Aggression in inpatient mental health units is a continuing problem that affects staff physically and emotionally (
1,
2) and is a principal cause of injury (
3). Contributing factors associated with aggression include environmental factors (
4,
5), negative interactions (
5,
6,
7), situational factors (
6), power issues (
5,
8,
9,
10), and patients' symptoms (
4,
10). Perceived ways of reducing aggression include improving security (
10,
11), increasing the number of staff (
6,
11), improving staff interpersonal skills, modifying the environment, enforcing legal penalties, improving staff training (
6), making stricter unit rules, and increasing medication (
11). Because of the emotional impact of aggression (
1,
2), debriefing after incidents of aggression has been recommended for staff and patients (
4,
10).
Limitations of previous studies have included neglecting verbal forms of aggression, using retrospective research designs, neglecting either staff or patient viewpoints (
5,
6,
12), obtaining results that are tentative and suggestive only (
9), and using diagnostically homogeneous samples. Only one study has examined patients' perceptions of staff care (
13), and none has investigated staff fear and staff perceptions of management of aggression.
To overcome these limitations, this prospective study included a population-based sample; a standardized, audited recording of witnesses' accounts of verbal and physical aggressive incidents; and interviews of staff and patients that investigated the emotions they had experienced and their perceptions of causes of the aggression, the current management of it, and ways of reducing it.
Methods
Procedures
The study was conducted on all four inpatient psychiatric units in the Illawarra region south of Sydney, Australia, covering a catchment area of 225,000 people. Approximately 282 patients were admitted to one of the units from October 1999 through January 2000, and 100 consecutive incidents of aggression were identified during this four-month period. The study was approved by the hospital's institutional ethics committee.
After written informed consent was obtained, one staff member—either the victim of the aggressive incident or a witness to it—was interviewed for each incident. Staff were interviewed within one week of the incident (mean, 4.10 days; median, three days; range, one to seven days), and patients were interviewed within three weeks of the incident (mean, 6.64 days; median, five days; range, one to 21 days). Patients were interviewed only if they were sufficiently stable and capable of giving written informed consent. Only one patient was interviewed per incident.
For five of the 100 incidents, staff refused to be interviewed, resulting in staff interviews for 95 incidents. In addition, for 48 incidents, no patient interview was conducted. Reasons were refusal (20 incidents), discharge (12 incidents), no memory of the incident (11 incidents), denial of aggression (four incidents), and not wanting to be liable (one incident). Thus the final sample was 47 aggressive incidents with paired patient and staff interviews and 53 incidents without paired interviews. Persons involved in the 47 incidents totaled 29 staff and 29 patients. On average, each person was interviewed concerning one aggressive incident (range, one to four).
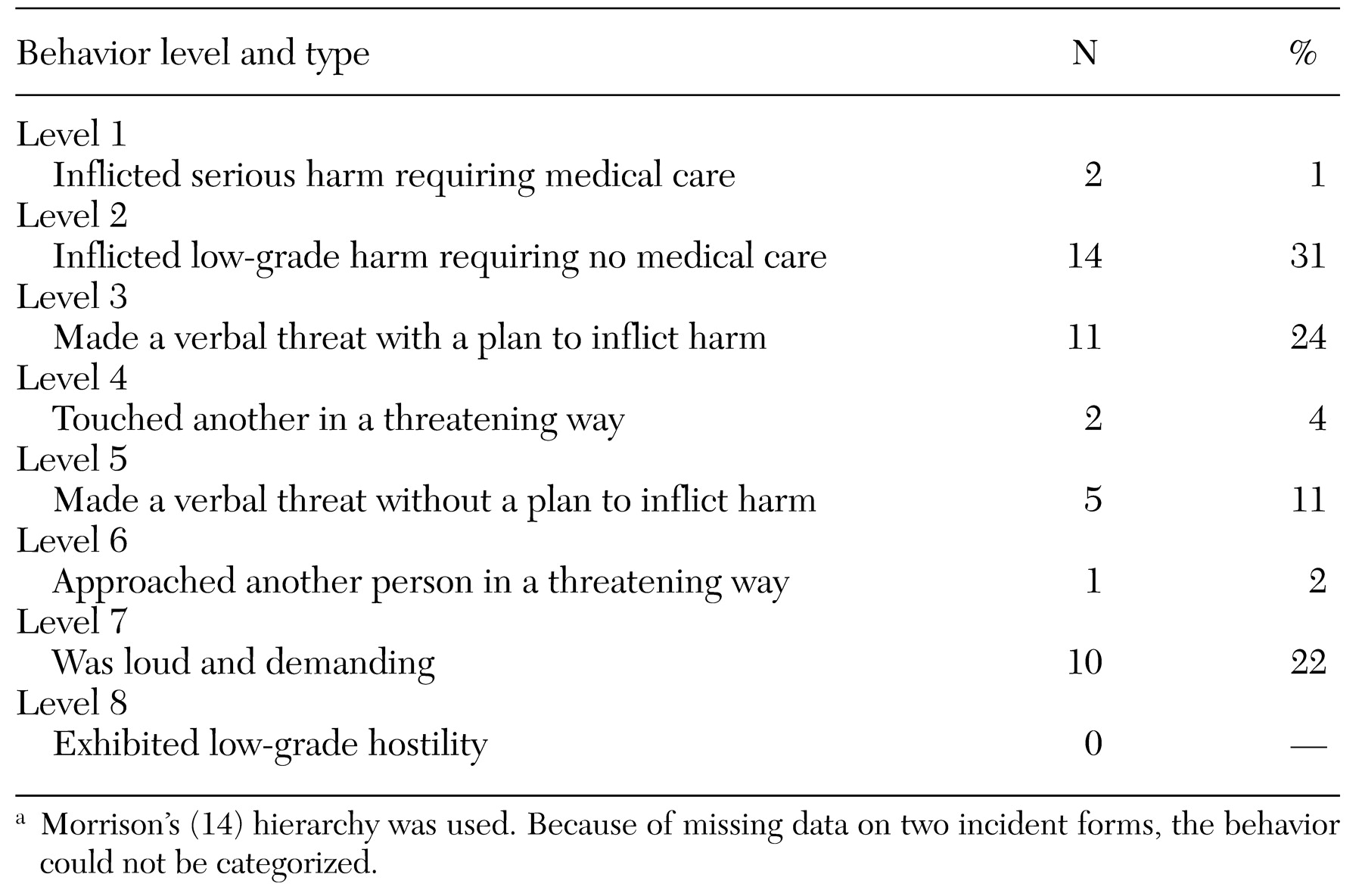
Morrison's hierarchy of aggressive and violent behaviors (
14) was used to score the 47 incidents in the study sample. Possible scores range from 1 to 8, with higher scores indicating minor aggressive behavior—for example, exhibiting low-grade hostility. The mean±SD aggression score was 5.16±2.03. The mean score for the 53 incidents not in the study sample was 4.96±1.93. The difference in scores was not significant. This finding suggests that the 47 incidents were representative of all 100 incidents.
Participants
Staff participants included 29 persons—15 men and 14 women. Their mean age was 33.02±9.2 years (range, 21 to 50 years). The sample included one nurse manager, one clinical nurse specialist, 22 registered nurses, three enrolled nurses, and two ward security staff. The length of time the staff participants had worked in psychiatry ranged from seven months to 25 years (mean duration, 5.61±5.99 years). Patient participants included 29 persons—19 men and ten women. Their mean age was 30.51±9.3 years (range, 19 to 64 years). Diagnoses were bipolar disorder (13 patients), schizophrenia (12 patients), another psychotic disorder (three patients), and adjustment disorder (one patient).
Measures
Aggressive/Assaultive Incident Form. The Aggressive/Assaultive Incident Form (
15) is completed by staff immediately following any aggressive incident. Aggression is defined as any act of verbal or physical aggression directed toward self or others, irrespective of outcome. Data recorded include the patient's demographic characteristics; the severity of the aggressive behavior, rated by Morrison's hierarchy (
14); and the interventions used, as described in the Overt Aggression Scale (
16).
Patient and staff interviews. Patients and staff were interviewed with comparable semistructured face-to-face interview schedules. The interviews were conducted by researchers who were not affiliated with the psychiatric facility, which helped to generate unbiased responses.
Patients and staff were asked about their feelings, what they thought caused the incident, how they thought similar kinds of incidents could be avoided in future, and whether they had been given the opportunity to debrief. Staff also made Likert-type ratings of how fearful they were during the incident—from 0, no fear, to 5, created extreme fear or anxiety; and how well the incident was managed in general, rather than personally—from 1, room for improvement, to 10, perfectly managed. Responses to interviews were recorded verbatim, and the transcripts were analyzed with a phenomenological "bracketing" of the researcher's expectations (
17). The two researchers separately determined the meaning of each significant statement, then compared their interpretations to determine when a statement could be interpreted in another way.
The significant statements were organized into themes expressed by both patients and staff. To check the validity and the meanings of the themes, they were discussed with some of the participants. Chi square analyses were used to identify differences between proportions of patient and staff responses; significance was set at .05.
Results
Characteristics of aggression by incident
Of the 47 incidents of aggression studied, 18 (38 percent) involved primarily physical aggression, 27 (58 percent) involved primarily verbal aggression only, and two (4 percent) involved behavior by patients that staff viewed as potentially aggressive.
In 45 incidents, aggression was directed at staff in 23 incidents (51 percent), at objects in 12 (27 percent), at other patients in nine (20 percent), and at self in one (2 percent).
Table 1 shows the frequencies of patients' specific aggressive behaviors, based on Morrison's hierarchy of aggressive and violent behaviors (
14).
In 44 incidents, information on types of interventions used by staff was obtained. The interventions included giving additional oral medication in 14 incidents (32 percent), putting the patient in seclusion in 12 (27 percent), isolating the patient (giving "time out") in six (14 percent), giving the patient an intramuscular injection in five (11 percent), restraining the patient in four (9 percent), and talking to the patient in three (7 percent).
Causes of aggressive incidents
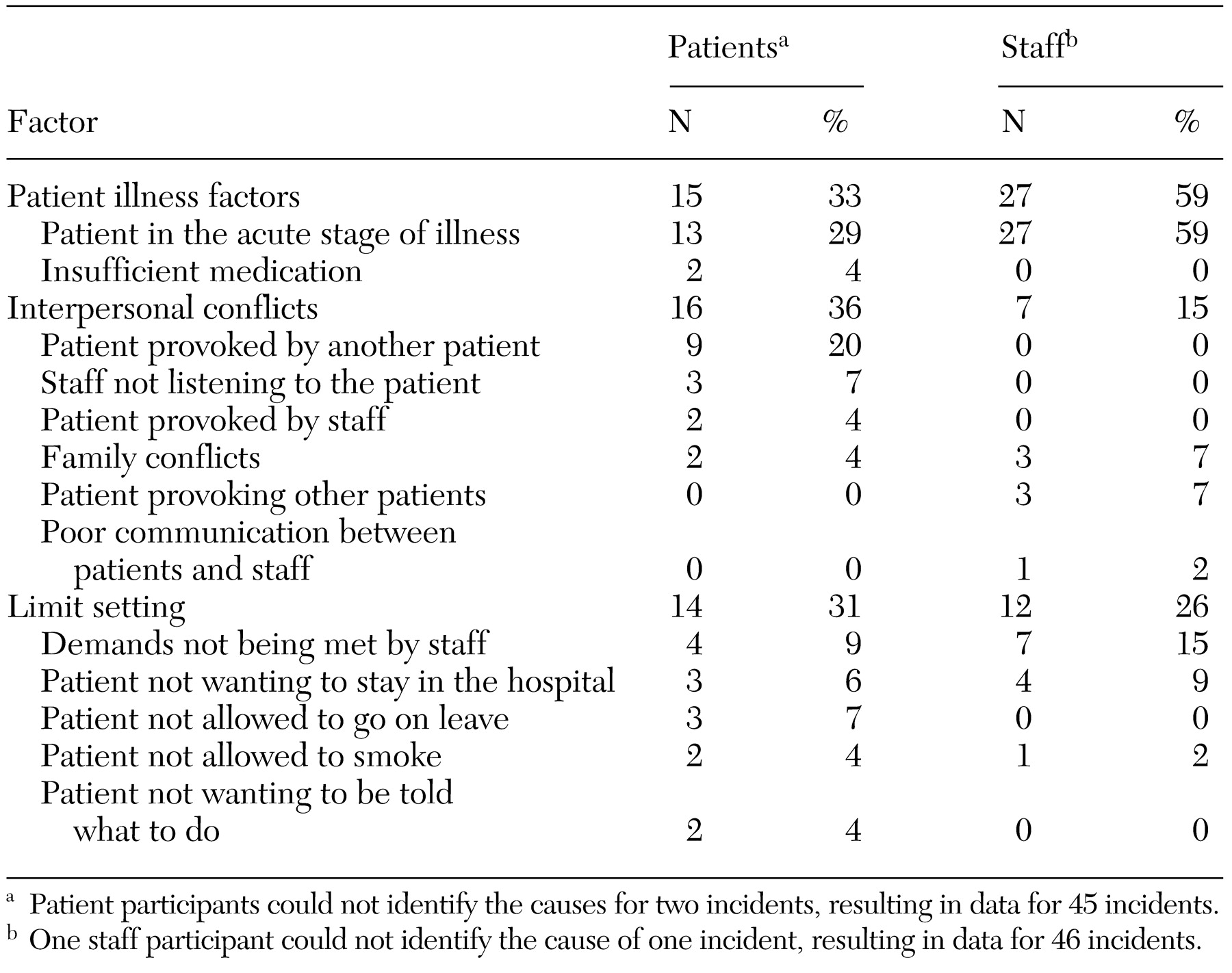
Content analysis of all verbatim responses by patients (responses for 45 incidents) and staff (responses for 46 incidents) about the causes of the aggressive incidents revealed three main causes, as shown in
Table 2: those attributable to the patient's illness, such as delusions; interpersonal conflicts, such as poor communication between patients and staff; and limit setting, such as being prevented from leaving the hospital. Patient and staff perceptions of the causes of aggression were significantly different from each other when compared across these three main factors (χ
2=7.09, df=2, p=.03). Patients viewed illness factors as the cause of aggressive incidents much less often than did staff. Patients more often saw interpersonal conflicts as the cause of aggression, and patients and staff almost equally reported limit setting as a cause of aggression.
Views on decreasing aggression
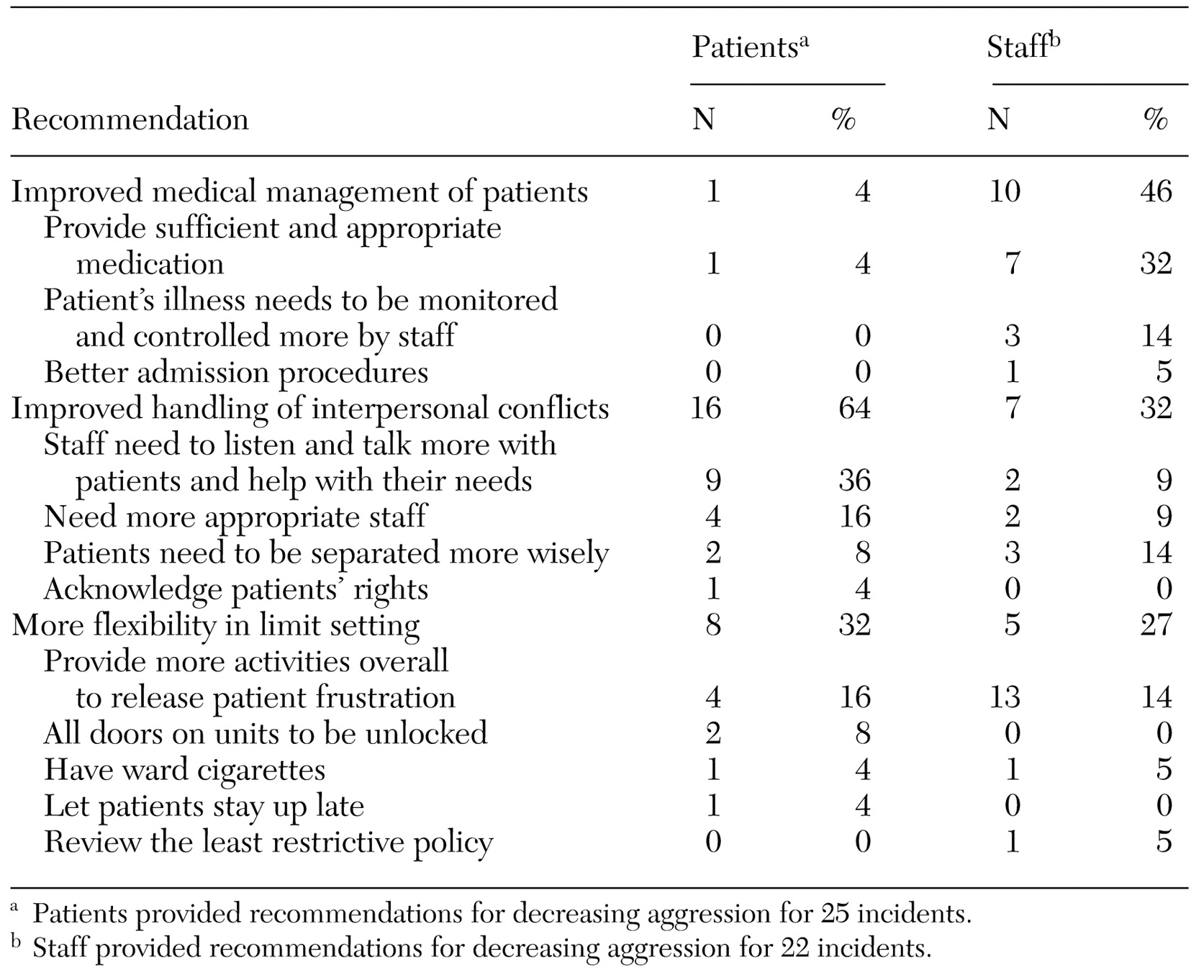
Content analysis of all verbatim responses by patients and staff about the means of reducing aggressive incidents revealed three main factors, as shown in
Table 3: those related to improving the medical management of the patient, such as providing sufficient medication; those related to better handling of interpersonal conflicts, such as inadequate communication; and those related to more flexible limit setting, such as providing more ward activities. Only about half of the patients and staff recommended ways of reducing aggression, despite prompting at the interviews. Patients' and staff's recommendations were significantly different from each other when compared across the three main factors (χ
2=11.4, df=2, p= .003). More staff than patients suggested improving medical management as a means of reducing aggression, and more patients than staff made suggestions related to decreasing interpersonal conflicts. There was a small and nonsignificant difference between the groups in recommendations related to limit setting.
Emotional reactions and postincident behaviors
Patients reported having negative emotions before 28 of 47 aggressive incidents (59.5 percent), including anger, anxiety, and depression. In contrast, staff reported negative emotional reactions before 16 of 47 aggressive incidents (34 percent)—most commonly, anger and anxiety.
Patients' aggressive behavior rated by Morrison's hierarchy of aggressive and violent behaviors (
14) was categorized by the level of aggressive behavior: physical (levels 1, 2, and 4) or verbal (levels 3, 5, 6, and 7). No association was found between the type of aggression displayed and whether the patient experienced a negative emotion before the incident. Furthermore, no association was found between the type of aggression displayed and whether staff experienced a negative emotion after the incidents.
Staff rated the level of fear and anxiety evoked during the aggressive incidents. The average fear rating on the scale of 0 to 5 was low (1.49±.66, range, 0 to 3). Of the incidents that evoked fear and anxiety among staff, 12 (52 percent) involved aggression against staff, and eight (36 percent) involved aggression against others.
Staff were moderately satisfied with the way the aggressive incidents were managed; the staff mean rating on the scale of 1 to 10 was 6.7±2.53. There was no relationship between this rating and staff age, years of psychiatry experience, or the level of fear evoked by the incident. Patients were generally satisfied with the way the aggressive incidents were managed; only 11 patients (24 percent) were dissatisfied. Of these 11, seven wanted staff to listen more, spend more time with them, and negotiate more concerning conflicts; three wanted staff to be calmer when dealing with aggressive incidents; and one wanted staff to spend more time explaining and encouraging medication adherence and to explain the consequences of noncompliance with medication.
More staff than patients reported that they had spoken to someone about the aggressive incident. For 30 of 47 incidents (64 percent), staff had spoken to a colleague or had had a formal debriefing session. In contrast, for only 11 of 47 incidents (23.4 percent) did patients report being given an opportunity to speak with, and speaking with, a staff member, a friend, or another patient. No patient reported a formal defusing or debriefing session.
Discussion
This study found significant differences between patient and staff perceptions of the causes of aggressive incidents on inpatient psychiatric units and of the ways to reduce them. Staff emphasized medication and medical management in both the causes of aggression and ways to reduce it. Patients emphasized equally the roles of interpersonal conflict, limit setting, and their illness in the cause of incidents, and they emphasized the need for better communication in incident management. Most patients and staff members were satisfied with how the incident was managed, although many more staff than patients were given an opportunity to discuss the aggressive incident.
Previous studies have also found that staff and patients stated different reasons for aggression (
6,
10,
12,
18). Staff in some studies attributed aggression to the stage of illness (
4,
10,
18,
19)—a finding similar to ours, in which staff emphasized medication management. Although patients in this study were generally satisfied with the way the aggressive incidents were managed, they did seek a more interpersonal approach from staff. According to the interviews, more than half of the patients (60 percent) reported experiencing negative emotions before the aggression. Thus it appears that negative emotions increase the risk of aggression.
Other studies have found that being sensitive to the patient's mental state, encouraging expression of feelings (
5), and helping the patient break the incident down into components (
20) can facilitate alternative, nonaggressive responses. Debriefing can assist staff in dealing with self-doubts about the management of incidents (
4) and can help deal with the emotional effects of being a witness to or a victim of aggression (
21). Although it might be expected that witnessing or being a victim of physical aggression would lead to more negative emotional effects among staff than witnessing or being a victim of verbal aggression, this was not found to be true, indicating that verbal aggression can be as distressing to staff as physical aggression.
This study had certain limitations: The results are based on a small sample size; therefore, the views expressed may not be representative of the views of patients generally. The open-ended style of interviewing meant that articulate patients contributed more to the data set than did less articulate patients.
Conclusions
The findings of this study suggested that patients and staff perceive aggression on inpatient mental health units differently. Supervision and training should highlight the need for staff to understand and take into account patients' perspectives. Future research needs to address patients' perceptions of the management of aggression following aggression management training for staff that incorporates the issues highlighted from this study.