise would be unable to be maintained in the community.
A total of 146 children and adolescents consecutively admitted to the day treatment programs between September 1, 1992, and June 30, 1995, were included in the study. Patients who had PDD were identified by chart diagnoses, which were formulated by the program psychiatrists. Psychiatrists and staff were unaware that a survey was being conducted at the time patients were evaluated for admission.
After patients with PDD were identified, the first author used DSM-IV criteria to confirm the diagnosis of PDD after interviewing each patient and reviewing the patient's clinical record. This review was part of clinical case assessments conducted routinely by the first author, the center's clinical director. Clinical records included the patient's history, which was provided by the parents or caregivers, and information obtained from the patient's previous psychiatric and pediatric service providers, from staff in educational settings in which the patient had been placed, and from observations of the patient's behavior and social interaction while he or she attended day treatment. Information gathered included reasons for referral; history of developmental abnormality, psychiatric disorders, and hospitalization; educational history; age at diagnosis of PDD; and family history of psychiatric disorders and Tourette's disorder.
The comparison sample consisted of 25 patients who were admitted to day treatment and who did not have PDD. Each individual in this group was matched retrospectively for age and sex with a patient who had PDD.
Principles governing the conduct of medical research involving human subjects as outlined by the Declaration of Helsinki were followed.
Results
Of the 146 patients, 20 (14 percent) met criteria for PDD. Of the 33 patients in the sample who were children (aged six to 12 years), ten (30 percent) had PDD. A total of 113 patients were adolescents, and ten (9 percent) had PDD. Five additional patients with PDD who were attending day treatment at the start of the survey were included in the study. The sample of patients with PDD consisted of 20 boys and five girls. The cases of two of the boys have been previously described (
27). Except for two boys who were African American, all the patients in the sample were Caucasian.
Of the 25 patients identified as having PDD, ten (40 percent) had been given the diagnosis of PDD by community physicians before they entered day treatment. In all, 17 of the 25 patients (68 percent) had been independently given a diagnosis of PDD by three or more medical providers. In the comparison sample, two patients had schizophrenia, 12 had ADHD-behavior disorder, two had schizoaffective disorder, three had a depressive disorder, one had bipolar disorder, three had major depression, and two had major depression with psychosis.
Patients with PDD were referred to day treatment for an array of difficulties, the combinations of which varied for each individual. Reasons for referral included failure to participate in and understand classroom routine, inability to accommodate change, social withdrawal and inability to establish peer relationships; inappropriate sexual behavior and verbalizations, and disorganized and bizarre verbal productions and behavior. The patients frequently exhibited anxiety, agitation, aggression, and disruptive behavior. Reasons for referral of children and adolescents in the comparison sample included academic difficulties, hyperactivity, aggression, disruptive behavior, school refusal, depression, and episodes of psychosis.
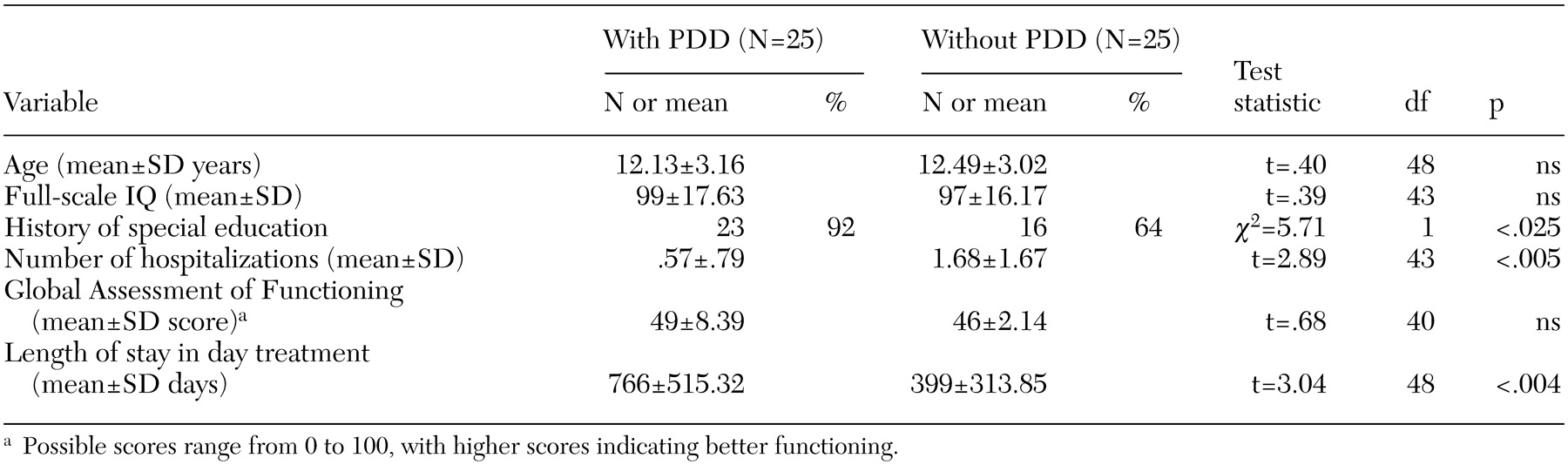
As shown in
Table 1, no significant differences were found in full-scale IQ or in scores on the Global Assessment of Functioning. Patients in the comparison group had significantly more hospitalizations. Nineteen patients in the comparison group (76 percent) had been hospitalized, compared with ten in the group with PDD (40 percent). Significantly more patients with PDD had a history of special education services. The mean stay in day treatment was significantly longer for patients with PDD.
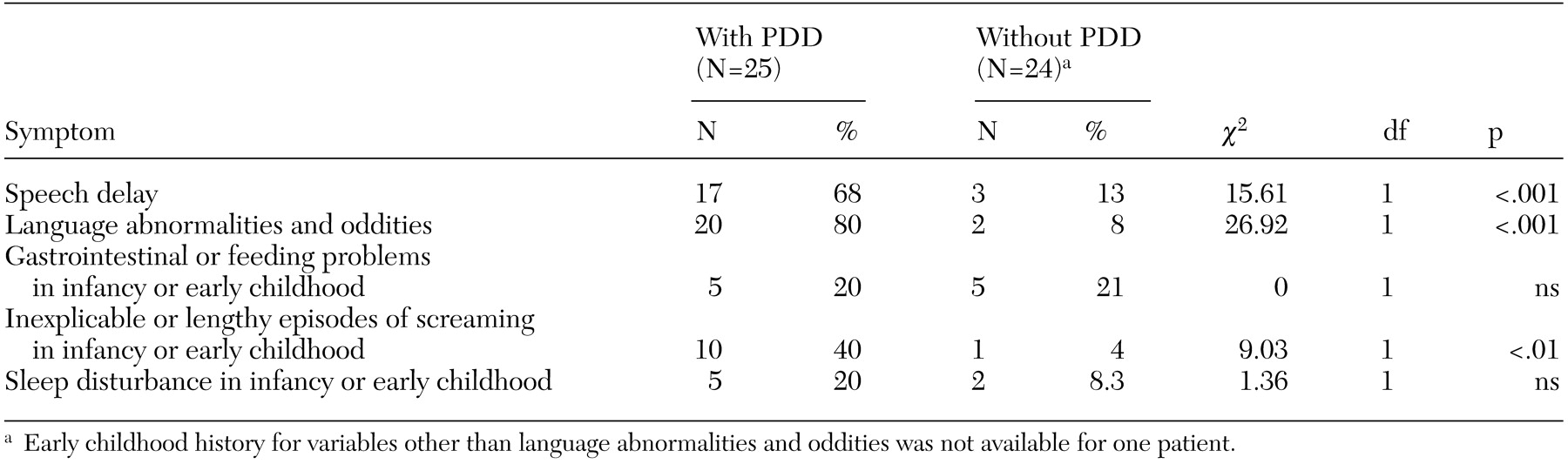
As shown in
Table 2, significantly more patients with PDD had a history of speech delay and language abnormalities. All except three patients with PDD had speech delay or language or communication abnormalities, including echolalia, tangentiality, irrelevance, loosening of association, and idiosyncratic use of language. The three patients who were the exceptions had a history of communication abnormalities characteristic of some individuals with autism-spectrum disorders: two showed monotonic speech, and one engaged in monologues on his special interests. Inexplicable or lengthy episodes of crying or screaming were also significantly more prevalent among patients with PDD.
The groups were compared on the age at which medical-psychiatric and educational interventions were first obtained because of developmental or behavioral disturbance. The mean±SD age at which professional intervention was obtained was significantly earlier for the patients with PDD (4.38±2.22 years compared with 7.73±3.32 years; t=5.04, df=48, p<.001). The educational system was the first to intervene for 20 of the children with PDD (80 percent). For the other five (20 percent), physicians were consulted first. Among patients in the comparison group, educational professionals were the first to be involved for 13 children (52 percent), and psychiatrists and other mental health providers were involved first in 12 cases (48 percent). Although patients with PDD had early abnormalities in speech acquisition and language or disturbances in behavior and social relatedness characteristic of PDD, the mean age at which the diagnosis of PDD was made was 9.85±4.02 years (range, 2.9 to 16 years).
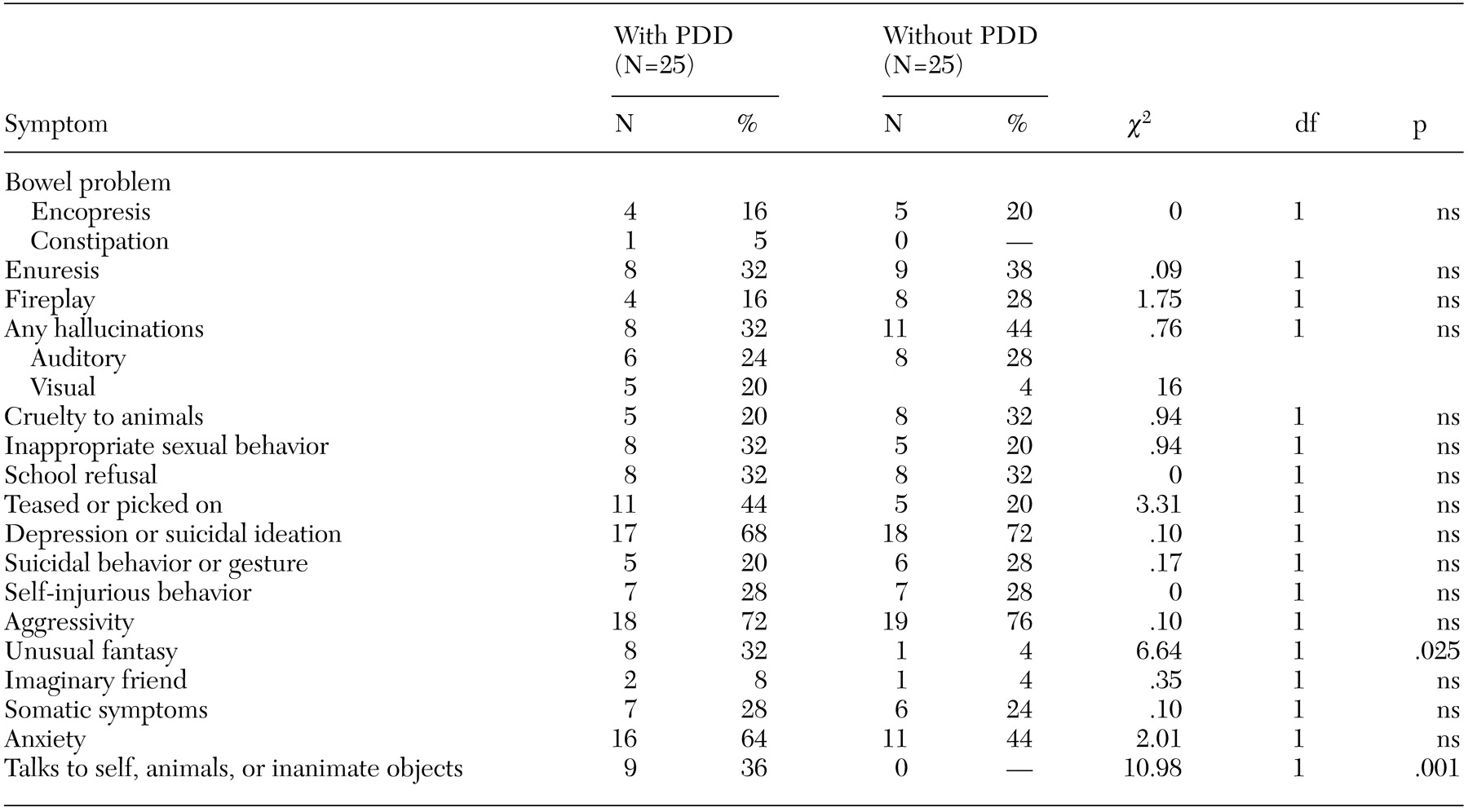
As shown in
Table 3, although patients with PDD had behavioral and psychiatric disturbances similar to those of the patients in the comparison group, two items distinguished the groups. Patients with PDD were significantly more likely to have a history of engaging in unusual fantasy and of talking to themselves, animals, or inanimate objects.
Eight patients with PDD engaged in serious and sometimes bizarre aggressive behavior. For example, one boy repetitively attacked his mother without apparent reason; one boy attempted to drown a younger sibling; and one adolescent, who collected knives and guns, was arrested after a gun he held accidentally fired and struck a peer whom he thought was about to attack him with a machete. The sexually inappropriate behaviors engaged in by patients with PDD included exhibitionism, frotteurism, sexual touching of others, utterance of lewd comments, and sexual preoccupations and thoughts.
Eight of the patients with PDD experienced hallucinations. This finding is of interest and adds to the growing recognition that some patients with PDD experience hallucinations. Among the eight patients, two girls and three boys had a diagnosis of childhood-onset schizophrenia with onset before the age of nine years. An additional girl and boy who showed bizarre and disorganized behavior and language had a diagnosis of childhood-onset schizophrenia. There was insufficient evidence to conclude that these patients experienced hallucinations or delusional thinking. For three boys who were reported to have experienced hallucinations, clinicians considered the hallucinatory experience to be episodic or stress related rather than chronic and persistent, and these children did not have a diagnosis of schizophrenia.
Eight of the patients with PDD had been given a diagnosis of tics or Tourette's disorder before referral to day treatment, and an additional 11 patients with PDD were given a diagnosis of tics after admission. Thus 19 of the 25 patients with PDD (76 percent) displayed tics. Eight (32 percent) had motor and vocal tics (not including echolalia). Of the seven children with PDD who had a diagnosis of childhood-onset schizophrenia, three also had a diagnosis of Tourette's disorder and four had a diagnosis of chronic motor tic disorder. In contrast, tic disorder was noted in the charts of four patients in the comparison group (16 percent).
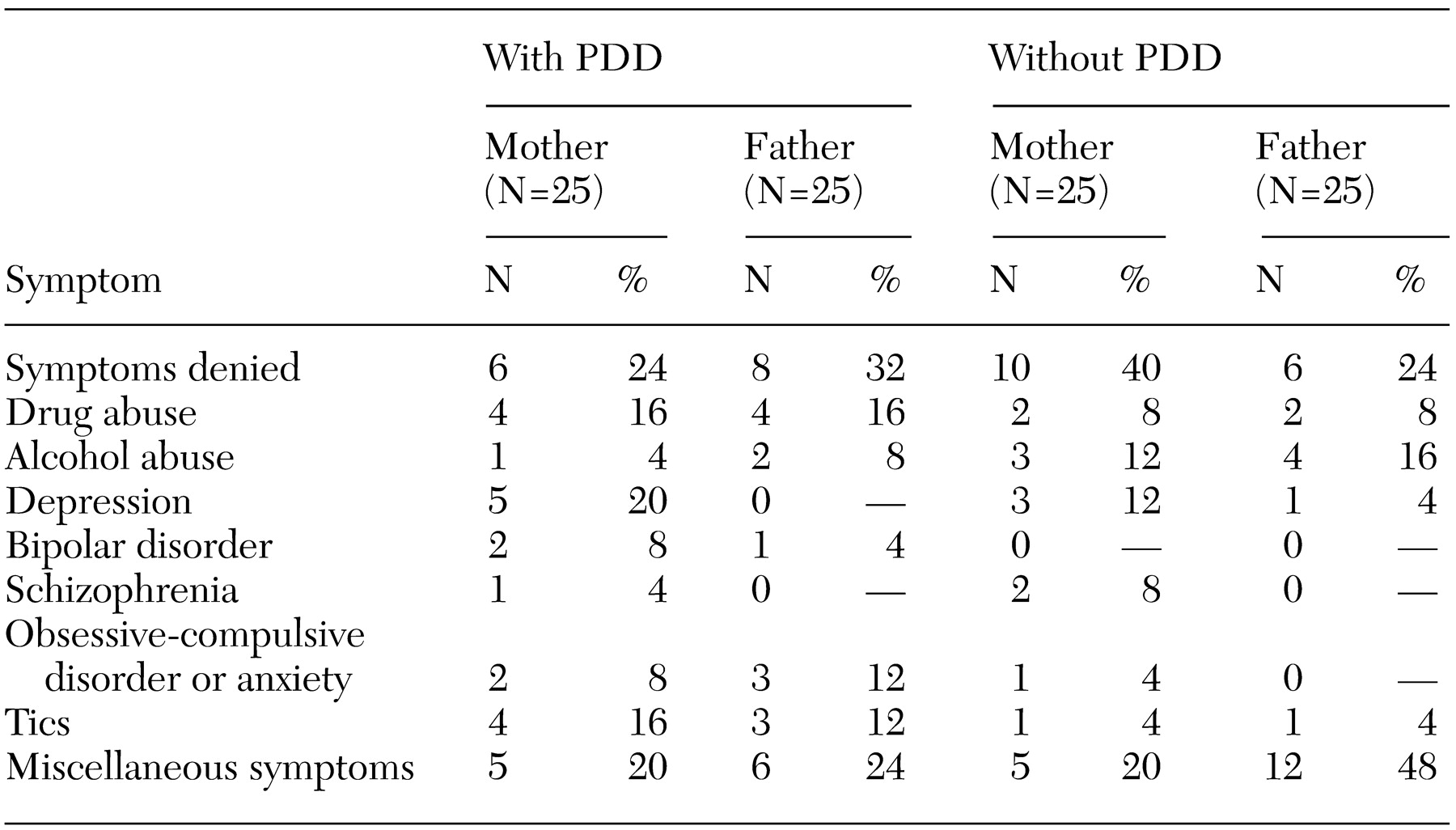
Table 4 provides information about patients' biological parents who were reported to have psychiatric disorders or symptoms. If a parent did not have a psychiatric or substance use diagnosis and did have behavior suggestive of impulse or temper dyscontrol or personality difficulties, the parent was considered to have a "miscellaneous" psychiatric symptom. When reports of psychiatric disturbances of extended family members were considered along with those of parents, such disturbances were present in both maternal and paternal families of 19 patients with PDD (76 percent) and 20 patients in the comparison group (80 percent). Schizophrenia was reported in the families of four patients with PDD and three patients in the comparison group.
Among patients with PDD who had a diagnosis of childhood-onset schizophrenia, schizophrenia was reported for one child's biological mother and for an extended family member of another child. A second cousin of a third patient was reported to have psychosis, and a maternal great aunt was reported to have talked to herself. The mother of another patient reported that she had experienced an episode of psychosis and had been given a diagnosis of bipolar disorder. Psychiatric hospitalization, institutionalization, or suicide was reported for an extended family member of another five patients with PDD and seven patients in the comparison group. Thus psychiatric disturbance in the families of both groups was considerable.
Discussion and conclusions
Fourteen percent of a sample of 146 children and adolescents with serious emotional disturbances who were consecutively admitted to psychiatric day treatment met criteria for PDD. This finding supports the view that PDD is not rare and may affect a significant proportion of children with serious emotional disturbance. Even though many of the children in this sample who had PDD had displayed signs of the disorder in early childhood, the mean age at which the diagnosis was made was 9.9 years. Others have noted that delays in the diagnosis of autism-spectrum disturbances are not uncommon, especially among children who are high functioning (
44).
Because PDD may be mild and may be associated with higher intellectual functioning, and because symptoms of the core syndrome may vary from one individual to another and may diminish in severity with age, the diagnosis of PDD may be easily missed (
1,
3,
4,
5,
21). In addition, many individuals with PDD have co-occurring psychiatric symptoms, which may further obscure the presence of the autistic process and may contribute to the delay in diagnosis (
1,
4,
21). The study reported here found that children who had PDD did not differ from those who did not have PDD in full-scale IQ, global functioning, and the presence of an array of psychiatric symptoms. These findings support the view that PDD may be easily missed because it may be mild and associated with psychiatric disturbances that are present in other severely ill youngsters.
Nevertheless, a number of clinical characteristics distinguished the two groups, which suggests that these features should alert clinicians to the possible presence of PDD. The features include a history of speech delay, language and communication abnormalities, episodes of inexplicable crying and screaming in infancy, and behavioral characteristics such as talking to oneself, animals, or inanimate objects and engaging in unusual fantasy (
1,
4,
6,
19,
20,
21,
22). Speech delay and abnormalities in language and communication are among the hallmark features of autistic disturbance and are readily reported by parents and caregivers (
1,
27). In addition, bizarre and aggressive ideation and behavior should alert clinicians to the possibility of underlying PDD (
1,
4,
15,
16,
18,
27,
37). Children and adolescents who have PDD frequently have comorbid obsessive-compulsive, anxiety, and depressive symptoms (
1,
27,
33,
35,
36). The patients with PDD in the study reported here had numerous such diagnoses: among 14 patients with PDD, the diagnoses of obsessive-compulsive disorder, separation anxiety, overanxious disorder, and social phobia were made 18 times, compared with ten times among eight patients in the comparison group.
Early recognition of PDD is important for parents and patients (
44,
45,
46,
47,
48). Once children with PDD are identified, appropriate interventions and supports can be provided to maximize cognitive and social growth and minimize stress and behavioral disturbance (
1,
4,
37,
44,
45,
46,
47,
48). In the study reported here, the children who had PDD experienced considerable distress in school settings, as evidenced by the frequent occurrence of anxiety, disorganized and agitated behavior, expression of depressive and suicidal thoughts, and school refusal. The finding that patients with PDD had significantly longer stays in the day treatment program suggests that children and their parents derived benefit from the support they received and were reluctant to transfer to less supportive programs. Furthermore, staff may have appreciated the need of these children for "sameness" and may have been reluctant to discharge them. In addition, teachers and other professionals in mainstream settings may have felt incapable of addressing the educational, emotional, and behavioral challenges presented by such children and may have been reluctant to accept them back into their programs.
The findings of this study highlight the importance of individualizing the school placements of children with PDD and for closely monitoring the progress of those who spend considerable time in mainstream settings. Children and adolescents with PDD are frequently bullied, teased, or assaulted by peers and may respond with aggression, conduct disturbance, depressed mood, suicidal behavior, and school refusal (
1,
4,
18,
27,
49). These considerations, along with the finding that educators are likely to be among the first professionals to be called on to intervene with children who have PDD, make it imperative that educators are familiar with autism-spectrum disorders and associated behavioral and emotional disturbances (
50).
In the group of children with PDD, seven (28 percent) also had either comorbid schizophrenia and either comorbid Tourette's disorder or chronic motor tic disorder. This finding has implications for the neurodevelopmental theory and etiology of schizophrenia (
1,
4,
26). Studies of the childhoods of patients who develop schizophrenia have consistently documented that a portion of patients experienced developmental defects in language; abnormalities in neuromotor functioning, including tics; and a history of symptoms of PDD (
1,
29,
51,
52,
53). Tourette's disorder is a common hereditary tic disorder (
1,
54,
55). Studies of psychiatric disorders among people with Tourette's disorder and their relatives have suggested that in addition to tics, the genetic abnormalities underlying Tourette's disorder may be expressed as a broad array of psychiatric disturbances, including hallucinatory experiences, paranoid ideation, and autism-spectrum disorder (
1,
24,
25,
26,
27,
54,
55).
It has been further hypothesized that most psychiatric disorders are a result of the chance convergence of polygenic defects and that the presence of tics is physical evidence that the threshold of inherited genetic deficits capable of producing psychiatric symptoms has been crossed (
1,
55). In the case of children with comorbid schizophrenia, PDD, and Tourette's disorder, the genetic loading is hypothesized to be particularly heavy (
1). These considerations, combined with the observation that the array of psychiatric disturbances among people with Tourette's disorder and their relatives is similar to the array among relatives of patients with PDD in this study and in other studies, provide support for the theory that the genetic defects underlying Tourette's disorder and its associated psychiatric disorders contribute to the pathogenesis of some cases of schizophrenia among children and adolescents (
1,
24,
25,
26,
27,
42,
54,
55).
Finally, the rate of PDD in this sample is 14 times greater than a recent population prevalence estimate, which supports anecdotal evidence among clinicians that referrals of children with PDD are rising (
1,
12,
13,
14). The results of this study cannot answer the question of whether the apparent increase in cases of autism-spectrum disorders is real or a result of better recognition and diagnosis. However, it is of interest that the rate of neuropsychiatric disorders that are thought to be genetically related to PDD also seem to be increasing (
14).
The generalizability of these findings is limited in that the study was confined to one psychiatric center. Standardized instruments were not used to validate the diagnoses of PDD, and interrater reliability was not conducted for data extraction from the clinical charts.