Racial and ethnic disparities in health care have been described across a wide spectrum of health services. Being a member of an ethnic or racial minority group appears to be a risk factor for receiving less comprehensive care. This effect has been documented for services ranging from prenatal care to treatment of cancer (
1). In the mental health field, ethnic disparities in access to insurance, use of mental health services, access to specialists, and adherence to guidelines have been described (
2).
Ethnic disparities in antipsychotic prescribing practices have also been documented. For example, despite evidence that a higher proportion of African Americans than Caucasians are slow metabolizers of antipsychotics, studies have shown that African Americans receive higher doses of antipsychotics (
2). These prescribing practices may be related to the higher risks of extrapyramidal symptoms and tardive dyskinesia that have been reported among African Americans (
2,
3).
The advent of atypical antipsychotics has led to new questions about disparities in mental health care. Three recent studies reported significant disparities in the use of atypical antipsychotics by race or ethnicity; in these studies, lower proportions of patients from minority groups received atypical agents (
4,
5,
6). Recent expert consensus opinion has suggested that preferred-practice recommendations include the use of atypical antipsychotics (
7).
We therefore conducted this study to determine whether there were ethnic disparities in the use of atypical antipsychotics at our community mental health center in New Haven, Connecticut. We intended to use these data as part of a performance improvement program in support of best clinical practices at the center.
Methods
We report on a convenience sample of 501 outpatients being treated with antipsychotic medication at the community mental health center. Of the 501 patients, 490 were identified between November 2000 and January 2002 through their participation in baseline screening for an ongoing epidemiology study of tardive dyskinesia. The additional 11 patients were identified between May 2001 and January 2002 through their participation in an ongoing study of adherence to psychotropic medications among Hispanic patients. Patients who were currently being treated with antipsychotic medication were accepted into the studies regardless of diagnosis or other possible exclusionary criteria. The participants in these ongoing studies represent about 40 percent of approximately 1,200 patients being treated with antipsychotic medication at the mental health center. All participants provided voluntary informed consent in accordance with Yale Human Investigation Committee protocol numbers 10731 and 10749. Only a few patients have declined to participate. The principal reason for nonparticipation thus far has been that research staff have not yet contacted patients to seek consent.
In both studies, an interviewer recorded demographic and treatment data by direct patient interview. Race or ethnicity was determined by patient self-report. Patients who identified themselves as Hispanic were not asked to self-identify their racial background. Other data recorded included age, gender, number of years of education, principal diagnosis, and comorbid current alcohol or substance abuse or dependence. For the 490 patients in the tardive dyskinesia study, diagnoses were established on the basis of the Structured Interview for DSM-IV. Clinical diagnoses were used for the 11 Hispanic patients in the other study.
In the univariate analyses, the chi square test was used for categorical variables, and analysis of variance was used for continuous variables. When more than two groups were being compared, an omnibus test was performed first, followed by pairwise post hoc testing when the p value for the omnibus test was less than .05. Multivariate analyses used logistic regression with any atypical antipsychotic versus only conventional antipsychotics as the dependent measure and the independent measures entered as a block. Results were considered statistically significant when p values were less than .05.
Results
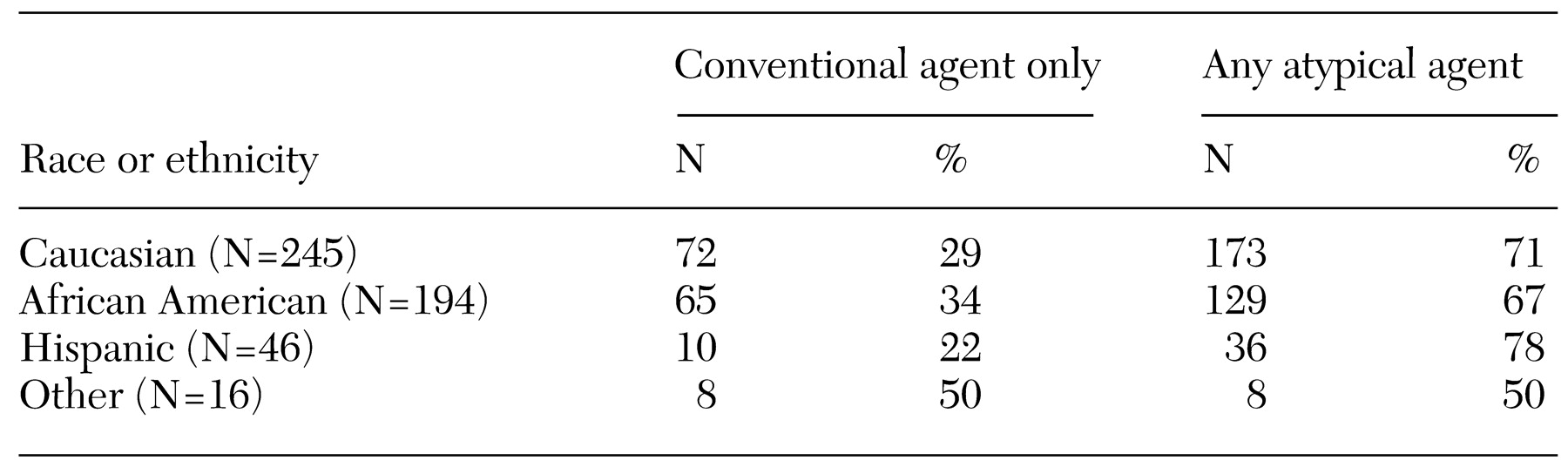
The patients' mean±SD age was 43.7±10.6 years, and 46 percent of the patients were women. The mean number of years of education in the sample was 11.7±2.5. A total of 245 patients (49 percent) were Caucasian, 194 (38 percent) were African American, 46 (9 percent) were Hispanic, and 16 (3 percent) had other racial or ethnic backgrounds (
Table 1). Patients included in the "other" category identified themselves as Asian (one patient), Native American (eight patients), and of mixed race (seven patients).
Principal diagnoses were schizophrenic and other nonaffective psychoses (380 patients, or 76 percent), affective disorders (105 patients, or 21 percent), and personality and other disorders (16 patients, or 3 percent); 84 patients (17 percent) met criteria for current alcohol or substance abuse or dependence. In the univariate analyses, significant associations with race or ethnicity were observed for age (Caucasians were older and African Americans younger), years of education (Caucasians had more years of education), and principal diagnosis (African Americans were more likely to have schizophrenia and less likely to have an affective disorder).
For 155 patients (31 percent), only conventional antipsychotics were prescribed; 346 patients (69 percent) received atypical antipsychotic medications. The distribution of type of antipsychotic medication by racial or ethnic category is shown in
Table 1. The result of the overall 2 × 4 chi square test was not statistically significant. To explore possible ethnicity effects more fully, post hoc testing was performed despite the nonsignificant omnibus test. None of the six post hoc 2 × 2 chi square tests yielded statistically significant results. In addition, the proportion of African-American versus non-African-American patients who received an atypical antipsychotic was not significantly different (67 percent compared with 71 percent).
Significant univariate associations with medication type were observed for age (younger patients were more likely to receive an atypical agent), number of years of education (patients with more years of education were more likely to receive an atypical agent), and substance abuse diagnosis (patients with dual diagnoses were less likely to receive an atypical agent). In multivariate logistic regression that included all predictors, significant and independent predictors of medication type included age (younger patients were more likely to receive an atypical agent, p<.001), number of years of education (patients with more years of education were more likely to receive an atypical agent, p=.034), and current alcohol or substance abuse or dependence (patients with dual diagnoses were more likely to receive an atypical agent, p=.043). African-American ethnicity, principal diagnosis, and gender were not significant predictors. The adjusted odds ratio (OR) for African-American versus non-African-American ethnicity was .725 (95 percent confidence interval [CI]=.480 to 1.096). The adjusted percentage of patients for whom any atypical antipsychotic was prescribed was 65 percent for African Americans and 72 percent for non-African-Americans.
Among the 347 patients who received an atypical antipsychotic, 22 (6 percent) received more than one atypical agent simultaneously and 74 (21 percent) received a conventional antipsychotic in combination with an atypical agent. There was no significant association between racial or ethnic group and antipsychotic medication in combination prescribing patterns. Among 254 patients who received only a single atypical antipsychotic, the proportions by medication were olanzapine, 53 percent (134 patients); risperidone, 24 percent (62 patients); clozapine, 17 percent (44 patients); and quetiapine, 6 percent (14 patients). None of the patients received a prescription for ziprasidone. No significant association was found between racial or ethnic group and type of atypical antipsychotic prescribed.
Depot conventional antipsychotics were prescribed for 69 patients (14 percent). The overall 2 × 4 chi square test indicated a significant association between race or ethnicity and prescription of a depot antipsychotic (χ2=10.83, df=3, p=.013). Pairwise post hoc testing showed that African Americans received depot medication more frequently than did non- African Americans (39 patients, or 20 percent, compared with 30 patients, or 10 percent; χ2=9.83, df=1, p=.002, crude OR=2.32, CI=1.35 to 4.01). In multivariate logistic regression that included all predictors, significant and independent predictors of medication type included African-American versus non-African-American ethnicity (African Americans were more likely to receive depot antipsychotics, p=.01) but not age, number of years of education, current alcohol or substance abuse or dependence, or diagnosis. The adjusted OR for African-American versus non-African-American ethnicity was 2.00 (CI=1.18 to 3.41).
Discussion and conclusions
The main finding of this study was that there were no significant racial or ethnic disparities in the prescription of atypical antipsychotics at our community mental health center. This finding was true for each minority group, including African Americans. Although the samples of Hispanics and other minorities were small, Hispanic patients had, if anything, a greater use of atypical agents than Caucasian patients. Race or ethnicity was not significantly associated with the prescription of antipsychotics in combination but was associated with use of depot medications.
It is not clear why our findings differed from those of previous studies on the use of atypical antipsychotics. The three previous studies that reported significantly lower rates of use of atypical antipsychotic medications among minority groups (
4,
5,
6) were all conducted in veteran populations, which traditionally comprise primarily male and somewhat older patients. However, demographic differences do not seem to account for the difference in results, because we found no effect of gender in our study, and when we adjusted for age there was still no significant effect of ethnicity.
Another possible explanation for the difference in results could relate to the time the studies were conducted. The three previous studies were conducted earlier in the atypical antipsychotic era than ours. The overall proportions of patients who received atypical antipsychotics increased steadily from one study to the next (32 percent, 47 percent, 59 percent, and 69 percent, respectively). The OR for comparisons between ethnic minority and white groups generally increased as well (.509, .568, .869, and .725, respectively), although these results must be interpreted carefully, because the ethnicity contrasts were structured and adjusted differently. It is possible that ethnic disparities in the use of a new and more expensive technology become less pronounced as the new technology becomes more generally available (
6).
The main limitation of our study was the size of the sample. This limitation is underscored by comparison of our sample with the much larger Department of Veterans Affairs national outpatient sample, in which the difference in the use of atypical antipsychotics across ethnicities was smaller than the one we found but nonetheless statistically significant. On the other hand, considerations of statistical significance aside, the degree of ethnic disparity that we observed may not be large enough to be considered a striking inequity.
Our data on medication use do not speak directly to issues of access. It is possible that patients could be offered new medications at equivalent rates—that is, have equal access—but decline the offer, leading to lower use. New medications can sometimes be viewed as risky or even experimental. To study access rather than use, we would have needed to determine whether patients were offered atypical antipsychotics.
Since the 1985 publication of an analysis of racial or ethnic disparities in the use of depot medications at our community mental health center (
8), the proportion of African Americans among patients treated with antipsychotics has increased from 22 percent to 39 percent, and the use of depot medications has decreased from 20 percent to 14 percent. Despite these developments, the higher use of depot medications among African Americans than among Caucasians has changed little since the 1985 study (adjusted OR=2.0 and 2.2, respectively). Unlike the use of atypical agents, the use of depot medications thus reveals a continuing disparity in care among ethnic or racial groups at our community mental health center. To some extent, this disparity has become less important as the use of depot medications has declined. However, as part of our performance improvement goals directed toward implementing best practices, we plan to monitor this issue closely if depot preparations of atypical antipsychotics become available that could lead to another increase in the use of depot medications.
Because our data did not suggest significant racial or ethnic disparities in the use of atypical antipsychotics at our community mental health center, our performance improvement goals will turn to other issues. Our study demonstrated how clinical research can combine with quality assurance and performance improvement efforts to contribute to an understanding about best practices.
Acknowledgments
This study was supported by U.S. Public Health Service grant R01-MH-61008 to Dr. Woods, grant K08-MH-01912 to Dr. Diaz, and grant K08-MH-01718 to Dr. Baker.